Abstract
Objectives:
To identify the natural course of changes in participation, employment, health and subjective quality of life over a 35-year interval among participants with spinal cord injury (SCI).
Methods:
Participants were enrolled in 1973 from a specialty hospital in the Midwestern United States and assessed again approximately 35 years later. The inclusion criteria were the following: having traumatic SCI; being 18 years of age or older; and a minimum of 2 years having elapsed post injury. There were 64 participants who responded on both occasions. Average age at follow-up was 61.5 years, with 41.1 years having passed since SCI onset. The Life Situation Questionnaire was used to measure outcomes.
Results:
Attrition analyses indicated that those who participated at follow-up were younger and had better overall outcomes at baseline (1973) when compared with those who dropped out of the study. Longitudinal analyses indicated a mixed pattern of favorable and unfavorable changes over the 35 years. The overall social participation decreased over time, although the sitting tolerance and hours spent in gainful employment increased. Non-routine physician visits increased. Satisfaction with employment improved over time, whereas satisfaction with social life, sex life and health declined. Self-reported adjustment improved, but the prediction of future adjustment in 5 years declined.
Conclusion:
Our study suggests that the natural course of SCI is marked by a survivor effect, whereby those with better outcomes are more likely to survive to follow–up, and a mixed pattern of favorable and unfavorable changes. Rehabilitation professionals should work to promote favorable outcomes in areas of strength, as well as minimize the likelihood of adverse outcomes.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) results in immediate and generally permanent changes to all aspects of life. The rehabilitation process is heavily focused on the time shortly after injury, including inpatient rehabilitation and transition to the community. However, life typically continues for years and even decades after SCI onset. What is the natural course of life changes after SCI? Answering this relatively simple and straightforward question requires a longitudinal investigation of changes in multiple life areas over time.
It is tempting to conceptualize the natural course of SCI entirely in terms of aging. As the years pass, an individual's chronological age increases, but so does the number of years after injury.1 Broader environmental changes also take place, such as those related to rehabilitation practices, medical and technological innovations, and funding practices. Longitudinal studies document the natural course of changes in life outcomes over a particular period of time reflecting a combination of factors, which may not easily be parceled into separate effects.
Several areas of life are relevant to adult life, including among those with SCI. These include vocation, social participation, health and quality of life. Relatively few longitudinal studies of SCI have been conducted. The number of health problems, fatigue, disability-related problems and shoulder pain have been found to increase over time, whereas range of motion decreases.2, 3 Physical independence, mobility, occupation and economic self-sufficiency scores on the Craig Handicap Assessment and Reporting Technique have also been found to decline with age, while social integration scores have improved.4
Several reports on a longitudinal cohort have been reported over a 30-year interval.5, 6, 7, 8, 9 Changes in outcomes have evolved over time. There has been a mixed pattern of favorable and unfavorable changes, with general improvements in employment outcomes, overall adjustment, and satisfaction with employment and finances. However, there was also a tendency for increases in need for medical care (hospitalizations), diminished social participation, and satisfaction with health, social life and sex life. Comparisons of outcomes over time with newly added cohorts (time lag analyses) suggested that longitudinal changes over at least the 11-year and 20-year intervals were partially explained by more general environmental changes.10, 11
Purpose and hypotheses
Our purpose was to identify the natural course of life-changes in self-reported participation, health and subjective well-being over a 35-year interval. Several hypotheses are based on the findings from earlier reports.
-
1
There will be a significant decline in activity level and health status over the 35-year follow-up.
-
2
There will also be a significant decline in satisfaction with activity and health status over the 35-year follow-up.
-
3
Adjustment, satisfaction with career and employment outcomes will improve over the 35-year follow-up.
Materials and methods
Participants
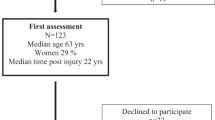
Participants were enrolled in 1973. All adults with traumatic SCI of at least 2 years duration who received renal function services at a large Midwestern University hospital clinic before 1973 were enrolled. There were 256 respondents in 1973, with an 85% response rate. Follow-up was conducted approximately 35 years later in 2008–2010, with 64 respondents. (Table 1 summarizes the pattern of attrition.)
Attrition
Several significant differences were identified in the Time 1 data between the 64 respondents who were surveyed for Time 2 and the initial full sample. Respondents were younger both at the time of the 1973 data collection (t(252)=−5.53, P⩽0.001) and at injury onset (t(254)=−3.43, P⩽0.001), and had lived fewer years after injury (t(254)=−3.43, P⩽0.001). Respondents reported more years of education (t(185)=2.77, P⩽0.01), greater satisfaction with health (t(249)=−2.56, P⩽0.01) and more frequent social outings (t(251)=3.65, P⩽0.001).
