Abstract
Study design:
Observational cohort study.
Objectives:
To evaluate ongoing health and community reintegration of patients with spinal cord injury (SCI) after discharge from inpatient rehabilitation in Nepal.
Setting:
Nepal.
Methods:
This study follows a cohort of 37 patients with SCI in Nepal, 1–2 years after discharge from inpatient rehabilitation in 2007. Participants were visited at home and data were obtained through semi-structured interviews that evaluated health, independence in daily living (Modified Barthel Index), community participation (Participation Scale) and barriers due to socioeconomic issues, housing, accessibility, and availability and use of mobility aids.
Results:
One-quarter of the cohort had died (35% of wheelchair users). Secondary health concerns, such as pressure ulcers and urinary tract infections, were common in the 24 patients interviewed, and eight had been rehospitalized to treat them. Inappropriate wheelchairs, inadequate housing and rugged terrain restricted accessibility. 80% of wheelchair users could not enter their homes independently and 74% of those who were using mobility aids could not access the community independently because of the physical terrain. Of all those who were interviewed, half had no accessible toilet, access to a water source or road access to their home. Community participation was a challenge for most using mobility devices, and less than half earned any income.
Conclusion:
This study identifies important areas of focus for rehabilitation centres in less-resourced contexts like Nepal to help with reintegration after discharge: vocational training during or after rehabilitation; accessible housing; wheelchairs appropriate to the terrain and the need for strong community-based rehabilitation.
Similar content being viewed by others
Introduction
Spinal Cord Injury (SCI) is a particular challenge in less-resourced countries, where lack of infrastructure and medical facilities limit access to health care, rehabilitation and assistive devices. In rural Nepal and India, many patients live in remote villages where subsistence farming is the primary source of income, and where steep terrain, limited road access and inaccessible housing are often barriers to those using mobility devices.1, 2, 3, 4, 5, 6
Green Pastures Hospital and Rehabilitation Centre (GPHRC), in Pokhara, Nepal, has been providing rehabilitation for patients with SCI since the mid 1990's,7 and is one of the two adult rehabilitation centres in Nepal (population 30 million). Pokhara (population 250 000) is situated in the mid-west of Nepal, with employment from tourism, small businesses and government institutions. GPHRC treats patients from the western half of Nepal through referral from primary care hospitals, health centres, community health workers and self-referral. It is unknown as to what proportion of those with SCI have access to a primary or tertiary care hospitals in Nepal.
Incidence and prevalence of SCI in Nepal are unknown. Worldwide incidence of traumatic SCI ranges from 9 to 174 per million population, and prevalence from 50 to 900 per million population.8 Thus an estimate of yearly incidence of traumatic SCI in Nepal is 300–5000, and prevalence 1500–25 000. One hospital in eastern Nepal reported 149 traumatic SCI admissions from 2001 to 20041 and 233 from 1997 to 2001.2 There are no reports of numbers of non-traumatic SCI in Nepal; one Indian hospital reported that 13% of 207 SCI admissions in 2003–2004 were non-traumatic.9
GPHRC is a 70-bed hospital that provides rehabilitation for patients affected by leprosy, SCI, amputation, burns, cerebral palsy and other physical disabilities. The rehabilitation team includes physicians, nurses, physical and occupational therapists, orthopaedic technologists, health educators, counsellors and peer counsellors. SCI patient outcomes after discharge from rehabilitation at GPHRC have been a concern, as approximately one-third of patients were found to require readmission for treatment of secondary complications. However, because of the challenges involved in completing follow-up in rural Nepal, formal evaluation has been limited.
Without good community reintegration, patients are more likely to get secondary health complications, such as pressure ulcers (PU) and urinary tract infections (UTI), resulting in rehospitalization or even death.4, 7, 10, 11, 12, 13 Based on GPHRC patient statistics, rehabilitating a SCI patient with PU results in hospitalization costs five times greater, and length of stay at least twice as long as compared with that of a patient without PU. In the west, PU account for approximately one-quarter of the cost of care for individuals with SCI, and 7–8% die from related complications.14
The objective of this study was to evaluate ongoing health and community reintegration of all patients with SCI discharged in 2007 from GPHRC at least one year post-discharge, and to evaluate barriers due to socioeconomic issues, housing, accessibility, and availability and use of mobility aids. Reported barriers may inform inpatient and community based rehabilitation (CBR) efforts in Nepal and other less-resourced countries.
