Abstract
Study design:
Longitudinal, multi-wave panel design.
Objectives:
To explore the changes in and the relationships between appraisals and coping with mood, functioning and quality-of-life (QOL) pre- and post-rehabilitation for acute spinal cord injury (SCI).
Setting:
The data collected was part of an ongoing study from specialist units in selected British, Swiss, German and Irish SCI centres.
Methods:
Questionnaires (Functional Independence, QOL, Mood, Appraisals, Coping and Support) were administered to 232 patients at 12 weeks post injury and sent to participants at 1 and 2 years post injury by post.
Results:
Significant changes were observed in various outcome measures between 12 weeks and 1 year post injury, with little significant change occurring during the following year. Appraisals and coping at 12 weeks post injury were significantly related to outcome scores and also contributed significantly to the variance in QOL, mood and stress-related growth at 2 years post injury.
Conclusion:
The study provides further evidence for the link between appraisals, coping and subsequent adjustment to injury. Suggestion is made for the potential benefit of early assessment and intervention for patients at risk of poor adjustment to SCI.
Similar content being viewed by others
Introduction
Sustaining a spinal cord injury (SCI) not only causes major changes to an individual's physical and functional independence but also the extended rehabilitation period means that the patient's personal life style is similarly disrupted. While the patient relearns simple tasks or masters new skills, they must also adjust to and accommodate to life with a SCI.
Quality-of-Life (QOL) ratings taken from SCI populations are generally found to be lower than those obtained from the general population.1 Why however, in-depth analysis of these findings has revealed that QOL ratings are linked to secondary complications, activity limitations and barriers to participation2, 3 rather than to factors relating to the injury itself or degrees of physical ability.4, 5 In fact, the majority of people with SCI report a high level of life satisfaction,6 with research indicating that life satisfaction is directly related to involvement in productive activities, such as employment and leisure pursuits.7 Qualitative studies highlight the importance of meaningful relationships, responsibility, a sense of control over one's own life and engagement in meaningful activity in increasing the individual's QOL.8
Psychological problems (for example, depression and anxiety) following SCI also appear to be related to individual appraisals and coping responses rather than level of injury or functional impairment.1 Social support has been found to be related to psychological outcomes and adjustment after SCI,9, 10 has been identified as a predictor of early mortality11 and is associated with low hopelessness and depression scores.12
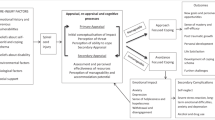
A review by Galvin and Godfrey13 suggested that the way people think about or ‘appraise’ their injury and the coping strategies they use in response to these appraisals have a significant role in the process of adjustment. In this context we consider ‘adjustment’ to include both psychological wellbeing and social functioning. In individuals with SCI, negative coping strategies have been linked to increased levels of depression and emotional distress14 and decreased levels of life satisfaction and participation,15 whereas positive adjustment to injury is found to be associated with active coping and positive reinterpretation.16
Kennedy, Lude, Elfström and Smithson17 examined the relationship between appraisals of injury and coping responses across time to find that individuals who initially interpret their injury as a challenge are more likely to use adaptive coping strategies such as acceptance. At 1-year follow-up, their scores on measures of QOL, anxiety and depression were considerably better than in individuals who initially interpreted their injury as a loss or a threat.
With increasing research suggesting a link between psychological factors and long-term outcomes, the current study aimed to explore the relationships between appraisals and coping variables, psychological wellbeing and QOL pre- and post-active rehabilitation. The current study extends research by Kennedy, Lude, Elfström and Smithson18 by following up participants at 1 and 2 years post injury. The questions to be explored are:
-
1
What changes are observed in appraisal and coping variables and outcome scores between 12 weeks, 1 year and 2 years post injury?
-
2
What are the relationships between appraisals and coping variables at 12 weeks post injury and outcome scores at 2 years post injury?
