Abstract
Study design:
Cohort Study (Prospective Observational Study).
Objectives:
The objectives of the study were (i) to examine left ventricular (LV) diastolic function at rest and during rapid saline infusion in those with spinal cord injury (SCI) and (ii) to determine the contribution of blood volume on the purported diastolic impairments in individuals with SCI.
Settings:
St Catharines, ON, Canada.
Methods:
Thirteen SCI (AIS:A-D; C4–T6; age: 41±8.5; 10 males, 3 females) and 12 able-bodied (AB) individuals (age: 40±8.5; 9 males, 3 females) without a history of cardiovascular disease participated in the study. LV structure and diastolic function were assessed via conventional echocardiography. The carbon monoxide rebreathe test was used to measure the blood volume. LV diastolic function was assessed once more following rapid saline infusion (dose: 15 ml kg−1; rate: 100 ml min−1).
Results:
Compared with the AB group, individuals with SCI had a smaller LV internal diameter (SCI: 4.5±0.3 cm vs AB: 5.1±0.7 cm; P=0.01), lower blood volume (SCI: 3.9±0.6 l vs AB: 5.0±1.2 l; P=0.02) and end-diastolic volume (SCI: 97.2±29.4 ml vs AB: 128.6±38.3 ml; P=0.03). There were no between-group differences in baseline diastolic parameters; however, when LV internal diameter was adjusted for individuals with SCI demonstrated lower early to late transmitral velocity ratio (SCI: 1.9±0.5 vs AB: 2.2±0.7; P=0.03). There was no between-group difference in diastolic responses to the saline infusion, as both groups showed similar diastolic changes following volume loading.
Conclusion:
Individuals with SCI have preserved LV diastolic function despite having lower preload. Preserved diastolic function may be mediated by the cardiac atrophy that occurs following SCI. Individuals with SCI also demonstrate normal diastolic responses to increased volume loading, suggesting compliant ventricles.
Similar content being viewed by others
Introduction
Individuals with spinal cord injury (SCI) represent one of the most physically inactive populations because of their profound immobility. Accordingly, such immobility results in an elevated risk of a wide array of cardiovascular complications, including coronary artery disease,1 peripheral artery disease,2 atherosclerosis3 and accelerated cardiovascular aging.4 Although severe physical inactivity has been shown to be associated with impaired diastolic function in able-bodied individuals,5, 6, 7 findings regarding diastolic function after SCI remain equivocal. Left ventricular diastolic function has been shown by some to be preserved in those with SCI,8, 9, 10 whereas more recent reports convey diastolic impairments after SCI.11, 12, 13, 14 Therefore, it is unknown whether diastolic dysfunction actually manifests after SCI.
It is important to note that echocardiographic parameters of diastolic function are highly influenced by preload. Specifically, an increase in preload augments diastolic values whereas a decrease in preload reduces them.15, 16, 17, 18 Individuals with SCI demonstrate reduced ventricular filling and preload, partly due to a reduction in blood volume secondary to the chronic physical inactivity.19 Therefore, it is not clear whether the reported diastolic impairments following SCI are a result of reduced blood volume or due to pathological alterations in the left ventricle, per se. In addition, diastolic function in individuals with SCI has always been examined while participants were in a relaxed state, and therefore it is unclear how ventricular filling after SCI functions when the heart is exposed to stress. Rapid saline infusion is a diagnostic method that increases preload, and may reveal left ventricular impairments that may otherwise not manifest during resting conditions.20 In addition, the normal diastolic responses to rapid saline infusion are well documented,17, 18 and therefore this method may be a useful tool to elucidate any left ventricular diastolic impairments in individuals with SCI.
Accordingly, the purpose of this study was to determine whether individuals with SCI demonstrate diastolic impairments at rest and/or during a volume stress induced by rapid saline infusion. We also aimed to determine whether reduction in blood volume following SCI contributes to the putative diastolic impairments in this population.