Materials and methods
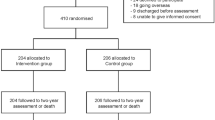
In this study, all persons with SCI discharged in 2007 from GPHRC inpatient rehabilitation were contacted for a follow-up home visit at least one year post-discharge. Medical chart review identified SCI patients discharged in 2007 (none excluded), as well as initial demographics, neurological level, completeness of injury and length of stay. All patients had been discharged home (sometimes a different house than pre-injury), as there are few other options in Nepal. Ethics approval was obtained through the research ethics boards of International Nepal Fellowship and Queen's University, Canada prior to implementation of the study, and informed consent obtained from participants.
Follow-up data were obtained through semi-structured interviews at participants’ homes with a national Nepali-speaking rehabilitation staff person and the primary author. Interviews included questions about: PU, UTI, and other secondary health complications, accessibility of home and community environments, employment and financial concerns, sexuality, wheelchair and/or mobility-aid use. All participants were asked the same questions. PU were visually examined, and categorized as either stage 2 (partial-thickness) or stage 3+ (full-thickness) tissue breakdown.14
Quantitative measures included the Modified Barthel Index (MBI)15 and the Participation Scale (P-Scale).16 The MBI evaluates independence in activities of daily living (ADL) in the areas of self-care, continence and locomotion.15 The MBI has been used in SCI populations,7, 17, 18 and was measured by GPHRC at admission and discharge. The P-Scale evaluates client-perceived community participation in the domains of general tasks, communication, learning, mobility, self care, domestic life, interpersonal interactions and relationships.16 It was developed to be cross-cultural and has been translated and validated for use in Nepal for various disabilities including SCI.16, 18 Descriptive statistics were applied to describe the quantitative measures and interview results.
Results
Of the 37 individuals discharged in 2007, 9 were reported deceased by family members. Twenty-four of the remaining individuals were contacted and visited 11–27 months post discharge (cohort demographics: Table 1). Of the 37 individuals discharged in 2007, 84% had been injured through falling from heights (15 from trees, 6 from buildings, 4 from ladders/construction and 6 from hill/cliff); the remaining 6 patients each had SCI of different etiologies: motor vehicle accident, gunshot wound, spinal tuberculosis, meningitis, transverse myelitis and unknown cause. Seven patients were readmitted in 2007; of them, two had died, two could not be contacted, and three were included in follow-up (one wheelchair user, two canes). Of the 24 participants visited, 15 were wheelchair users, 4 required walking aids (1 walker, 1 crutches and 2 canes) and 5 could walk unassisted.
The nine deceased patients were somewhat older, had a longer hospital stay and lower ADL independence (reflected by MBI scores) at discharge compared with those of the entire cohort. All nine were wheelchair users; eight were male and eight had complete SCI. It was difficult to determine the cause of death, as it rarely occurred in a medical setting; however, infections, PU and possible suicide (two individuals) were reported by family and caregivers.
Secondary health complications
Secondary health complications were common amongst participants. Ten were rehospitalized because of complications after discharge (all mobility-aid users). At the time of home visit, 9 had unhealed PU; all together 13 (12 wheelchair users) had developed PU since discharge (8 had grade 3+ ulcers). Eight were readmitted to GPHRC because of PU, and one died subsequent to the interview because of PU complications. Eleven participants reported UTI since discharge, and four required hospitalization. At the time of interview, half the patients were self-voiding, six used indwelling catheters, four used intermittent catheters and two needed catheters, but were not using them because of cost or poor access to supplies.
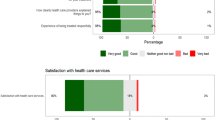
When asked an open question about other health problems, nine reported ongoing pain and six reported problems with spasticity or contractures. Eight participants reported depressed mood, two reported sleep problems, and two reported issues with drugs and alcohol. However, most of them felt reasonably positive about their health. Half of those who were interviewed felt that their health would continue to improve, whereas only five felt that their health would worsen.
