Abstract
Study design:
Cross-sectional, observational and longitudinal.
Objectives:
The aim of the study was to analyze the relationship between pain intensity, plasma lipids and severity of spinal cord injuries in patients with paraplegia (n=11), tetraplegia (n=16) and polytrauma (n=15). We concentrated on the hospitalization period immediately following injury.
Methods:
Pain intensity was assessed on a visual analog scale immediately after patients were transported to hospital, again 14 days after injury and before discharge from hospital. Blood samples were also obtained at these same times. We measured following biochemical parameters: total protein, albumin, total cholesterol, HDL cholesterol, LDL cholesterol, triglycerides, glycemia, and C-reactive protein. Data were analyzed with respect to type of injury, state of unconsciousness immediately after injury, hemorrhage, measure of liability (self-inflicted injuries vs casualties), cause of the accident and pre-injury cholesterol levels.
Results:
On the day of injury, pain intensity correlated positively with HDL cholesterol (r=0.48, P=0.04); on the day of discharge from hospital, pain intensity correlated positively with blood glucose levels (r=0.67, P=0.0002). Diagnostic subgroups did not differ either in pain intensity or in pain dynamics during hospitalization. Total cholesterol level was lowest in patients with polytrauma. In all patients, the lowest total cholesterol level was observed immediately after injury. HDL cholesterol was highest after injury.
Conclusion:
After spinal cord injury, lower total cholesterol levels reflected more serious trauma intensity and HDL cholesterol predicted more intensive pain. Subjects responsible for their own injuries suffered less intensive pain than those who were not responsible for their injuries.
Similar content being viewed by others
Introduction
In our previous experimental and clinical studies we described that some parameters of lipid, saccharide and protein metabolism mostly increase during nociceptive stimulation and acute pain processes.1, 2
Clinical studies in patients with spinal cord injuries mostly deal with the consequences of long-term immobilization and development of chronic pain.3 However, the situation immediately after injury is different, as the levels of plasma lipids represented by total cholesterol are, on the contrary, relatively low.
The low cholesterol levels have frequently been reported in association with suicidal behavior.4 Lower cholesterol levels may weaken serotonergic functions and consequently trigger increased aggressive or auto-aggressive behavior. In addition, individuals with auto-aggressive behavior, manifested by self-mutilation or self-injury, have also been observed to have lower cholesterol levels in comparison with control subjects.5
Self-injury behavior tends to be accompanied by lower pain sensitivity and higher pain thresholds. Pain perception has also been observed to be reduced in those who have survived suicide attempts.6
The aim of our study was to analyze the relationship between pain intensity and levels of plasma lipids as they relate to the severity of injury in patients with spinal cord trauma. We tested the hypothesis that subjects with lower total cholesterol levels experience lower pain intensity.
Patients and methods
When evaluating injuries to patients and the severity of clinical conditions, we followed the recommendations for the study of spinal cord injuries in humans.7
Our sample consisted of 42 patients: paraplegia (n=11), tetraplegia (n=16), and polytrauma (n=15). Four patients out of the group died (on average 26 days after their injury). The spinal cord injuries were caused by car accidents, motorcycle or biking accidents, falls from high places, jumps to water or other causes. On hospitalization, 13 patients were unconscious as a consequence of craniocerebral injuries. Diagnostic groups had a similar average age, roughly 38 years old. There were 35 men and 7 women in the sample. Women did not differ from men in any of the investigated items; therefore it was possible to analyze both sexes together. Demographic descriptions of the patient sample are shown in Table 1.
The intensity of pain was evaluated on a visual analog scale VAS (10 cm line segment). Levels of total cholesterol, LDL and HDL cholesterol, triglycerides, total proteins, albumin, glycemia and CRP were analyzed using standard biochemical laboratory methods. Patients had 5 ml blood samples taken (i) immediately after their arrival at hospital (within several hours of the injury), (ii) after 2 weeks, and (iii) before discharge. Pain intensity was also evaluated at these same three times; pain intensity was either marked by the patient themselves, or in the case of tetraplegic patients, with the assistance of a doctor according to the patient's instructions. The first measurement of pain could not be carried out on patients who were brought to hospital unconscious; however, blood samples were taken.