Procedures
Data were collected by mailed survey. Cover letters were sent to participants to describe the study and remind them of their previous participation. The full set of materials was sent 4–6 weeks later. A second mailing and follow-up phone call were initiated to the non-respondents, followed by a third set of materials. Participants were offered $30 in remuneration for participation.
Measures
The Life Situation Questionnaire (revised version will be supplied upon request) was developed in 1973 to measure the objective aspects of an individual's life after SCI.5 In essence, it is the integration of sets of items that describe the ‘life situation’ after SCI. At the time of study initiation, there were few available measures for outcome studies. The Life Situation Questionnaire includes five sets of items, including education and employment, activities/participation, recent treatments, self-rated adjustment and life satisfaction.
Education was defined as the number of years of formal education. Employment was defined as ‘working for pay’ and was assessed by the number of hours per week an individual spent working. Activity patterns included number of weekly visitors, frequency of weekly outings and sitting tolerance. Weekly visitors and weekly outings were presented as multiple-choice grouped frequencies in the original survey (rarely; 1–3 times per month; 1–2 times per week; 3 or more times per week). Sitting tolerance was also presented as multiple-choice (0–3; 4–7; 8–12 h; and >12 h). Recent medical history within the past 2 years included number of non-routine doctor visits, number of hospitalizations and days hospitalized. These were also presented as grouped frequencies in the original survey, with the number of physician visits and hospitalizations categorized as 0, 1–3, 4–10 and >10. Days hospitalized was categorized as none, less than a week, 1–4 weeks and >4 weeks.
In the follow-up assessment, activity and recent medical history items were either open-ended or presented as expanded categories. Sitting tolerance and days hospitalized were open-ended questions requiring the actual number of hours or days. Follow-up data were recoded to match the original grouped frequencies for the purposes of data analysis (for example, sitting tolerance was recoded into the following categories: 0–3; 4–7; 8–12 h; and >12 h).
The six life satisfaction items included living arrangements, employment, finances, social life, sex life and general health. Each of these required participants to rate their satisfaction with particular areas of life on a 5-point scale. Self-rated adjustment included two 10-point adjustment scales (current adjustment and future adjustment).
Analyses
Data analyses were conducted using SPSS. We reported descriptive statistics to summarize the participant characteristics. We then evaluated selective attrition by comparing biographic and injury characteristics, and the outcomes of participants who remained in the study since 1973 (n=64) with those who dropped out by follow-up (n=192). T-tests, the McNemar statistic and Wilcoxon's tests were used to test the significance of differences in the attrition analysis.
In the primary set of analyses, each outcome variable was compared across two times of measurement. The paired t-tests were used with continuous variables (years of education, hours spent working, present and future adjustment) whereas the Wilcoxon signed-rank test, a nonparametric test used to evaluate change over time (a paired difference test), was used with ranked categorical variables. Life satisfaction items were treated as ranked categorical variables to better clarify the proportion of individuals reporting positive ranks (increased satisfaction) and negative ranks (decreased satisfaction). We treated hospitalizations, treatments and participation variables in a similar manner, as they were initially presented as grouped frequencies (that is, ordinal measurement).
For employment status, we conducted the analyses including all participants, and then a second time restricting the analyses to participants who had not reached the traditional retirement age of 65. McNemar tests were used to identify a change in the proportion of individuals employed at each time of measurement.
Statement of ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Participant characteristics
The average age of respondents was 61.5±7.2 years, and mean time since injury was 41.4±4.9 years (see Table 2). Eighty-eight percent of them were male. Cervical injuries were reported by 66%. In all, 52% reported sensation below their level of injury, whereas 28% reported some voluntary movement, and only 8% were ambulatory. The majority of participants (89%) had worked at some time since injury. They had on average 15.1±2.9 years of education.
Changes in outcomes over time
Years of education significantly increased from 13.8 to 15.1 years (Table 3). The percentage employed was not significant while considering all participants or only those who were under 65 at follow-up. There was a marginally significant (P = 0.051) increase in the number of hours per week spent working (coding zero for non-employed) when all participants were considered, and a significant increase when only those under 65 were considered.
A significant increase was observed for sitting tolerance (Table 4). The frequency of weekly visitors and weekly outings decreased significantly over time. The number of non-routine physician visits increased significantly. Neither the number of hospitalizations nor the days hospitalized changed significantly.