Materials and methods
Participants
Patients with newly acquired traumatic/non-traumatic lesions were recruited from selected British, Swiss, German and Irish spinal centres. Individuals recruited had sustained their injury between the ages of 18 and 83 years, and were fluent in the language of the country from which they were recruited. Individuals with a known head injury or communication disorder were excluded from the study, as such difficulties would prevent comprehension of and completion of the questionnaires.
Design
A longitudinal multi-wave panel design was used. Data was collected at the following time points: 12 weeks post injury, 1 year post injury and 2 years post injury.
Materials
The following questionnaires were chosen as they are frequently used to measure the concepts addressed in this study, they have good psychometric properties and have previously been used with individuals with SCI. A double translation method was used for all questionnaires.
Outcome measures
Functional Independence Measure (FIM)
FIM assesses the degree of independence in activities of daily living in six areas of function: self-care, mobility, sphincter control, locomotion, communication and social cognition.19 Respondents indicate on a Likert scale ranging from 1 (complete assistance needed) to 7 (completely independent) with higher scores indicating a greater level of independence. This measure has a good psychometric profile and has been favourably evaluated for use as a self-report measure in the SCI population.20
Hospital Anxiety and Depression Scale (HADS)
HADS enables detection of clinical cases and assessment of severity without contamination of scores through physical symptomology.21 Scores on Anxiety and Depression subscales can be obtained separately with higher scores indicating greater psychopathology. This measure has previously been validated for use in SCI populations.22
Quality of Life (WHOQoL-BREF)
An international, cross-culturally comparable QOL assessment instrument comprising of 26 items in four domains: physical health, psychological health, social relationships and environment.23 Higher scores on each subscale indicate a greater perceived QOL in that area. This measure has previously been used in the SCI population.24
Spinal Cord Injury Quality of Life Questionnaire (SCI QL-23)
The SCI QL-23 consists of 23 items that were found to best predict overall QOL in individuals with SCI.25 Two factors were used; problems regarding injury (PROB; six items), which was derived from a list of 10 questions26 describing perceptions of physical dependency (being unable to walk or move freely, needing help with many things, being unable to do things when wanted), of complications and of social stigma. Physical/social functioning (FUNC; 10 items) covers limitations in mobility, body care and movement and social interaction. High scores on the subscales of this measure represent limitations in SCI-related QOL.
Resource, coping and appraisal measures
The Stress-Related Growth Scale (SRGS-15)
The SRGS-15 is a 15-item measure of self-reported stress-related growth.27 SRGS items reflect positive changes in personal resources, social relationships and coping skills. Participants are asked to think about a stressful event in their life and respond to statements on a three-point scale. The SRGS-15 has a good internal consistency (Cronbach's alpha=0.94) and test–retest reliability over a 2-week period is acceptable (r=0.81). Higher scores indicate greater levels of stress-related growth.
Perceived Manageability Scale (PMnac)
This is a newly developed subscale of the Needs Assessment Checklist.28, 29 The perceived manageability subscale of the Needs Assessment Checklist consists of six items measuring how often an individual has certain feelings or beliefs about their injury and/or situation on a four-point scale. The scale aims to measure the extent to which an individual believes their situation is manageable, indicated by higher scores and is designed to be sensitive to change. This scale was shown to be psychometrically reliable with a Chronbach's alpha of 0.70 upon removal of item number five from the scale (0.64 with all items).28
Appraisal of Life Events Scale (ALE)
A checklist of 16 adjectives designed to elicit respondents’ cognitive appraisals of stressful life events in terms of threat, challenge and loss, with higher scores on subscales indicating the individual appraises the current situation in this way.30 It has been shown to have a good factor structure, good test-retest reliability, internal reliabilities and construct validity.30 The ALE questionnaire has previously been used in a SCI population.31
Spinal Cord Lesion-Related Coping Strategies Questionnaire (SCL CSQr)
This measure was developed specifically for use with individuals with SCI to explore coping processes and contains 12 items measuring three coping strategies: acceptance, fighting spirit and social reliance.32 Higher scores on a subscale indicate that the individual tends to use that coping strategy in response to a stressor. The scale has good psychometric properties and acceptable internal validity correlations and internal reliability coefficients for the three strategies. The questionnaire used in the present study contained amended wording of some questionnaire items, based on the findings of previous research.33
Selected subscales from the COPE
The COPE is a generic coping measure, which measures coping styles as opposed to situation-specific coping strategies.34 This measure has been successfully used with a SCI population.35 Three subscales found in previous research35 to be associated with adjustment were used: positive reinterpretation, behavioural disengagement and planning. Higher scores indicate the greater use of a particular coping style.