Materials and methods
Participants
Thirteen individuals with SCI (C4–T6; AIS A-D; 16.5±9.7 years post injury) and 12 able-bodied individuals matched for age, sex and body mass participated in this study. Participants were nonsmokers, nonhypertensive, did not have history of heart disease and had a normal resting and exercise electrocardiogram. As this is the first study to perform rapid saline infusion in individuals with SCI, those with unstable autonomic dysreflexia were excluded. Participants from both groups included a range of sedentary to physically active individuals but none were competitive or highly trained athletes. Individuals with SCI were recruited from an outpatient community-based exercise center for SCI and other neuromuscular conditions (Power Cord, St Catharines, ON, USA). All the participants provided informed consent to participate in the study, and we certify that all applicable institutional regulations concerning the ethical use of human volunteers were followed during the course of this research.
General study protocol
All participants were required to void their bladder before testing, especially those with SCI to reduce any risk of autonomic dysreflexia. After a 15 min resting period in the left lateral decubitus position, resting blood pressure was obtained manually from the brachial artery, and a continuous electrocardiogram recording (lead II) was taken throughout the testing session. Following the resting period, assessment of left ventricular structure and function was performed via two-dimensional and M-mode echocardiography. Participants then performed the carbon monoxide rebreathe test for the measurement of total blood volume. This was followed by rapid saline infusion. After 5 min of the saline infusion, left ventricular diastolic function was assessed once more.
Echocardiography
All echocardiographic images were obtained using a commercially available ultrasound system (Vivid 7; GE Vingmed Ultrasound AS, Horten, Norway) with a 1.5 MHz phased-array transducer. All images were acquired by a single experienced sonographer and were stored for later offline analysis using a commercially available software (EchoPac version 6.0; GE Vingmed Ultrasound AS). Images were obtained while participants were in the left lateral decubitus position at end expiration and three consecutive cycles for each image were stored and averaged for offline analysis.
Left ventricular wall dimensions were assessed at end diastole and end systole via M-mode recordings (and values were confirmed by two-dimensional recordings) in accordance to the recommendations of the American Society of Echocardiography.21 Left ventricular wall dimensions included intraventricular septal thickness at diastole and systole, posterior left ventricular internal diameter at diastole (LVIDd) and systole (LVIDs) as well as posterior wall thickness in diastole and systole. Hemodynamic measures that included end-diastolic volume, end-systolic volume, ejection fraction, as well as stroke volume were measured from the long parasternal axis view through M-mode, as apical chamber views from individuals with SCI were suboptimal for the use of Simpson’s Biplane. Cardiac output was calculated as the product of stroke volume and heart rate. Left ventricular mass (LVM) was calculated using the Devereux formula22 and was indexed for body surface area (LVMi).23
Pulsed-wave Doppler and tissue Doppler were used to assess diastolic function according to the recommendation of the American Society of Echocardiography.24 For mitral inflow velocity, from an apical four-chamber view, a 4-mm sample volume was placed between the mitral valve leaflet tips during diastole. The Doppler velocity curves were digitized to obtain peak early (E) and late (A) mitral flow velocities, and their ratio (E:A) was calculated. The descending limb of the E wave was used to measure deceleration time, and isovolumetric relaxation time was measured as the time between aortic valve closure and mitral valve opening. Mitral annular velocities were measured via tissue Doppler imaging from the four-chamber apical view. A 2-mm sample volume was placed along the longitudinal movement of the basal septal and basal lateral walls. Peak early (E′) and late (A′) diastolic myocardial tissue velocities were recorded, and E:E′ was calculated as a noninvasive measure of left ventricular filling pressure.25
Carbon monoxide rebreathe test
The carbon monoxide rebreathe test was used for the assessment of total blood volume in accordance to the Burge and Skinner method.26 Briefly, a 20-gauge catheter was placed in the antecubital vein for instant blood draws. A baseline blood sample was taken for measurement of hematocrit. After a 4 min period of breathing 100% oxygen (Praxair, Hamilton, ON, Canada), participants inhaled a 15–20 ml priming dose of 100% CO gas (Praxair) and a 1 ml blood sample was obtained in a heparinized vacutainer for assessment of carboxy-hemoglobin and total hemoglobin. A second dose of carbon monoxide gas (40–50 ml) was inhaled, and after 10 min of breathing, a final blood sample was obtained for carboxy-hemoglobin assessment. All blood samples were analyzed by a blood–gas analyzer via photospectromery (Phox-Cooximeter; NovaBiomedical, Mississauga, ON, Canada). The carbon monoxide rebreathe test yields a low reproducibility error in both able-bodied27 and SCI individuals,19 and total blood volume was reported in absolute values and indexed for body mass.