Four of the six life satisfaction variables changed significantly (all except living arrangements and finances). Satisfaction with employment improved (from 3.1 to 3.7), with decreases in satisfaction with social life, sex life and health. The overall self-rated current adjustment increased significantly, but the overall self-rated future adjustment did not change significantly (there was a non-significant decreasing trend, P=0.08; Table 3).
Discussion
The current study was designed to identify the natural course of life changes over a 35-year period among a cohort of participants with SCI from the Midwestern United States. The natural course is differentiated from aging per se in that multiple factors affect longitudinal outcomes over time, only one of which is aging. Other factors include the unique circumstances or environmental changes over time.
Each of the study hypotheses was confirmed. There are several important points. First, study attrition was selective with those individuals who were better adapted to longer survival. The survivor effect was important to consider while evaluating outcomes, as it appeared to be a natural process by which those with the most favorable characteristics were maintained in the study. Not all attrition could be attributed to mortality, as only a limited number of factors were significantly related to attrition, whereas a much wider array of predictive factors has been identified in previous research.12, 13
There were several similarities with the earlier research over shorter intervals.7, 8, 9 In addition to the aforementioned survivor effect, there was a combination of favorable and unfavorable changes. Participants were clearly less active socially and continue to report a greater number of health problems, with corresponding diminished satisfaction in related areas. On the other hand, their self-rated adjustment and satisfaction with employment continued to be favorable.
While considering the trends reported earlier,9 it does appear that there are some subtle changes in those areas that were previously considered areas of improvement. Satisfaction with finances no longer indicated significant improvement, as was observed during earlier studies.9 Participants were no longer more likely to be working at follow-up, although this appeared to be due to the proportion of individuals who had reached retirement age (percentage employed was identical when considering all participants, but had improved overall among those under 65). Research in the general population suggests that, at least for men, satisfaction peaks at about the age of 65, after which it declines.14 These declines are greatest in the year before death. This trend may help to explain the declining life satisfaction over time, as individuals either pass the age of 65 or discontinue work. Given the limited life expectancy after SCI,15, 16 many individuals may have been surveyed while experiencing life changes nearing mortality.
Implications
Trieschmann17 conceptualized rehabilitation as a lifelong process, yet SCI is treated in many ways as more of an acute event. There is always the temptation to view the course of SCI as a negative process associated only with declines, but life indeed appears to evolve with aging after SCI, as those who survive rely on their ability to adjust and adapt to the changing circumstances. Overall, the adaptation appears to be remarkably successful despite many adverse changes in health and participation. The importance of adaptation should not be surprising, given the emphasis on successful coping, rather than life satisfaction, among those aging in the general population.18
Limitations
Several limitations must be acknowledged. First, the scope of the outcome variables is relatively limited by the limited options for outcome measurement available at the time this study was initiated. All longitudinal studies over this length of time would have some such limitations. Second, attrition over time was high even though the adjusted response rate excluding mortality was excellent (only 4 non-respondents out of 68). This issue is also inherent to longitudinal studies. Because mortality rates are higher after SCI, the attrition-related mortality was higher. In fact, given that the cohort averaged 35 years of age and nearly 10 years post injury at the time of enrollment, the sheer number of survivors over the 35-year interval is encouraging. The third limitation is the lack of racial–ethnic diversity. This is directly related to the geographical region of the United States from which participants were selected. Fourth, we did not attempt to adjust for statistical tests. This would have restricted the number of comparisons owing to the number of participants. Lastly, our findings are related to the natural course of SCI and are not an assessment of aging per se. We have provided no information for or against the hypothesis that aging is accelerated after SCI or that aging accelerates at a certain point based on chronological age or a particular number of years after injury.
Future research
Ongoing longitudinal studies are needed to continue to identify the natural course of SCI. Studies are needed to reveal the dynamic nature of changes in SCI outcomes as related to a variety of characteristics, including the timeframe of participant enrollment. Given the dramatic changes in rehabilitation practices over the past two decades, those injured more recently have experienced different rehabilitation cultures. The effects of such broad environmental changes require additional research, including the use of time-lag designs that enroll new cohorts and compare outcomes over time among different cohorts.
Future research should also enroll substantial numbers of participants sufficient for analysis of aging effects. This will require starting with cross-sectional cohorts based on three aging parameters, including chronological age, age at injury onset and years lived after injury. Shorter intervals of follow-up will likely be required to counteract attrition. A search for explanatory factors of change will also help to interpret the study findings. No single study can fully identify the natural course of SCI or any other disabling condition, so progress will come only through multiple studies using similar, but not identical, methodologies.