The Sense of Coherence Scale (SOC)
The SOC scale contains 13 items that measure ease of understanding, manageability and meaningfulness of stressful life situations.36 Higher scores indicate a stronger SOC and better-perceived health. This measure has previously been used in SCI populations.17
The Short Form Social Support Questionnaire (SSQ6)
This scale is a brief measure of perceived social support.37 It is a 6-item version of the original 27-item SSQ.38 The SSQ6 assesses two dimensions of social support; number of supports (a quasi-structural measure) and satisfaction with support (a global functional measure). The SSQ6 is reported to show satisfactory psychometric properties, with high internal consistency for both number and satisfaction subscales (alpha=0.90–0.93) and high test-retest reliability.38 Higher scores indicate a greater quantity of support and satisfaction with social support.
Demographic information
Questions to obtain the demographic information of gender, age and injury type.
Procedure
Data included in the current study is part of a longitudinal study looking at adjustment and coping during the first 2 years of injury. Participants were approached shortly after admission to the rehabilitation centres and once medically stabilised provided with an information leaflet about the study. Questionnaires were administered by a trained member of the Psychology team at 12 weeks post injury. In the UK, this time point is typically when patients begin their active rehabilitation in SCI rehabilitation centres. At 1 year post injury all participants had completed their active rehabilitation and were discharged from hospital, so questionnaires were sent by post at 1 year and 2 years post injury. Reminder letters were sent out to the participants to reduce attrition rates. Data was collected in a number of countries with one or more specialised centres and entered into a standardised template. Data was entered using coded strings and stored in accordance with ethical guidelines and data protection laws. Ethical approval for this study was obtained from each Centre's local research ethics committee. All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Data analysis
Data were analysed using the Statistical Package for Social Sciences. Data quality checks were performed to examine the distribution of measures and internal consistencies of the scales. Changes in measures over time were examined using paired sample t-tests. Correlation analyses were conducted to investigate the relationships between appraisals and coping variables with outcome measures. Stepwise regression analyses were performed on the outcome measures controlling for the effects of the sociodemographic variables of gender, age and injury type.
Results
Response rates
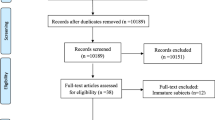
At 12 weeks post injury a total of 232 participants completed the questionnaires including 95 participants from the UK, 80 from Germany, 33 from Switzerland and 24 from Ireland. At 1 year post injury, 144 participants (60%) returned the questionnaires: 56 questionnaires were returned from the UK, 49 from Germany, 28 from Switzerland and 11 from Ireland. At 2 years post injury 90 questionnaires (38.8%) were returned. The UK returned 45, Germany returned 31 and Switzerland returned 14.
Demographics
Participants ranged in age from 18 to 74 with a mean age of 40. Most of the participants in the sample were men; at 12-weeks, 184 men (79.3%) and 48 women (20.7%) completed questionnaires, at 1 year post injury 114 men (79.2%) and 30 women (20.8%) returned questionnaires and at 2 years post injury the sample included 71 men (78.9%) and 19 women (21.1%).
