Abstract
Study design:
Prospective, unblinded, multicenter, randomized, controlled, cross-over study assessing user preference and ease of use characteristics of two gel intermittent catheters in 81 self-catheterizing wheelchair-using men.
Objectives:
To evaluate the male user’s preference between a 30-cm and a 40-cm intermittent catheter (Apogee Intermittent Catheter, Hollister Incorporated, Libertyville, IL, USA) regarding the ease of insertion and removal, ability to control the catheter during insertion, bladder emptying confidence and ease of draining urine into a receptacle or connecting to a urine bag.
Setting:
Multiple institutions in the United States.
Methods:
Subjects were randomized to order of catheter use, using both 10 test catheters (30-cm) and 10 control catheters (40 cm). All catheters were 12 or 14 French and identical in design and composition, except length. Safety was assessed during the entire study period regarding adverse events (AE) and adverse device events (ADE). Subjects evaluated their ease of use characteristics after each catheter use and final catheter preference.
Results:
Subjects preferred the Apogee 40-cm intermittent catheter (91.4%) over the 30-cm length (8.6%). The preference was due to subject confidence of complete bladder emptying (70%), more satisfactory length (74%) and easier to drain into a receptacle (58%) with a portable urinal being the most utilized (37%), followed by toilet (35%). The only AE/ADE reported was minor urethral bleeding in one subject and minor pain in another subject, both with the 30-cm catheter. None were reported with the 40-cm catheter.
Conclusions:
The Apogee 40-cm catheter was the preferred intermittent catheter due to subject confidence in bladder emptying, ease of catheter manipulation and the ease of draining urine into a receptacle.
Similar content being viewed by others
Introduction
Urethral catheters made from metal or wood tubes coated with ghee (liquid butter) in India and hollow leaves of onion plants coated with lacquer in China can be traced back to 100 BC. Later hallmark events in catheter use included the introduction of the Foley balloon catheter in the 1930s and the concept of intermittent catheterization by Lapides and group1 in the 1970s. Modern catheter design length of about 40 cm can be attributed to historical catheter designs. A recent study showed an average male urethral length of ∼22 cm.2 In contrast, the average female urethral length is ∼4 cm.3 The urethral length differences have led to the development of novel shorter female intermittent catheters with greater comfort, ease of use and concealment. This study explores whether a shorter catheter would be perceived as a benefit to a male population who routinely perform intermittent catheterization.
The primary objective of this study was to assess male users’ preference between catheters with two different lengths (30 cm and 40 cm), but otherwise identical construction.
The secondary objective was to assess ease of use characteristics, including ease of insertion and removal, ease of controlling the catheter when inserting into the urethra, ability of the catheter to drain the bladder and ease of draining into a urine receptacle or ease with which to connect to a urine bag.
Materials and methods
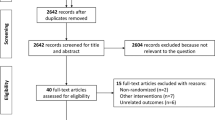
This unblinded, multicenter, randomized, controlled, prospective, cross-over study assessed user preference between two gel intermittent catheters. The study, conducted at seven sites between October 2010 and July 2011, was open to adult males who currently self-catheterize at least three times daily and use a wheelchair. Subjects had to be able to use a size 12 or 14 French catheter and self-catheterize for at least 2 months at the time of enrollment. The Control catheter was a single lumen, 40-cm Apogee Intermittent Catheter and the Test catheter was a single lumen 30-cm Intermittent Catheter (Figure 1). The two catheters were identical in all respects, except length. Subjects enrolled in the study were randomized to order of catheter use. The randomization scheme was balanced to site; no adjustments were made to control for a site effect.
The institutional review board approval was obtained along with informed consent from all participants before any study procedures being conducted. Each subject was given 10 Control catheters and 10 Test catheters to be used consecutively until all 20 catheters were used. Subjects were to either use the Test catheters first and then the Control catheters or the Control catheters first and then the Test catheters. Subjects were asked to complete a questionnaire after using each catheter and an overall preference questionnaire after all catheters had been used. Participation consisted of approximately 1 week of product use and two visits.
The data are analyzed using SAS v9.2, and includes a descriptive analysis of the demographic profile, including frequencies and measures of central tendency as appropriate. For overall comparisons using the χ2 in the primary and secondary objectives, the final sample size of 81 subjects is sufficient to detect a 20% difference in product performance at 80% power with a two-tailed Type I error rate of 0.05, based upon a current product acceptance of 80%.
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
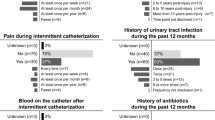
A total of 91 consented subjects were enrolled in the study. Ten subjects were removed from the data set for various protocol violations, resulting in a final data set of 81 eligible subjects available for analysis. The subject mean age was 38, with a height of 70 inches and weight of 185 pounds. Median duration of intermittent catheterization was 72 months. Subjects most commonly self-catheterized four times daily and described themselves as very physically active with full ability to grasp objects. The need to catheterize was most often secondary to spinal cord injury, particularly in the thoracic vertebrae. Sensation below the waist was minimal to none in the majority of patients. Table 1 yields the full-demographic profile. No serious events occurred in this study. Two minor adverse events were reported: one instance of minor urethral bleeding with use of a 30-cm catheter was reported by one subject, and minor pain during use of all 10 30-cm catheters was reported by a second subject.