References
Jensen MP, Hirsh AT, Molton IR, Bamer AM . Sleep problems in individuals with spinal cord injury: frequency and age effects. Rehabil Psychol 2009; 54: 323–331.
Ballinger DA, Rintala DH, Hart KA . The relation of shoulder pain and range-of-motion problems to functional limitations, disability, and perceived health of men with spinal cord injury: a multifaceted longitudinal study. Arch Phys Med Rehabil 2000; 81: 1575–1581.
McColl MA, Arnold R, Charlifue S, Glass C, Savic G, Frankel H . Aging, spinal cord injury, and quality of life: structural relationships. Arch Phys Med Rehabil 2003; 84: 1137–1144.
Weitzenkamp DA, Jones RH, Whiteneck GG, Young DA . Ageing with spinal cord injury: cross-sectional and longitudinal effects. Spinal Cord 2001; 39: 301–309.
Crewe N, Krause J . An eleven-year follow-up of adjustment to spinal cord injury. Rehabil Psychol 1990; 35: 205–210.
Krause JS . Longitudinal changes in adjustment after spinal cord injury: a 15-year study. Arch Phys Med Rehabil 1992; 73: 564–568.
Krause JS . Changes in adjustment after spinal cord injury: a 20-year longitudinal study. Rehabil Psychol 1998; 43: 41–55.
Krause JS, Broderick L . A 25-year longitudinal study of the natural course of aging after spinal cord injury. Spinal Cord 2005; 43: 349–356.
Krause JS, Coker JL . Aging after spinal cord injury: a 30-year longitudinal study. J Spinal Cord Med 2006; 29: 371–376.
Krause JS, Crewe NM . Chronologic age, time since injury, and time of measurement: effect on adjustment after sinal cord injury. Arch Phys Med Rehabil 1991; 72: 91–100.
Krause JS, Sternberg M . Aging and adjustment after spinal cord injury: the roles of chronologic age, time since injury, and environmental change. Rehabil Psychol 1997; 42: 287–302.
Krause JS, Carter RE, Pickelsimer E, Wilson D . A prospective study of health and risk of mortality after spinal cord injury. Arch Phys Med Rehabil 2008; 89: 1482–1491.
Krause JS, Zhai Y, Saunders LL, Carter RE . Risk of mortality after spinal cord injury: an 8-year prospective study. Arch Phys Med Rehabil 2009; 90: 1708–1715.
Mroczek DK, Spiro A, 3rd . Change in life satisfaction during adulthood: findings from the veterans affairs normative aging study. J Pers Soc Psychol 2005; 88: 189–202.
Strauss DJ, DeVivo MJ, Paculdo DR, Shavelle RM . Trends in life expectancy after spinal cord injury. Arch Phys Med Rehabil 2006; 87: 1079–1085.
DeVivo MJ . Estimating life expectancy for use in determining lifetime costs of care. Top Spinal Cord Inj Rehabil 2002; 7: 49–58.
Trieschmann RB . Spinal Cord Injuries: Psychological, Social and Vocational Rehabilitation, 2nd edn. Demos: New York, 1988.
Fisher BJ . Successful aging, life satisfaction, and generativity in later life. Int J Aging Hum Dev 1995; 41: 239–250.
Acknowledgements
The authors acknowledge the following members of the research team without whose contributions completion of this article would not have been possible: Richard Aust, Jennifer Coker, Emily Johnson, Karla Reed, Jillian Ricks and Dr Lee Saunders.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Disclaimer
The contents of this publication were developed under grants from the Department of Education, NIDRR grant numbers H133G020239, H133B090005 and H133G060126. However, those contents do not necessarily represent the policy of the Department of Education and any endorsement by the Federal Government should not be assumed.
Rights and permissions
About this article
Cite this article
Krause, J., Bozard, J. Natural course of life changes after spinal cord injury: a 35-year longitudinal study. Spinal Cord 50, 227–231 (2012). https://doi.org/10.1038/sc.2011.106
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.106
Keywords
This article is cited by
-
Trends in nonroutine physician visits and hospitalizations: findings among five cohorts from the Spinal Cord Injury Longitudinal Aging Study
Spinal Cord (2020)
-
Sensory and motor responses after photobiomodulation associated with physiotherapy in patients with incomplete spinal cord injury: clinical, randomized trial
Lasers in Medical Science (2020)
-
Associations between time since onset of injury and participation in Dutch people with long-term spinal cord injury
Spinal Cord (2018)
-
Participation in activities and secondary health complications among persons aging with traumatic spinal cord injury
Spinal Cord (2017)
-
The natural course of spinal cord injury: changes over 40 years among those with exceptional survival
Spinal Cord (2017)