Home and community accessibility
Lack of home and community accessibility was a major barrier for most using mobility aids (Table 2). Nearly half of the participants lived in hilly areas; 79% outside the city. In all, 80% of wheelchair users could not enter their homes independently and 74% of those who were using mobility aids could not access the community independently. Six had no community wheelchair access even with assistance, because of steep terrain. Half of those who were interviewed and two-thirds of wheelchair users, had no accessible toilet, could not access a water source and had no road access to their home (three lived at a distance of >30-min walk from a road). These challenges were reflected in P-Scale scores: 79% of all participants (93% of wheelchair users) indicated ‘severe’ or ‘extreme’ restrictions to community participation. No statistical analysis was run, because of small numbers however, it appears that although the MBI may have been increased between admission and discharge, no changes in ADL independence were evident between discharge and follow-up visit.
All but two participants lived with family, and all but one reported supportive families. At the time of visit, most of the patients required a caregiver, though seven were independent for ADL. Caregivers were most frequently wives (six participants), followed by parents, including in-laws (five participants), and husbands, with help from children or siblings (four participants). Most caregivers were present during hospitalization (caregiver required for inpatient stay), and would have learned about care alongside the patient.
Employment
Lack of finance was a barrier for many. Six participants earned enough to support themselves (two from army pensions), four earned some income, two were in training, seven helped with tasks at home and five were unemployed. Nearly half (11 participants) expressed financial concerns, and seven wanted training or employment. Only six mobility-device users earned any income at all. Finances were a barrier to implementing accessible solutions at home, and for eight of nine participants who had home improvements, modifications were only possible through financial assistance from local non-governmental organizations. Three wheelchair users relocated to urban areas for more accessible living, training and employment.
Sexuality
In the past few years, GPHRC staff have provided education about changes in sexual function after SCI. At the home visit, half of the participants and spouses recalled having education about sexuality, and 80% found it to be helpful. Two-thirds of married participants reported receiving education, compared with one-third of unmarried participants. Four participants (three unmarried) reported that more information would have been helpful. Half of the married participants reported continuing marital relationships after SCI. Reasons for not continuing sexual relations included concerns about birth control, lack of interest and partner's fear that they were too ill.
Wheelchairs
All wheelchair users were provided with standard folding four-wheel chairs donated by the Wheelchair Foundation. Three had replaced their wheelchairs since discharge, and seven wheelchairs were in serious disrepair. All but one were using wheelchair cushions made of poor-quality locally available foam with vinyl covers (cushions were not included with donated wheelchairs).
Based on self-report, participants spent an average of 5 h per day in their wheelchair, and only four regularly used their wheelchairs for longer than 6 h per day. Three wheelchair users could not mobilize in their wheelchairs at all, because of inaccessible home environments. The remaining time was spent primarily in bed. Two had no mattresses on wooden bed frames; the rest had mattresses made of locally available foam or cotton materials.
Discussion
This study followed 37 SCI patients discharged in 2007 from GPHRC. Although the results from this study may be extrapolated to similar SCI populations, evidence is limited to the cohort measured. Many responses were self-reported, providing an indication of self-perceived reintegration, but could not be independently verified. No statistical analysis was performed because of small numbers and low statistical power. Despite these limitations, this study provides valuable insight into the outcomes after discharge with SCI in Nepal.
The demographics of the patient cohort in this study were similar to others reported in Nepal and India.1, 11, 18, 19, 20 Most (89%) had traumatic SCI, similar to 87% reported in India,9 but different from the west, where non-traumatic SCI incidence is similar to traumatic.18, 21 In the west, motor vehicle accidents are the most common cause of SCI,8 however, in Nepal and India, falls are the most common cause (Tables 3a: and b). Falls from trees often occurred when climbing for firewood or fodder for livestock. Safety precautions are rare in Nepal, and thus falling from steep paths, ladders, scaffolding, roofs and verandas is also common.
In this cohort, the mortality rate was at least 24% at follow-up; 35% amongst wheelchair users. This is similar to SCI studies in less-resourced countries: 21% in Nepal,7 25% in Zimbabwe,10 but much higher than the west, where 1-year survival is 90–99%22.