During hospitalization the patients received standard analgesic treatment. Post-traumatic and, if necessary, post-surgical pain was alleviated with varying combinations of weak opioids (piritramid, tramadol) and non-opioid analgesics (paracetamol, metamizol, nimesulid), antidepressants (sertralin, mirtazepin, citalopram), antipsychotics (ziprasidon) myorelaxants (baclofen), and anxiolytics (bromazepam).
Data analysis
The data were analyzed using the non-parametric Kruskal–Wallis test. Changes in pain intensity and changes in biochemical data were compared: (1) in patients with different levels of lesion and severity of injury (paraplegia, tetraplegia, polytraumas); (2) depending on the state of unconsciousness immediately after injury; (3) depending on the degree of hemorrhage; (4) depending on the measure of liability (self-inflicted injuries vs casualties); (5) cause of the accident (dives, falls from height, car accidents and biking accidents) and (6) depending on pre-injury cholesterol levels (if it could be determined from the patients’ previous medical records or if it was known by the patients themselves). When indicated, simple effects were computed using post hoc analyses.
The relationship between pain and biochemical data at the beginning and at the end of the treatment was determined using Pearson's correlation coefficients.
Results
Clinical factors influencing biochemical values
The length of hospitalization was shorter in paraplegia (34.2 days) and tetraplegia (39.7 days) than in polytraumas (62.7 days) (F(1,36)=6.1; P=0.02).
The level of lesion and severity of injury
The mean values for individual diagnostic groups are summarized in Table 2.
Paraplegic patients did not differ from tetraplegics in any variables except for HDL cholesterol levels immediately after admission to hospital. Compared with normal physiological values, HDL cholesterol as a whole was lower in all groups. In all groups the highest levels were observed immediately after injury, followed by a gradual decline in values. The initial level of HDL cholesterol did not differ from normal values in paraplegic patients (Figure 1).
Total cholesterol was the lowest in patients with polytraumas. In all groups, cholesterol levels were lowest immediately after injury (Figure 2). Although the level of cholesterol gradually increased during hospitalization, it remained relatively low. LDL cholesterol behaved in a similar way, but there were no significant differences between groups.
Changes in total cholesterol levels in diagnostic groups. The arrows mark the lower and upper limits of normal (physiological) cholesterol values. Immediately after injury, all groups of patients, except of paraplegics, had cholesterol levels below the lower limit for normal values. Even though cholesterol levels gradually increased, they nevertheless remained low. *P<0.05; **P<0.01.
There were no differences between groups with regard to triglyceride levels. During hospitalization, however, they increased significantly in all groups (F(2,54)=4.6, P=0.014).
Total protein was lower in all groups and followed a similar pattern; with the lowest protein levels being in polytrauma patients immediately after injury. During hospitalization these values increased, reaching normal values by the time of hospital discharge. Albumin levels were at their lowest levels 14 days after injury.
Blood glucose and CRP were significantly increased after injury in all groups. In polytrauma patients, the elevated glucose levels and CRP were still present 14 days after injury. At discharge from hospital, glucose values, as well as CRP, had decreased significantly compared with initial values.
Diagnoses did not differ with regard to pain intensity and its dynamics during hospitalization, that is, high VAS scores were observed both on admission to hospital and 14 days later. However, at discharge from hospital, VAS scores were significantly lower in all groups (Figure 3).
Craniocerebral trauma
The patients who were unconscious after injury had lower total cholesterol levels than patients who did not lose consciousness (3.2 mmol l−1 vs 3.9 mmol l−1, F(1,32)=4.8, P=0.04), lower albumin levels (33 g l−1 vs 37 g l−1, F(1,28)=6.0, P=0.02), higher levels of triglycerides (1.76 mmol l−1 vs 1.25 mmol l−1, F(1,33)=4.74, P=0.04), and higher CRP (130 mg l−1 vs 50 mg l−1, F(1,31)=10.95, P=0.002). There were no significant differences found in other values.