Volume loading
Preload was increased via rapid infusion of warm isotonic saline (0.9% NaCl) through the antecubital vein by an 18–20-gauge catheter. The saline dose consisted of 15 ml kg−1 at a rate of 100 ml min−1.
Statistical analysis
A Shapiro–Wilk test was used to check for normalcy in all parameters, and as a result, parametric statistics were justified. Unpaired t-tests were used to compare all baseline left ventricular structural, diastolic and hemodynamic parameters between groups. An analysis of covariance was used to assess differences in baseline diastolic parameters while adjusting for LVIDd. The LVIDd was used as a covariate because a reduction in left ventricular size following SCI has been proposed as a mechanism to maintain normal diastolic function despite a reduction in preload,8, 28 and LVIDd had equal regression coefficient associated with both groups (assumption of homogeneity of regression). A two-way repeated-measures analysis of variance was used to detect group by condition (IV infusion) interactions as well as main effects for diastolic parameters. Statistical analyses were performed using Microsoft Excel 2013 and Statistical Package for Social Sciences (SPSS 21.0, IBM, Chicago, IL, USA) software. Data were reported as means±s.d., and the level of statistical significance was set at P⩽0.05.
Results
Participants
All participant characteristics are provided in Table 1. There were no between-group differences in age, height, body mass, heart rate or blood pressure (able-bodied: 105±13 mm Hg vs SCI: 101±16 mm Hg; P>0.05). All participants tolerated the rapid saline infusion well, and no adverse events occurred.
Baseline left ventricular structure and hemodynamics
Compared with able-bodied participants, individuals with SCI exhibited cardiac atrophy as evidenced by smaller LVIDd. In addition, the SCI group demonstrated lower end-diastolic volume, stroke volume and cardiac output; however, ejection fraction was not different between groups (Table 2). There were no between-group differences in LVM, LVMi or any of the other structural parameters. Absolute total blood volume and blood volume indexed for body mass were significantly lower in the SCI group (Table 2). In addition, there were no between-group differences in any of the diastolic parameters (Table 3); however, after controlling for LVIDd, the SCI group demonstrated a significantly lower E:A ratio (Table 3).
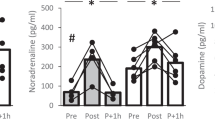
Diastolic response to rapid saline infusion
There was no difference in the average amount of saline given to both groups (SCI: 1184±214 ml vs able-bodied: 1208±252 ml; P=0.80). There were no group by condition interactions for any of the diastolic measures (P>0.05), suggesting that both groups responded similarly to the rapid saline infusion. However, there was a significant main effect for condition, specifically when collapsing across groups, the saline infusion resulted in a significant increase in E (0.78±0.10 m s−1 to 0.90±0.11 m s−1; P<0.01; Figure 1a) and the E:A ratio (2.06±0.61 to 2.82±1.05; P<001; Figure 1b), as well as a significant decrease in A (0.40±0.09 m s−1 to 0.35±0.11 m s−1; P=0.05; Figure 1c), deceleration time (208.37±50.04 ms to 183.16±37.21ms; P=0.01; Figure 1d) and isovolumetric relaxation time (102.04±17.54ms to 88.42±14.11ms; P<0.01; Figure 1e). The saline infusion also resulted in a significant increase in E′Sept (0.13±0.02 m s−1 to 0.14±0.03 m s−1; P=0.01) and E′Lat (0.15±0.04 m s−1 to 0.17±0.04 m s−1; P<0.001) velocities. Rapid saline infusion resulted in no changes in A′Sept velocity (0.09±0.02 m s−1 to 0.10±0.03; P=0.20), A′Lat velocity (0.08±0.03 m s−1 to 0.08±0.03 m s−1; P=0.40) or left ventricular filling pressure as indicated by EE′ (5.8±1.3 to 6.0±1.2; P=0.40). In addition, Table 4 shows that the percent change in diastolic values in response to the saline infusion was similar between groups.