Overall, 91.4% (74 subjects) preferred the longer 40-cm catheter compared with 8.6% (7 subjects) who preferred the shorter 30-cm catheter. The analysis of questionnaires revealed preference for the longer catheter in terms of ability to drain the bladder entirely (85 vs 36%, P<0.0001) and directing the urine into a receptacle (88 vs 55%, P<0.0001). The longer catheter was also determined to be easier to insert into the urethra (88 vs 72%, P<0.05), remove from the urethra after the urine was drained (96 vs 87%, P<0.05) and handle during insertion (90 vs 76%, P<0.05). Twenty-three subjects (28%) perceived that they were unable to drain their bladder adequately with the 30-cm catheter. Table 2 shows ease of use characteristics.
The top three reasons for preference of the longer catheter (n=74) were that it drained the bladder more completely (70%), it was a more satisfactory length for them (74%) and it was easier to drain into a receptacle (58%). The top three reasons for preference of the shorter catheter (n=7) were that it was easier to drain into a receptacle (100%), easier to handle during removal (86%) and easier to handle during insertion (71%). Tables 3 and 4 summarize reasons for preference.
Information was also collected on what subjects actually used as their drainage receptacle. Of 1389 collected responses, a portable urinal was most commonly utilized (37%), followed by drainage into a toilet (35%), a drainage bag (13%), ‘other’ receptacle (13%) and standard urinal (3%). Subjects who responded ‘other’ either were not able to drain their bladder or used another receptacle not listed (for example, water bottle, enema bottle, in the shower, container, and so on). Table 5 summarizes receptacle use practices.
Discussion
The primary objective of this study was to assess preference between catheters of two different lengths in men who empty their bladders by clean intermittent catheterization. All men in the study were wheelchair users and had been performing catheterization for at least 3 months.
A potential confounding factor in this study is the varying bladder sensory perception differences in patients suffering different types of neurological injury. This study design was intended to test catheter preference for management of their neuropathic voiding dysfunction regardless of etiology. Because of the potential for a bias toward those with an intact bladder filling proprioception, the study was also designed such that each individual patient served as their own control. In addition, it is the author’s opinion that this study’s design more accurately reflects the typical clinical practice as the causes of neurologic insult in wheelchair-using men performing intermittent self-catheterization are virtually always heterogeneous.
In 2011, Domurath et al.,4 reported on a trial with the use of a 30-cm telescoping catheter which was compared with a 40-cm length standard catheter. That study reported a non-statistically significant trend toward patient preference for the shorter length catheter with no significant difference in post void residual when comparing groups by ultrasound measurement after catheterization. In this study, two catheters were compared that differed not only in length but also in composition. The 30 cm, shorter length catheter was also of a telescoping compact type that might have impacted the study outcome as much as any other unique feature it presented.
In contrast, the main objective of this study was to identify user preference between two catheters that were identical in all ways with the exception of length. The primary objective was focused on patient perception of emptying and preference of catheter length. With each patient as their own cross-over control, there was a clear preference demonstrated for the longer length catheter. However, despite this preference, a small interesting subset of men (7/81) actually preferred the shorter catheter.
Overall, men who use a wheelchair and empty their bladder by clean intermittent catheterization prefer the standard 40-cm length catheter when compared with a shorter 30-cm length. One of the most commonly cited reasons for the preference of the longer catheter was the perception of the ability to more completely empty their bladder.
Data archiving
There were no data to deposit.
References
Bloom DA, McGuire EJ, Lapides J . A brief history of urethral catheterization. J Urol 1994; 151: 317–325.
Kohler TS, Yadven M, Manvar A, Liu N, Monga M . The length of the male urethra. Int Braz J Urol 2008; 34: 451–454.
Zacharin RF . The suspensory mechanism of the female urethra. J Anat 1963; 97 (Pt 3): 423–427.
Domurath B, Kutzenberger J, Kurze I, Knoth HS . Clinical evaluation of a newly developed catheter (SpeediCath Compact Male) in men with spinal cord injury: residual urine and user evaluation. Spinal Cord 2011; 49: 817–821.
Acknowledgements
Hollister research investigators contributed to the writing of this manuscript. This study was funded by Hollister Incorporated (ClinicalTrials.gov Identifier No. NCT01284361). Drs Costa, Kohler and Mr. Doran, as well as other participating centers were part of this investigation and received research funding. This study was funded by Hollister Incorporated.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Costa is a consultant for Coloplast Inc. Ms Menier is a statistician employed by Hollister Incorporated. Mr Doran has no disclosures. Dr Kohler is a consultant for American Medical Systems and Coloplast Inc. He is also on the speaker’s bureau for Allergan, Auxilium and Actient.
Rights and permissions
About this article
Cite this article
Costa, J., Menier, M., Doran, T. et al. Catheter length preference in wheelchair-using men who perform routine clean intermittent catheterization. Spinal Cord 51, 772–775 (2013). https://doi.org/10.1038/sc.2013.76
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2013.76