Secondary health complications
PU (54% all PU; 33% Grade 3+) and UTI (46%) were common after discharge, resulting in rehospitalization for one-third of patients. PU have been reported in about one-third of patients in less-resourced settings,4, 10, 13, 20 similar to an incidence of 20–31% in the west.14 UTI were reported in 35%,4 44%20 and 54%13 of participants in other follow-up studies. In India, readmission was reported for 28%4–48%20 of patients because of health complications. In both cases interventions and follow-up reduced readmissions.4, 20
Reducing the incidence and severity of complications from PU or UTI is essential for the ongoing health of those with SCI.4, 14 Considerations such as appropriate wheelchairs, seat cushions, bed mattresses, access to catheters and their regular maintenance are important. In addition, teaching PU and UTI prevention strategies is an essential part of rehabilitation for SCI patients and their caregivers during and after hospital stay.7
Home and community accessibility
Lack of accessibility was a major barrier for those using mobility devices, particularly wheelchairs. Although MBI scores at discharge and follow-up indicated no decrease in ADL independence, similar to previous reports,7 most reported ‘severe’ or ‘extreme’ restrictions to community participation based on their P-Scale scores. Many required assistance to enter their homes, to get water, for toileting and to access their communities, with heavy reliance on family and neighbours for support.
Although it has been used elsewhere,7, 17, 18 the sensitivity of the MBI to changes in SCI populations has been questioned.17 This may suggest why no change was apparent between MBI at discharge and home visit (though it appeared sensitive to changes between admission and discharge). This measure was being used at GPHRC for all rehab patients, and was used in the follow-up to provide a comparison with their inpatient stay.
The P-Scale has been widely used to measure community participation,23 but only a few studies report results in SCI populations. A Canadian study reported a P-Scale of ‘severe’ or ‘extreme’ restriction for 19 of 24 (79%) community dwelling participants with disabilities, including 3 with SCI,24 the same percentage reported in this current study. Another compared the average P-Scale scores of SCI inpatients in Canada (mild restriction) and Nepal (moderate restriction).18 The lower restriction reported may be due to the accessibility of the inpatient rehabilitation facilities, compared with the greater participation barriers experienced by patients at home.
All primary caregivers were family members, most frequently wives, as has been observed in other studies.7, 12 However, although others were often willing to help in person, only one family had independently done renovations to improve accessibility. Even simple, inexpensive solutions to improve accessibility required external advice and financial support. A study in Afghanistan found that easy home access had a significant influence on self-perceived quality of life (QOL) for those with SCI.13 Improving home accessibility must be a priority, to allow for better reintegration of patients into their family and communities.
Employment
Employment and finances were major issues for patients after SCI, especially for those requiring mobility devices: only one-third earned any income at all. This is similar to studies in less-resourced countries that report employment rates of 13%,10 27%13 and 35%.4 In the west, it is estimated that 30–50% are employed after SCI, and that it is associated with social integration and life satisfaction.25 In Bangladesh, a vocational reintegration program was shown to increase the employment to 50%.12 Employment and social integration were significantly correlated with QOL after SCI in an Indian study11.
Having no productive task or job, paid or otherwise, was a problem for one-quarter of mobility-device users in this study. Boredom and lack of purpose due to unemployment were cited as major problems for 33% after SCI in Zimbabwe.10 Suicide and lack of community integration are more common in those who are not employed.4 One Nepali SCI study reported that 58% of patients had been primary breadwinner before injury, and 80% were supporting over 6 people.1 Better vocational training would be beneficial to improve outcomes after SCI25.
Sexuality
Sexuality after SCI is a topic rarely mentioned in studies in less-resourced countries, presumably because of cultural taboos.26 In the current study, half of the married couples reported continuing sexual relations, similar to 61% in an Indian study.26 The Indian study reported most desired more sexual education during rehabilitation and half expressed dissatisfaction with their sex life.26 Cordial partner relations were found to be correlated with improved QOL after SCI in another Indian study.11 The current study supports the importance of education around sexuality after SCI for married and unmarried patients, despite cultural taboos.
Wheelchairs
There exists some consensus regarding the need for wheelchair prescription appropriate to the terrain and intended use.27 Donated standard wheelchairs did poorly in this study. Within two years, two-thirds needed replacement. Most participants could not access their community independently in these wheelchairs, and three were not using them at all. Because cushions were not included with the wheelchair, poor-quality locally-available materials were used for pressure relief. Studies in India found standard wheelchairs ‘inappropriate’28 or ‘useless’29 in the local setting, and 71% were unused or sold.29 Wheelchairs developed specifically for use in less-resourced, rural contexts would be much more suitable.