(a) Early transmitral diastolic velocity after rapid saline infusion. (b) Ratio of early to late transmitral filling velocity after rapid saline infusion. (c) Late transmitral diastolic velocity after rapid saline infusion. (d) Transmitral deceleration time after rapid saline infusion. (e) Isovolumetric relaxation time after rapid saline infusion. A, late transmitral diastolic velocity; AB, able-bodied; DT, deceleration time; E, early transmitral diastolic velocity; E:A, early to late diastolic velocity ratio; IVRT, isovolumentric relaxation time; SCI, spinal cord injury. Error bars are s.d. * denotes significant main effect for condition (P<0.05).
Discussion
The main findings of this investigation are that (i) individuals with SCI have preserved left ventricular diastolic function at rest despite having a lower blood volume, (ii) cardiac atrophy following SCI may have a role in preserving diastolic function in response to lower preload and (iii) rapid saline infusion resulted in similar left ventricular filling patterns between spinal cord injured and able-bodied individuals.
Baseline diastolic function
The current investigation shows that individuals with SCI have preserved left ventricular diastolic function at rest. This has been corroborated by previous studies where normal diastolic function was reported in individuals with complete tetraplegia8 and paraplegia10 regardless of being sedentary9 or active.28 However, other investigators have reported reduced diastolic function following SCI.11, 12, 13, 14 It has been proposed that the chronic physical inactivity after SCI may have a role in such diastolic impairments, as active spinal cord injured individuals have been shown to present better diastolic patterns compared with sedentary ones.11, 14 However, Maggioni et al.29 reported no difference in diastolic function between trained and untrained spinal cord injured individuals and De Groot et al.8 reported no difference in diastole between able-bodied individuals and sedentary individuals with severe tetraplegia. In addition, Driussi et al.12 reported lower diastolic function in those with SCI compared with able-bodied individuals even after controlling for levels of physical activity, suggesting that physical activity did not have a major role in the diastolic impairments. It is interesting to note, however, that in two of the studies that reported diastolic impairments after SCI,12, 13 the spinal cord injured groups exhibited left ventricular concentric hypertrophy, which is a pattern often seen in individuals with diastolic heart failure.30 Therefore, these individuals may have had other concomitant disorders that resulted in unfavorable left ventricular structural alterations, which in turn caused diastolic impairments.
Diastolic function after saline infusion
This is the first study to perform rapid saline infusion in individuals with SCI. Rapid saline infusion is an excellent diagnostic method for unmasking cardiac dysfunctions that otherwise may not manifest during resting conditions. If a ventricle is compliant, then diastolic function should be augmented in response to increased loading without significant changes in left ventricular filling pressures.17, 18 In contrast, a noncompliant ventricle will demonstrate significant elevations in filling pressure after increased volume loading.20 Both groups in the current investigation demonstrated similar changes in all diastolic parameters, and both the groups showed no changes in the left ventricular filling pressures, as shown by EE′. This is evidence that the left ventricle of the current SCI cohort is compliant and does not have intrinsic pathological alterations. In addition, both groups received the same average dose of saline despite the SCI group having a smaller left ventricle. This means that the left ventricle in those with SCI likely expanded relatively more during the infusion with no significant changes in the filling pressure, which further supports the notion that left ventricular elasticity is maintained after SCI.
Positive morphological adaptation
Owing to the lower blood volume and preload (end-diastolic volume) demonstrated by the spinal cord injured group, a reduction in left ventricular diastolic function was expected. However, both groups showed similar values for all diastolic parameters. This was unexpected, as hypovolemia has been shown to reduce ventricular diastolic function5, 15 and distensibility.6, 7 However, despite the spinal cord injured participants being hypovolemic with lower preload, diastolic function was still preserved. This may be mediated by the ventricular atrophy experienced after SCI, as shown by a smaller LVIDd, which is likely a morphological adaptation to the chronic reduction in preload. A smaller chamber size may preserve diastolic velocities despite a lower preload by preserving ventricular wall stress. Although this has been hypothesized to occur after SCI,8, 28 this is the first study to show evidence of such a mechanism, as the SCI group demonstrated reduced diastolic function (lower E:A ratio) only when LVID was controlled for. It is interesting to note that the current SCI cohort did not show a reduction in LVM. This could possibly be because of the preservation of normal systolic blood pressure (afterload), which maintains a certain level of resistance to preserve LVM. This has been previously shown, as individuals with SCI who show reduced LVM also demonstrate reduced blood pressure,8, 28 whereas those who present normal LVM exhibit normal blood pressure.12 This suggests that LVID is more important than LVM in maintaining diastolic velocities during hypovolemia. Furthermore, SCI is associated with severe skeletal muscle atrophy,32 peripheral vasculature atrophy33 and a decrease in capillary density,34 all of which have a role in reduced overall oxygen demand.33, 35 As a result, the heart is not required to maintain a normal size and likely also atrophies in accordance to the muscular and vascular atrophy after paralysis. Therefore, the cardiac atrophy that occurs after SCI may be a positive morphological adaptation, which preserves normal cardiac function and allows the heart to operate in accordance to lower systemic demands.