In patients who were unconscious on admission to hospital, the first data concerning pain intensity are, of course, missing. Further comparisons did not show any connection between unconsciousness and the intensity of pain.
Hemorrhage
Patients with hemorrhages had lower albumin levels at admission than patients without hemorrhages (35.8±5.9 g l−1 vs 41.7±6.2 g l−1, H(1,42)=7.92, P=0.005) and the situation remained unchanged over the following 14 days (H(1,35)=3.32, P=0.06).
Patients with bleeding did not differ with regard to pain intensity at admission (35.5±13.7 vs 32.4±15.6, H(1,29)=0.75, P=0.4) or at discharge from hospital (19.2±9.7 vs 17.2±10.6, H(1,30)=0.07, P=0.8).
Psychological and other factors influencing biochemical values
Measure of liability for injury
The persons who were liable for their own injury (that is, the injury was their own fault) had lower HDL cholesterol levels directly after injury compared with those who were not responsible for their injuries (1.2±0.29 mmol l−1 vs 2.1±0.13 mmol l−1, H(1,24)=4.6, P=0.03).
Patients who were responsible for their own injuries also reported lower pain intensity immediately after the injury compared with those who were not responsible for their injuries (32.2±14.0 vs 54.0±4.2, H(1,29)=4.3, P=0.04).
Causes of accidents
When comparing age and weight of patients, there were no differences between those whose injuries were caused by jumps into water, jumps from high places, car accidents or biking accidents (age: KW(3,42)=2.88, P=0.41; weight: KW(3,36)=2.07, P=0.5).
Compared with other causes of injuries, we observed an increase in CRP in injuries caused by car accidents (14 days after the accident F(1,29)=5.67, P=0.02) and an increase in triglycerides before discharge (F(1,28)=7.92, P=0.009).
After transport to hospital, car accident patients had the lowest cholesterol levels compared with other groups (F(1,37)=5.24, P=0.03).
There were no differences, with regard to pain intensity, between the different causes of injuries.
Pre-injury cholesterol levels
As levels of total cholesterol before injury might have significantly influenced other values in the lipid spectrum, we evaluated the measured data in light of this fact. Patients with higher pre-injury total cholesterol also had a higher value immediately after injury compared to persons with normal pre-injury cholesterol (4.05±1.21 mmol l−1 vs 3.24±0.72 mmol l−1, H(1,41)=4.8, P=0.02).
Patients with higher pre-injury levels of cholesterol were older (58.6±16.5 years vs 33.2±13.8 years, H(1,42)=11.1, P=0.0009) and had a higher body weight (90.0±11.8 kg vs 74.5±15.6 kg, H(1,36)=4.8, P=0.02).
Correlation of pain intensity with biochemical values
The intensity of pain at admission correlated only with the level of HDL cholesterol (r=0.48, P=0.04) (Figure 4). In addition, pain correlated positively with body weight (r=0.43, P=0.024) and less significantly with LDL cholesterol level (r=0.4027, P=0.087). The higher the levels of HDL and LDL cholesterol and body weight the patients had, the more pain they perceived. At discharge, the intensity of pain correlated positively with blood glucose (r=0.67, P=0.0002) (Figure 5).
Discussion
Most studies dealing with biochemical and hormonal changes following spinal cord trauma evaluate the period from several months to several years after the trauma.8, 9, 10 In our study, however, we concentrated on the hospitalization period immediately following injury.