Summary
Persons with SCI in Nepal face many challenges after returning home from rehabilitation. This study highlighted several such problems of significance. Ongoing health is a serious issue. One-quarter of those who were discharged in 2007 had died (one-third of wheelchair users), and nearly half had been rehospitalized because of PU or UTI. Rugged terrain and inaccessible housing made access to the community difficult. Inappropriate wheelchairs further restricted accessibility, and poor-quality wheelchair cushions and mattresses made PU prevention more difficult.
Community participation was a challenge for most using mobility devices. Less than half earned any income, and one-quarter of those who were using mobility devices had no employment/tasks in the home or community. Better patient and family education, follow-up and CBR support are needed to help families and communities improve the participation of persons with SCI. All of these issues are challenges in less-resourced countries; however, measures can and are being taken to improve the situation for wheelchair users in Nepal, including training and education for CBR workers and community groups, and advocacy by those with mobility impairments themselves.
This study identifies important areas of focus for rehabilitation centres in less-resourced contexts to help with reintegration after discharge: vocational training during or after rehabilitation is necessary for many patients, accessible housing is essential and must be considered prior to discharge, appropriate wheelchairs and cushions are also necessary. This study highlights the need for strong CBR to improve accessibility and provide support to those with SCI so that they can better participate in and contribute to their families and communities.
References
Shrestha D, Garg M, Singh GK, Singh MP, Sharma UK . Cervical spine injuries in a teaching hospital of eastern region of Nepal: a clinico-epidemiological study. J Nepal Med Assoc 2007; 46: 107–111.
Lakhey S, Jha N, Shrestha BP, Niraula S . Aetioepidemiological profile of spinal injury in eastern Nepal. Trop Doct 2005; 35: 231–233.
Singh R, Sharma SC, Mittal R, Sharma A . Traumatic spinal cord injuries in Haryana: an epidemiological study. Indian J Community Med 2003; 28: 184–186.
Prabhaka MM, Thakker TH . A follow-up program in India for patients with spinal cord injury: paraplegia safari. J Spinal Cord Med 2004; 27: 260–262.
Richardson SA . Physical impairment, disability, and handicap in rural Nepal. Dev Med Child Neurol 1983; 25: 717–726.
Goudel C . A report on disability in the Western Region of Nepal. Asia Pacific Disabil Rehabil J 2004; 15: 86–94.
Herm FB, Spackman J, Anderson AM . Experiences with family supported rehabilitation of people with spinal cord injury. Asia Pacific Disabil Rehabil J 2000; 11: 31–35.
Furlan JC, Krassioukov A, Miller WC, von Elm E . Epidemiology of traumatic SCI. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, et al (eds). Spinal Cord Injury Rehabilitation Evidence, vol. 3.0. Vancouver, Canada, 2010.
Agarwal P, Upadhyay P, Raja K . A demographic profile of traumatic and non-traumatic spinal injury cases: a hospital-based study from India. Spinal Cord 2007; 45: 597–602.
Levy LF, Makarawo S, Madzivire D, Bhebhe E, Verbeek N, Parry O . Problems, struggles and some success with spinal cord injury in Zimbabwe. Spinal Cord 1998; 36: 213–218.
Singh R, Dhankar SS, Rohilla R . Quality of life of people with spinal cord injury in Northern India. Int J Rehabil Res 2008; 31: 247–251.
Hansen CH, Mahmud I, Bhuiyan AJ . Vocational reintegration of people with spinal cord lesion in Bangladesh–an observational study based on a vocational training program at CRP. Asia Pacific Disabil Rehabil J 2007; 18: 63–75.
Deconinck H . The health condition of spinal cord injuries in two Afghan towns. Spinal Cord 2003; 41: 303–309.
Regan M, Teasell RW, Keast D, Aubut JL, Foulon BL, Mehta S . Pressure ulcers following spinal cord injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, et al (eds). Spinal Cord Injury Rehabilitation Evidence, Vol. 3.0. Vancouver, Canada, 2010.
Shah S, Vanclay F, Cooper B . Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol 1989; 42: 703–709.
Van Brakel WH, Anderson AM, Mutatkar RK, Bakirtzief Z, Nicholls PG, Raju MS et al. The participation scale: measuring a key concept in public health. Disabil Rehabil 2006; 28: 193–203.