Most of the sample (where injury data was provided) were categorised as having complete paraplegia (N=63, 32%) followed by incomplete tetraplegia (N=54, 27.4%), incomplete paraplegia (N=41, 20.8%) and complete tetraplegia (N=39, 19.8%) at 12 weeks post injury. At 1 year post injury, the majority of the sample were categorised as having complete paraplegia (N=51, 35.7%) followed by incomplete tetraplegia (N=42, 29.3) and complete tetraplegia and incomplete paraplegia (both groups N=25, 17.5%). Injury data was unavailable for one respondent at this time point. At 2 years post injury, the majority of this sample were classified as having complete paraplegia (N=32, 35.6%) followed by incomplete tetraplegia (N=28, 31.1%), incomplete paraplegia (N=17, 18.9%) and complete tetraplegia (N=13, 14.4%).
Changes in scores between time points
Means and s.d. of measures at 12 weeks, 1 year and 2 years post injury are displayed in Table 1.
The results in Table 1 indicate that most of the significant changes in the outcome measures occurred between 12 weeks and 1 year post injury, with little significant change occurring during the following year.
HADS anxiety and depression scores were grouped according to cut-off scores (0–7=non clinical case, 8–10=possible case, 11–21=clinical case) and percentages of participants falling into each category at the three time points are displayed in Table 2. No significant changes were observed in HADS scores at any of the three time points.
Relationship between appraisals, coping and outcome measures
Correlation analyses were conducted to investigate the relationships between appraisals and coping variables at 12 weeks post injury and outcome measures at 2 years post injury. Results of these analyses are displayed in Tables 3 and 4.
Significant relationships were evident between most appraisal and outcome measures, as shown in Table 3. Table 4 illustrates that the following coping strategies were significantly correlated with outcome measures: COPE positive interpretation (physical and psychological QOL, stress-related growth), SCLCSQ acceptance (psychological QOL, SCQoL problems regarding injury, anxiety and depression, stress-related growth), fighting spirit (psychological QOL, depression, stress-related growth) and social reliance (Physical QOL, SCQoL problems regarding injury, SCQoL physical and social functioning, depression).
To investigate the contribution of appraisals and coping strategies at 12 weeks post injury to the variance in psychological QoL, SCI-related QoL, anxiety, depression and stress-related growth at 2 years post injury, stepwise regression analyses were performed. To control for socio-demographic factors, neurological deficit and personal beliefs, the variables gender, age, injury type, SOC at 12 weeks and perceived manageability at 12 weeks were included among the potential predictor variables, which were stepwise regressed on psychological QOL, SCI-related QOL, anxiety, depression and stress-related growth at 2 years. Results are displayed in Table 5.
Individuals’ SOC scores and ‘challenge’ appraisals explained 41.3% of the variance in Psychological QoL at 2 years post injury. Perceived Manageability, ‘loss’ appraisals and social reliance coping strategies explained 34.9% of the variance in the individual's ratings of the problems they experienced regarding their injury (dependency and social stigma), whereas social reliance alone explained 30.2% of the variance in the problems they experienced related to physical functioning and social interactions. SOC explained 30.2% of the variance in anxiety, whereas SOC, challenge appraisals and gender explained 38.7% of the variance in depression. The coping strategy ‘acceptance’ explained 14.6% of the variance in stress-related growth.
Discussion
The current study explored the changes in and the relationships between appraisals and coping with mood, functioning and quality-of-life pre and post rehabilitation for acute SCI. It extended research by Kennedy et al.18 by exploring outcomes for this patient group at 2 years post injury.
A significant increase in the motor subscale of the FIM and in the total FIM score was observed from 12 weeks to 1 year post injury with no further increases between 1 and 2 years post injury. It seems that the participants in this sample tended to make most of the improvements in their functional independence during their stay in hospital.
Exploration of levels of anxiety and depression (HADS) revealed a slight increase in scores on both subscales from 12 weeks to 1 year post injury. Anxiety and depression scores decreased again at 2 years post injury. A similar pattern of results was observed when participants were grouped according to cut-off scores. This peak in emotional distress at 1 year post injury may be indicative of increased concerns regarding discharge into the community, and has been documented in previous studies.12 At 2 years post injury, the sample were found to be fairly psychologically well adjusted, with only around 20% of the sample scoring above clinical cut-off points for anxiety and depression. These levels are slightly elevated in comparison with the normal population.