Our study confirmed findings that as a consequence of severe spinal cord trauma, levels of plasma lipids decrease immediately after injury undergoing significant dynamic changes during a relatively short period of time. Low levels of plasma lipids, in particular cholesterol, have been described in severe trauma, burns and serious infections. Hypocholesterolemia in these patients may be considered a significant prognostic marker of mortality.11 The causes of hypocholesterolemia may be explained by a lower production of cholesterol precursors in the liver, by faster catabolism or faster utilization by damaged tissues during regeneration but not caused by simple hemodilution.12, 13
Elevation in lipid levels during hospitalization can be explained by reduced mobility, or a radically changed lifestyle and quality of life. Chronically elevated lipid levels represent a significant risk factor for development of cardiovascular diseases in patients with spinal cord injuries.14 Some studies point out that patients undergoing physiotherapy have, during hospitalization, a better course with regard to levels of HDL cholesterol, which increased in these patients.15 On the other hand long-term immobilization (longer than 15 years) lowers the levels of HDL cholesterol.16
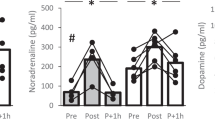
In our study, pain intensity did not differ between patients with different lesion levels or in patients who suffered a craniocerebral injury as a consequence of their accident. The best predictor of pain intensity at the time of admission to hospital proved to be HDL and LDL cholesterol levels, which correlated positively with the intensity of pain. HDL and LDL cholesterol proved to be positively correlated with levels of adrenalin and noradrenalin.9 This means that activity of the sympathetic nervous system is reflected in the levels of plasma lipids. Our results showed that pain intensity immediately after injury was related to HDL cholesterol levels, which might have been influenced by the sympathetic nervous system being activated by injury-associated stress. The decrease in HDL cholesterol over the course of hospitalization can perhaps be explained by the lower levels of catecholamines brought on by interruption of the spinal cord. Studies have shown that tetraplegics have lower adrenalin and noradrenalin levels, whereas low-lesion paraplegics have higher adrenalin and noradrenalin levels than high-lesion paraplegics or control subjects.9
At the time of discharge from hospital, pain intensity was correlated with blood glucose levels. Experiments with animals have shown that glycemia is a good indicator of stress intensity.17 In our study, the degree of glycemia apparently reflected not only pain intensity, but also the level of long-term stress brought about by the injury.
On the day of injury, the most severe pain was felt by patients who were not responsible for their injuries. On the other hand, patients who were, at least in part, responsible for their injury due to hazardous behavior, suffered less. However, there is a parallel with experimentally induced pain. If nociceptive stimuli are applied by another person, pain thresholds are lower than when the stimuli are applied by the experimental subject themselves.18 Also, preparedness for pain may have a role. Such preparedness might have been present in patients who suffered their injury while engaging in a risky activity.
Our study raises several questions, which need further study: (1) Whether low cholesterol levels increase hazardous behaviors in general; (2) Whether low cholesterol levels are a cause or a consequence of hazardous behavior, or perhaps both? (3) If we consider the association between pain intensity and HDL cholesterol, we cannot rule out the effect of treatment or acute stress. There is evidence that one of the mechanisms which participates in the rise of cholesterol levels during stress is the opioid system.19 Blockade of the opioid system by naltrexone, before stress, suppresses an increase in cholesterol levels, whereas administration of morphine will, by itself, increase the level of cholesterol in the absence of stress.20
Conclusions
Our results suggest that total cholesterol levels reflect the severity of the trauma. On the other hand, the severity of the trauma was not associated with pain intensity. We did not find a direct connection between pain intensity and total cholesterol levels. Immediately after injury pain intensity correlated positively with HDL cholesterol levels and at discharge from hospital with glycemia. Besides the mentioned markers, we found that the intensity of experienced pain was also influenced by psychological factors, that is, persons responsible for their injuries experienced less intensive pain on the day of injury.
References
Krikava K, Kalla K, Yamamotová A, Rokyta R . Blood serum changes in patients with pain during bone fractures and acute pancreatitis. Neuroendocrinol Lett 2004; 25: 62–69.
Rokyta R, Yamamotová A, Sulc R, Trefil L, Racek J, Treska V . Assessment of biochemical markers in patients with pain of vascular origin. Clin Exp Med 2008; 8: 199–206.
Jensen MP, Hoffman AJ, Cardenas DD . Chronic pain in individuals with spinal cord injury: a survey and longitudinal study. Spinal Cord 2005; 43: 704–712.
Engelberg H . Low serum cholesterol and suicide. Lancet 1992; 339: 727–729.