Anderson K, Aito S, Atkins M, Biering-Sørensen F, Charlifue S, Curt A et al. Functional recovery measures for spinal cord injury: an evidence-based review for clinical practice and research. J Spinal Cord Med 2008; 31: 133–144.
Wee JM, Schwarz R . An international comparative study assessing impairment, activities, and participation in spinal cord injury rehabilitation–a pilot study. Asia Pacific Disabil Rehabil J 2004; 15: 42–52.
Chacko V, Joseph B, Mohanty SP, Jacob T . Management of spinal cord injury in a general hospital in rural India. Paraplegia 1986; 24: 330–335.
Singh R, Rohilla RK, Siwach R, Dhankar SS, Magu NK, Sangwan SS . Health related problems and effect of specific interventions in spinal cord injury: an outcome study in Northern India. Eur J Phys Rehabil Med 2010; 46: 47–53.
New PW, Sundararajan V . Incidence of non-traumatic spinal cord injury in Victoria, Australia: a population-based study and literature review. Spinal Cord 2008; 46: 406–411.
van den Berg MEL, Castellote JM, de Pedro-Cuesta J, Mahillo-Fernandez I . Survival after spinal cord injury: a systematic review. J Neurotrauma 2010; 27: 1517–1528.
Magasi S, Post MW . A comparative review of contemporary participation measures’ psychometric properties and content coverage. Arch Phys Med Rehabil 2010; 91: S17–S28.
Wee J, Lysagh R . Factors affecting measures of activities and participation in persons with mobility impairment. Disabil Rehabil 2009; 31: 1633–1642.
Noreau L, Escorpizo R, von Elm E, Miller WC, Tawashy AE . Work and Employment. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, et al. (eds). Spinal Cord Injury Rehabilitation Evidence, Vol. 3.0. Vancouver, Canada, 2010.
Sharma SC, Singh R, Dogra R, Gupta SS . Assessment of sexual functions after spinal cord injury in Indian patients. Int J Rehab Res 2006; 29: 17–25.
Borg J, Khasnabis C (eds). Guidelines on the provision of manual wheelchairs in less-resourced settings. World Health Organization: Geneva, Switzerland, 2008.
Mukherjee G, Samanta A . Wheelchair charity: a useless benevolence in community-based rehabilitation. Disabil Rehabil 2005; 27: 591–596.
Kim J, Mulholland SJ . Seating/wheelchair technology in the developing world: need for a closer look. Tech Disabil 1999; 11: 21–27.
Acknowledgements
This study received financial support from Livablity Ireland, and in-kind support from International Nepal Fellowship and the Department of Physical Medicine and Rehabilitation, Queen's University, Canada. Sandra Boone, GPHRC Superintendent, provided invaluable advice and assistance during this project. The study was made possible by Nepali rehabilitation staff who participated in home visits: Juna Gurung, Laxmi Shahi, Sita KC, Hera Shahi, Bimila KC, Purna Thapa and those who helped to locate discharged patients. Thanks to Megan Barker, Occupational Therapist, who interviewed two rural participants when the primary author was strike bound in Pokhara. Finally thanks to the study participants who welcomed us into their homes with such hospitality.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Scovil, C., Ranabhat, M., Craighead, I. et al. Follow-up study of spinal cord injured patients after discharge from inpatient rehabilitation in Nepal in 2007. Spinal Cord 50, 232–237 (2012). https://doi.org/10.1038/sc.2011.119
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.119
Keywords
This article is cited by
-
Incidence, severity and time course of pressure injuries over the first two years following discharge from hospital in people with spinal cord injuries in Bangladesh
Spinal Cord (2022)
-
Telerehabilitation for individuals with spinal cord injury in low-and middle-income countries: a systematic review of the literature
Spinal Cord (2022)
-
Functional outcome following inpatient rehabilitation among individuals with complete spinal cord injury in Nepal
Spinal Cord Series and Cases (2021)
-
Overcoming Barriers to Accessing Surgery and Rehabilitation in Low and Middle‐Income Countries: An Innovative Model of Patient Navigation in Nepal
World Journal of Surgery (2021)
-
Loss of work-related income impoverishes people with SCI and their families in Bangladesh
Spinal Cord (2020)