There was a significant decrease in scores on the ‘Psychological’ and ‘Social’ subscales of the Quality of Life measure (WHOQoL-BREF) between 12 weeks and 1 year post injury; this may be related to the slight increase in observed scores on measures of anxiety and depression between these two time points. However, in contrast to score on the HADS, scores on the WHOQoL-BREF then remained stable from 1 year to 2 years post injury. With regard to Quality of Life specifically related to SCI (SCI-QL23), scores on the ‘problems regarding injury’ subscale did not change between 12 weeks and 1 year post injury but decreased significantly between 1 year and 2 years post injury. Scores on the ‘physical and social’ subscale decreased significantly between 12 weeks and 1 year but then remained stable at the 2 year follow-up.
Stress-Related Growth Scale scores remained stable over time. In the initial analysis of this sample, Kennedy et al.18 found an increase in SRG between 6 and 12 weeks post injury. This suggests that in this sample, the first 12 weeks following injury was the time period for patients to reflect on positive changes in personal resources, social relationships and coping skills.
Previous analysis of this sample18 and results from the current study revealed that, as with SRG, scores on measures of Perceived Manageability and the Appraisal of Life Events (ALE) questionnaires plateaued at 12 weeks, with no further increases observed at 1 and 2 years post injury. These findings highlight the importance of nurturing patients’ self-efficacy and positive appraisals during this time to facilitate adjustment and long-term psychological wellbeing.
When scores on the Coping Orientations to Problems Experienced (COPE) questionnaire were examined, significant changes were observed on all three subscales between the 12 week and 1 year post injury time points, with no significant changes at the 2-year follow-up. Participants were less likely to use positive reinterpretation and planning at 1 year, and more likely to use behavioural disengagement as a way of coping with their injury. Concerning the SCI-specific measure of coping strategies, the SCL CSQr, significant changes were observed between 12 weeks and 1 year post injury, with no significant changes at the 2-year follow-up. At 1 year post injury, participants were found to score lower in the domains ‘social reliance’ and ‘fighting spirit’. Although a reduction in both of these domains may appear counter intuitive, it may be that during the initial stage following injury, participants utilise strategies that are not usually required in everyday life and the reduction in ‘fighting spirit’ may signify a return to baseline levels. Scores on the SOC scale also changed between 12 weeks and 1 year, decreasing slightly between the two time points.
Between 12 weeks and 1 year post injury, the perceived quality and quantity of social support decreased significantly, remaining stable at the 2-year follow-up. The duration of SCI rehabilitation is lengthier than the majority of hospital admissions, and many people treated in specialist spinal centres are a long way from their home town. Patients appear to experience a change in their social-support network following injury, reporting that ‘you find out who your friends are’. The changes observed in the social-support scale may reflect such experiences.
Correlation analyses revealed significant relationships between the appraisals and coping strategies participants endorsed at 12 weeks post injury and emotional wellbeing at 2 years post injury. Regression analyses similarly suggested appraisal and coping variables to account for a significant proportion of the variance in psychological measures following discharge from the hospital environment. SOC was evident in the regression models for anxiety, depression and psychological Quality of Life, supporting the findings of previous research.17
The current study followed a cohort of patients who were receiving rehabilitation care at specialist SCI centres. Several significant results throughout the study highlight issues that may be relevant to clinical care and the provision of rehabilitation services. The study has provided further evidence for the relationship between appraisals, coping behaviour and subsequent adjustment to injury. Significant contributions to psychological variables, such as anxiety, depression and Quality of Life ratings, were made through SCI being appraised by the individual as a ‘loss’, whereas those who accepted their injury tended to report better psychological adjustment.