Structural and hemodynamic findings
Although stroke volume and cardiac output were lower in the SCI group, this was likely because of the reduced preload and not because of impaired ventricular contractility, as evidenced by similar ejection fractions between the groups. Furthermore, the observed reduction in LVIDd demonstrated by the spinal cord injured participants is in agreement with several previous reports.10, 11, 12, 28 However, the commonly reported reduction in LVM in this population8, 9, 10, 28, 29 was not observed in the current participants. As mentioned, the smaller LVIDd can be explained by the chronic reduction in preload, as demonstrated by a lower end-diastolic volume and blood volume. The reduction in preload decreases ventricular mass to volume ratio, thus decreasing ventricular wall stress and consequently resulting in adaptive cardiac atrophy.36 In addition, the left ventricle is highly adaptive to changes in loading conditions, as cardiac atrophy has been shown to occur in as little as 2 weeks of reduced preload.36
The blood volume values obtained in our study are comparable to those reported by Houtman et al.,19 whose participants had a similar distribution of injury levels compared with those in the current study (C4–T6). Physical inactivity is a known stimulus for hypovolemia,6, 7, 37 thus the smaller blood volume in SCI individuals is likely because of the chronically reduced physical activity levels. However, it is interesting to note that the reduction in blood volume in response to physical inactivity is typically demonstrated from models of severe immobilization, such as bed rest31, 37 and spaceflight. The spinal cord injured individuals in the current study were not completely immobilized, as they use manual wheelchairs for their main method of transportation, they perform daily transfers and the majority of them participate in regular aerobic and resistance exercise with the upper limbs. However, although being relatively active, they still demonstrated a lower blood volume compared with the able-bodied group. This suggests that moderate upper limb activity is insufficient to maintain blood volume after SCI and perhaps lower limb exercise is required in this regard. This hypothesis is supported by an exercise study that reported no change in blood volume following 6 weeks of arm ergometry in individuals with SCI despite an increase in exercise performance.38 In contrast, Houtman et al.19 demonstrated significant elevations in blood volume in individuals with SCI following only 2 weeks of electrically stimulated leg cycling exercise.
Conclusion
Although individuals with SCI were hypovolemic, which results in reduced preload, diastolic function is still preserved at rest. The cardiac atrophy that occurs after SCI may have a role in maintaining normal diastolic function. In addition, individuals with SCI demonstrated normal ventricular filling responses to rapid saline infusion, suggesting that the left ventricle is compliant in these individuals. However, further and more invasive examination of human SCI ventricular compliance is required to confirm our results. These investigations can use methods such as pulmonary wedge capillary pressure or analysis of human myocardial tissue.
Limitations
The primary limitation to this study was the small number of participants given the difficulty of recruiting a large number of individuals with SCI. Another limitation is that we are basing our conclusion of compliant ventricles following SCI from noninvasive measures; thus, further studies using more direct measures of ventricular compliance are warranted. Finally, all individuals with SCI were grouped together due to the small sample size; therefore, larger studies are required to compare the diastolic function between different severities and levels of injuries.
DATA ARCHIVING
There were no data to deposit.
References
Bauman WA, Spungen AM . Coronary heart disease in individuals with spinal cord injury: assessment of risk factors. Spinal Cord 2008; 46: 4664–4676.
Bell JW, Chen D, Bahls M, Newcomer SC . Evidence for greater burden of peripheral arterial disease in lower extremity arteries of spinal cord-injured individuals. Am J Physiol Heart Circ Physiol 2011; 301: H766–H772.