Florkowski A, Gruszczynski W, Wawrzyniak Z . Selected biochemical parameters of blood serum in soldiers committing self-mutilation. Mil Med 2001; 166: 375–377.
Orbach I, Mikulincer M, King R, Cohen D, Stein D . Thresholds and tolerance of physical pain in suicidal and nonsuicidal adolescents. J Consult Clin Psychol 1997; 65: 646–652.
Anderson DK, Beattie M, Blesch A, Bresnahan J, Bunge M, Dietrich D et al. Recommended guidelines for studies of human subjects with spinal cord injury. Spinal Cord 2005; 43: 453–458.
Campagnolo DI, Bartlett JA, Chatterton R, Keller SE . Adrenal and pituitary hormone patterns after spinal cord injury. Am J Phys Med Rehabil 1999; 78: 361–366.
Schmid A, Halle M, Stutzle C, Konig D, Baumstark MW, Storch MJ et al. Lipoproteins and free plasma catecholamines in spinal cord injured men with different injury levels. Clin Physiol 2000; 20: 304–310.
Vidal J, Javierre C, Curia FJ, Garrido E, Lizarraga MA, Segura R . Long-term evolution of blood lipid profiles and glycemic levels in patients after spinal cord injury. Spinal Cord 2003; 41: 178–181.
Kamolz L-P, Andel H, Mittlböck M, Winter W, Haslik W, Meissl G, Frey M . Serum cholesterol and triglycerides: potential role in mortality prediction. Burns 2003; 29: 810–815.
Bakalar B, Zadak Z, Pachl J, Eidam M, Hyspler R, Crhova S . Hypocholesterolemia after multiple injuries is not caused by simple hemodilution. Rozhl Chir 2001; 80: 67–71.
Bakalar B, Hyspler R, Pachl J, Zadak Z . Changes in cholesterol and its precursors during the first days after major trauma. Wien Klin Wochenschr 2003; 115: 775–779.
Bauman WA, Spungen AM . Coronary heart disease in individuals with spinal cord injury: assessment of risk factors. Spinal Cord 2008; 46: 466–476.
de Groot S, Dallmeijer AJ, Post MW, Angenot EL, van den Berg-Emons RJ, van der Woude LH . Prospective analysis of lipid profiles in persons with a spinal cord injury during and 1 year after inpatient rehabilitation. Arch Phys Med Rehabil 2008; 89: 531–537.
Bauman WA, Adkins RH, Spungen AM, Herbert R, Schechter C, Smith D et al. Is immobilization associated with an abnormal lipoprotein profile? Observations from a diverse cohort. Spinal Cord 1999; 37: 485–493.
Armario A, Marti J, Gil M . The serum glucose response to acute stress is sensitive to the intensity of the stressor and to habituation. Psychoneuroendocrinology 1990; 15: 341–347.
Brad L, Cahusac PMB . Decreased sensitivity to self-inflicted pain. Pain 2006; 124: 134–139.
Bryant HU, Kuta CC, Story JA, Yim GK . Stress- and morphine-induced elevations of plasma and tissue cholesterol in mice: reversal by naltrexone. Biochem Pharmacol 1988; 37: 3777–3780.
Bryant HU, Story JA, Yim GK . Assessment of endogenous opioid mediation in stress-induced hypercholesterolemia in the rat. Psychosom Med 1988; 50: 576–585.
Acknowledgements
This study was founded by Research Goal MSM 0021620816.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yamamotová, A., Šrámková, T. & Rokyta, R. Intensity of pain and biochemical changes in blood plasma in spinal cord trauma. Spinal Cord 48, 21–26 (2010). https://doi.org/10.1038/sc.2009.71
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.71
Keywords
This article is cited by
-
The Identification of Blood Biomarkers of Chronic Neuropathic Pain by Comparative Transcriptomics
NeuroMolecular Medicine (2022)
-
Upregulation of Inflammatory Mediators in a Model of Chronic Pain after Spinal Cord Injury
Neurochemical Research (2011)