Not only were appraisals and coping behaviours linked to psychological adjustment, but also to physical quality-of-life and functional outcomes, supporting the findings of previous research.39 The passive and disengaged coping strategy ‘social reliance’ was found to be significant in explaining the variance in these outcome measures. Clinically, if patients are assessed using these measures prior to commencing active rehabilitation, those tending to see their injury as a loss or those patients prone to using passive and avoidant behavioural strategies to deal with the emotional sequelae of their injury could receive additional support, psycho-education or participate in Coping Effectiveness Training.40 This may encourage patients to reappraise their injury and bolster self-efficacy such that the occurrence of SCI is viewed as a manageable and unthreatening life event and one after which they can continue to participate fully in social activities.
A further clinically relevant observation was that scores on measures of appraisals and perceived manageability tended to plateau at 12 weeks in this sample. The relationship found between appraisals and rehabilitation outcomes supports the suggestion that early assessment of appraisals may be beneficial in order to provide suitable support and advice during rehabilitation.
The longitudinal design of this study was beneficial in assessing the role of appraisals and coping behaviour in adjustment to SCI. However, it would be useful for future research to follow up individuals with SCI over a longer time frame to investigate the influence of appraisals and coping throughout the lifespan. A major strength of the study is that it was conducted in a number of centres in Europe, including the UK, with participants that are representative of the SCI population, meaning that the findings may be relevant to many individuals with SCI. However, it is important to note that although European SCI centres operate in a similar manner to those in the UK, there may be differences in the rehabilitation process that were not recorded and could have had an impact on the results. Any differences should be considered in future multi-centre research in this area so that we can be aware of how rehabilitation practice might impact on the psychosocial variables measured in this study. Additionally, caution may need to be taken when applying these results to American individuals with SCI, as it is not yet known whether the comparatively short rehabilitation time for SCI in America would impact on the relationships between appraisals, coping and physical and psychological outcomes. Future research is required to answer this question.
A further limitation is the lack of data on individuals who refused to take part in the study or on those participants who dropped out over the 2 years. The longitudinal nature of this research resulted in significant attrition of the sample over time and unfortunately it was not possible to collect any information from these individuals. The lack of information about these individuals means we cannot be sure of the representativeness of our sample or of any impact on the generalisability of our findings. Furthermore, we cannot know whether the ‘non-completers’ score differently on measures of appraisals, coping, depression, anxiety, social support and so on, than those who participated. There is a possibility that those who did not participate or who dropped out were, for example, more depressed or used very different coping styles and these differences could have had an impact on the results. It is important that this information is collected in future research to ensure that the results are relevant to all individuals within the SCI population. In the current study, staffing resources meant that it was impossible to administer the follow-up questionnaires face to face. In-person follow-up may have minimised attrition rates throughout the 2-year period. Furthermore, this change in data collection may have had an impact on the results as at 1 and 2 years post injury, participants were in an environment that is less conducive to socially desirable responding.
In summary, the findings from this study provide further support for the relationships between psychological factors and subsequent adjustment to SCI over and above demographic and injury variables. The results may have clinical implications for the rehabilitation of individuals with SCI; suggestion was made for early assessment of appraisals and the delivery of interventions such as Coping Effectiveness training40 to address potentially unhelpful appraisals and coping strategies. Further, longitudinal research in different populations is required in order to add to these findings.
References
Martz E, Livneh H, Priebe M, Wuermser LA, Ottomanelli L . Predictors of psychosocial adaptation among people with spinal cord injury or disorder. Arch Phys Med Rehabil 2005; 86: 1182–1192.
Barker RN, Kendall MD, Amsters DI, Pershouse KJ, Haines TP, Kuipers P . The relationship between quality of life and disability across the lifespan for people with spinal cord injury. Spinal Cord 2009; 47: 149–155.
Lund ML, Nordlund A, Bernspång B, Lexell J . Perceived participation and problems in participation are determinants of life satisfaction in people with spinal cord injury. Disabil Rehabil 2007; 29: 1417–1422.