Matos-Souza JR, Pithon KR, Ozahata TM, Oliveira RT, Téo FH, Blotta MH et al. Subclinical atherosclerosis is related to injury level but not to inflammatory parameters in spinal cord injury subjects. Spinal Cord 2010; 48: 740–744.
Wecht JM, Weir JP, DeMeersman RE, Schilero GJ, Handrakis JP, LaFountaine MF et al. Cold face test in persons with SCI: age versus inactivity. Clin Auton Res 2009; 19: 221–229.
Dorfman TA, Rosen BD, Perhonen MA, Tillery T, McColl R, Peshock RM et al. Diastolic suction is impaired by bed rest: MRI tagging studies of diastolic untwisting. J of App Physiol 2008; 104: 1037–1044.
Levine BD, Zuckerman JH, Pawelczyk JA . Cardiac atrophy after bed-rest deconditioning A nonneural mechanism for orthostatic intolerance. Circulation 1997; 96: 517–525.
Perhonen MA, Zuckerman JH, Levine BD . Deterioration of left ventricular chamber performance after bed rest ‘cardiovascular deconditioning’ or hypovolemia? Circulation 2001; 103: 1851–1857.
De Groot PC, Van Dijk A, Dijk E, Hopman MT . Preserved cardiac function after chronic spinal cord injury. Arch Phys Med Rehabil 2006; 87: 1195–2000.
Eysmann SB, Douglas PS, Katz SE, Sarkarati M, Wei JY . Left ventricular mass and diastolic filling patterns in quadriplegia and implications for effects of normal aging on the heart. Am J Cardiol 1995; 75: 201–203.
Kessler KM, Pina I, Green B, Burnett B, Laighold M, Bilsker M et al. Cardiovascular findings in quadriplegic and paraplegic patients and in normal subjects. Am J Cardiol 1986; 58: 525–530.
De Rossi G, Matos-Souza JR, Costa E, Campos LF, Santos LG, Azevedo ER et al. Physical activity and improved diastolic function in spinal cord-injured subjects. Med Sci Sports Exerc 2014; 46: 887–892.
Driussi C, Ius A, Bizzarini E, Antonini-Canterin F, d'Andrea A, Bossone E et al. Structural and functional left ventricular impairment in subjects with chronic sci and no overt cardiovascular disease. J Spinal Cord Med 2014; 37: 85–92.
Matos-Souza JR, Pithon KR, Oliveira RTD, Téo FH, Blotta MH, Cliquet A Jr et al. Altered left ventricular diastolic function in subjects with spinal cord injury. Spinal Cord 2011; 49: 65–69.
Schreiber R, Paim LR, De Rossi G, Matos-Souza JR, Costa E Silva Ade A, Souza CM et al. Matrix metalloproteinases and left ventricular function and structure in spinal cord injured subjects. Clin Chim Acta 2014; 437: 136–140.
Assa S, Hummel Y, Voors A . Changes in left ventricular diastolic function during hemodialysis sessions. Am J Kidney Dis 2013; 62: 549–556.
Borlaug BA, Melenovsky V, Redfield MM, Kessler K, Chang HJ, Abraham TP et al. Impact of arterial load and loading sequence on left ventricular tissue velocities in humans. J Am Col Cardiol 2007; 50: 1570–1577.
Firstenberg MS, Levine BD, Garcia MJ, Greenberg NL, Cardon L, Morehead AJ et al. Relationship of echocardiographic indices to pulmonary capillary wedge pressures in healthy volunteers. J Am Col Cardiol 2001; 36: 1664–1669.
Prasad A, Popovic ZB, Arbab-Zadeh A, Fu Q, Palmer D, Dijk E et al. The effects of aging and physical activity on Doppler measures of diastolic function. Am J Cardiol 2007; 99: 1629–1636.
Houtman S, Berend O, Hopman M . Blood volume and hemoglobin after spinal cord injury. Am J Phys Med Rehabil 2000; 79: 260–265.
Fujimoto N, Borlaug BA, Lewis GD, Hastings JL, Shafer KM, Bhella PS et al. Hemodynamic responses to rapid saline loading: the impact of age, sex, and heart failure. Circulation 2012; 21: 55–62.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 2005; 18: 1440–1463.