Westgren N, Levi R . Quality of life and traumatic spinal cord injury. Arch Phys Med Rehabil 1998; 79: 1433–1439.
Manns P, Chad K . Determining the relation between quality of life, handicap, fitness and physical activity for persons with spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1566–1571.
Carpenter C, Forwell SJ, Jongbloed LE, Backman CL . Community participation after spinal cord injury. Arch Phys Med Rehabil 2007; 88: 427–433.
Schonherr MC, Groothoff JW, Mulder GA, Eisma WH . Participation and satisfaction after spinal cord injury: results of a vocational and leisure outcome study. Spinal Cord 2005; 43: 241–248.
Hammell KW . Quality of life after spinal cord injury: a meta-synthesis of qualitative findings. Spinal Cord 2007; 45: 124–139.
North NT . The psychological effects of spinal cord injury: a review. Spinal Cord 1999; 37: 671–679.
Holicky R, Charlifue S . Aging with spinal cord injury: the impact of spousal support. Disabil Rehabil 1999; 21: 250–257.
Krause JS, Carter RE . Risk of mortality after spinal cord injury: relationship with social support, education, and income. Spinal Cord 2009; 47: 592–596.
Beedie A, Kennedy P . Quality of social support predicts hopelessness and depression post spinal cord injury. J Clin Psychol Med S 2002; 9: 227–234.
Galvin LR, Godfrey HPD . The impact of coping on emotional adjustment to spinal cord injury (SCI): Review of the literature and application of a stress appraisal and coping formulation. Spinal Cord 2001; 39: 615–627.
Kennedy P, Marsh N, Lowe R, Grey N, Short E, Rogers B . A longitudinal analysis of psychological impact and coping strategies following spinal cord injury. Br J Health Psychol 2000; 5: 157–172.
Hansen N, Tate D . Avoiding coping, perceived handicap, and coping strategies of persons with spinal cord injury. SCI Psychosoc Processes 1994; 7: 195.
Pollard C, Kennedy P . A longitudinal analysis of emotional impact, coping strategies and post-traumatic psychological growth following spinal cord injury: a 10-year review. Br J Health Psychol 2007; 12: 347–362.
Kennedy P, Lude P, Elfström M, Smithson E . Sense of coherence and psychological quality of life in people with spinal cord injury: appraisals and behavioural responses. Br J Health Psychol 2010; 15: 611–621.
Kennedy P, Lude P, Elfström M, Smithson E . Cognitive appraisals, coping and quality of life outcomes: a multi-centre study of spinal cord injury rehabilitation. Spinal Cord 2010; 48: 762–769.
Hamilton BB, Granger CV . Guide for the Use of the Uniform Data Set for Medical Rehabilitation. Research Foundation of State University of New York: Buffalo, NY, 1990.
Grey N, Kennedy P . The Functional Independence Measure: a comparative study of clinician and self ratings. Paraplegia 1993; 31: 457–461.
Zigmond AS, Snaith RP . The Hospital Anxiety and Depression Scale. Brit Med J Clin Res Ed 1986; 292: 344.
Kennedy P, Rogers BA . Anxiety and depression after spinal cord injury; A longitudinal analysis. Arch Phys Med Rehab 2000; 81: 932–937.
WHOQoL Group. Development of the World Health Organisation WHOQoL-BREF quality of life assessment. Psychol Med 1998; 28: 551–558.
Jang Y, Hsieh CL, Wang YH, Wu YH . A validity study of the WHOQoL-BREF assessment in persons with traumatic spinal cord injury. Arch Phys Med Rehab 2004; 85: 1890–1895.
Lundqvist C, Siösteen A, Sullivan L, Blomstrand C, Lind B, Sullivan M . Spinal cord injuries: a shortened measure of function and mood. Spinal Cord 1997; 35: 17–21.
Lundqvist C, Siösteen A, Blomstrand C, Lind B, Sullivan M . Spinal cord injuries. Part 1: clinical, functional, and emotional status. Spine 1991; 16: 78–83.
Park CL, Cohen LH, Murch RL . Assessment and prediction of stress-related growth. J Pers 1996; 64: 71–105.
Kennedy P, Scott-Wilson U, Sandhu N . The psychometric investigation of a brief and sensitive measure of perceived manageability. Psychol Health Med 2009; 14: 454–465.
Kennedy P, Hamilton LR . The needs assessment checklist: a clinical approach to measuring outcome. Spinal Cord 1999; 37: 136–139.
Ferguson E, Matthews G, Cox T . The appraisal of life events (ALE) scale: reliability and validity. Br J Health Psychol 1999; 4: 97–116.
Kennedy P, Lude P, Taylor N . Quality of life, social participation, appraisals and coping post spinal cord injury: a review of four community samples. Spinal Cord 2006; 44: 95–105.
Elfström ML, Rydén A, Kreuter M, Persson LO, Sullivan M . Linkages between coping and psychological outcome in the spinal cord lesioned: development of SCL-related measures. Spinal Cord 2002; 40: 23–29.
Elfström ML, Kennedy P, Lude P, Taylor N . Condition-related coping strategies in persons with spinal cord lesion: a cross-national validation of the Spinal Cord Lesion-related Coping Strategies Questionnaire in four community samples. Spinal Cord 2007; 45: 420–428.
Carver CS, Scheier MF, Weintraub JK . Assessing coping strategies; a theoretically-based approach. J Pers Soc Psychol 1989; 56: 267–283.
Kennedy P, Lowe R, Grey N, Short E . Traumatic spinal cord injury and psychological impact: A cross-sectional analysis of coping strategies. Br J Clin Psychol 1995; 34: 627–639.
Antonovsky A . The structure and properties of the sense of coherence scale. Soc Sci Med 1993; 36: 725–733.
Sarason I, Levine HM, Basham RB, Sarason BR . Assessing social support: the Social Support Questionnaire. J Pers Soc Psychol 1983; 44: 127–139.
Sarason BR, Shearin EN, Pierce GR, Sarason IG . Interrelationships of social support measures; theoretical and practical implications. J Pers Soc Psychol 1987; 52: 813–832.
Kennedy P, Smithson E, McClelland M, Short D, Royle J, Wilson C . Life satisfaction, appraisals and functional outcomes in spinal cord injured people living in the community. Spinal Cord 2010; 48: 144–148.
Kennedy P, Duff J, Evans M, Beedie A . Coping effectiveness training reduces depression and anxiety following traumatic spinal cord injuries. Br J Clin Psychol 2003; 41: 41–45.
Acknowledgements
The authors give their appreciation and thanks to all of the patients who participated in the study. Thanks to Margareta Kreuter for her help in the planning of the study, Yvonne Lude for her valuable assistance during the research and Laura Blakey who assisted in the preparation of this manuscript. We also thank those who gave their time to help with the recruitment and questionnaire process and to all the staff at the specialist spinal injury units involved with this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kennedy, P., Lude, P., Elfström, M. et al. Appraisals, coping and adjustment pre and post SCI rehabilitation: a 2-year follow-up study. Spinal Cord 50, 112–118 (2012). https://doi.org/10.1038/sc.2011.127
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.127
Keywords
This article is cited by
-
Cognitive appraisals of disability in persons with traumatic spinal cord injury: a scoping review
Spinal Cord (2022)
-
Regaining A Sense Of Me: a single case study of SCI adjustment, applying the appraisal model and coping effectiveness training
Spinal Cord Series and Cases (2021)
-
The associations of acceptance with quality of life and mental health following spinal cord injury: a systematic review
Spinal Cord (2020)
-
Forgiveness and acceptance of disability in people with traumatic spinal cord injury—the mediating role of disability appraisal. A cross-sectional study
Spinal Cord (2020)
-
Sense of coherence is linked to post-traumatic growth after critical incidents in Austrian ambulance personnel
BMC Psychiatry (2019)