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 1986; 57: 450–458.
Du Bois D, Du Bois EF . A formula to estimate the approximate surface area if height and weight be known. 1916. Nutrition 1989; 5: 303.
Nagueh SF, Smiseth OA, Appleton CP, Byrd 3rd BF, Dokainish H, Edvardsen T et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2016; 29: 277–314.
Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM et al. Clinical utility of Doppler echocardiography and Doppler tissue imaging in the estimation of left ventricular filling pressures. Circulation 2000; 102: 1788–1794.
Burge CM, Skinner SL . Determination of hemoglobin mass and blood volume with CO: evaluation and application of a method. J App Physiol 1995; 79: 623–631.
Gore CJ, Hopkins WG, Burge CM . Errors of measurement for blood volume parameters: a meta-analysis. J Appl Physiol 2005; 99: 1745–1758.
West CR, Campbell IG, Shave RE, Romer LM . Resting cardiopulmonary function in paralympic athletes with cervical spinal cord injury. Med Sci Sports Exerc 2012; 44: 323–329.
Maggioni MA, Ferratini M, Pezzano A, Heyman JE, Agnello L, Veicsteinas A et al. Heart adaptations to long-term aerobic training in paraplegic subjects: an echocardiographic study. Spinal cord 2012; 50: 538–542.
Zile MR, Brutsaert DL . New concepts in diastolic dysfunction and diastolic heart failure: part ii causal mechanisms and treatment. Circulation 2002; 105: 1503–1508.
Carrick‐Ranson G, Hastings JL, Bhella PS, Shibata S, Levine BD . The effect of exercise training on left ventricular relaxation and diastolic suction at rest and during orthostatic stress after bed rest. Exp Physiol 2013; 98: 501–513.
Gorgey AS, Dudley GA . Skeletal muscle atrophy and increased intramuscular fat after incomplete spinal cord injury. Spinal Cord 2007; 45: 304–309.
Hopman MT, Van Asten WNJC, Oeseburg B . Changes in blood flow in the common femoral artery related to inactivity and muscle atrophy in individuals with long-standing paraplegia. Adv Exp Med Biol 1996; 388: 379–383.
Martin TP, Stein RB, Hoeppner PH, Reid DC . Influence of electrical stimulation on the morphological and metabolic properties of paralyzed muscle. J App Physiol 1992; 72: 1401–1406.
Hopman MT, Groothuis JT, Flendrie M, Gerrits KH, Houtman S . Increased vascular resistance in paralyzed legs after sci is reversible by training. J App Physiol 2002; 93: 1966–1972.
Perhonen MA, Franco F, Lane LD, Buckey JC, Blomqvist CG, Zerwekh JE et al. Cardiac atrophy after bed rest and spaceflight. J App Physiol 2001; 91: 645–653.
Fortney SM, Turner C, Steinmann L, Driscoll T, Alfrey C . Blood volume responses of men and women to bed rest. J Clin Pharm 1994; 34: 434–439.
Knutsson E, Lewenhaupt-Olsson E, Thorsen M . Physical work capacity and physical conditioning in paraplegic patients. Spinal Cord 1973; 11: 205–216.
Acknowledgements
We thank Dr Richard Hughson and Danielle Greaves for assisting with the carbon monoxide rebreathe test. We also thank Robert Kuman for helping with data collection. We also thank the Ontario Neurotrauma Foundation, Toronto, ON, Canada (Grant #2011-ONF-RHI-MT-894) for helping to fund this research. This funding source had no involvement in the preparation of this article and there is no relationship with industry.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sharif, H., Wainman, L., O'Leary, D. et al. The effect of blood volume and volume loading on left ventricular diastolic function in individuals with spinal cord injury. Spinal Cord 55, 753–758 (2017). https://doi.org/10.1038/sc.2017.30
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2017.30
This article is cited by
-
Spinal cord injury impairs cardiac function due to impaired bulbospinal sympathetic control
Nature Communications (2022)
-
Left Atrial Remodeling Mechanisms Associated with Atrial Fibrillation
Cardiovascular Engineering and Technology (2021)
-
Cardiac parasympathetic activity and ventricular diastolic interactions in individuals with spinal cord injury
Spinal Cord (2019)