Abstract
Objective:
To determine the efficacy and safety of sacral neuromodulation (SNM) in incomplete spinal cord injured (SCI) subjects affected by neurogenic lower urinary tract symptoms (NLUTS).
Methods:
Twenty-four SCI patients were enrolled. The individuals were divided into two groups: 13 individuals in the urinary retention category and 11 suffering from overactive bladder syndrome. All subjects underwent definitive SNM implantation (Medtronic, Inc.). Voiding symptoms were assessed using patient bladder diaries, which recorded both pre-SNM and before each follow-up (1, 3 and 6 months, and then every 6 months). Outcome measures were per 24 h: number of voids and voided volume per void for both groups; number of urinary leakages, pad use and nocturia for patients with overactive bladder syndrome; and volume per catheterization and number of catheterizations for urinary retention subjects only. Final checkups were completed by June 2008.
Results:
Median follow-up was 61 months. Up to the final visit, all subjects maintained a clinical improvement of more than 50% compared with baseline. Twenty-two side effects were recorded. Four subjects with urinary retention needed a new implant in the controlateral S3 sacral root because of loss of efficacy. One patient with urinary retention developed a wound infection at the implanted pulse generator site.
Conclusions:
Our study contains the largest series of implanted SCI patients ever published. SNM is a therapy to consider in the treatment of NLUTS for partial SCI patients, even if the loss of clinical benefits for patients with retentive NLUTS must be taken into account. All adverse events were treated effectively.
Similar content being viewed by others
Introduction
In the past, renal failure was the leading cause of death after spinal cord injury (SCI). Today, mortality from SCI has declined dramatically, partly because of the improved management of urological dysfunction associated with SCI.1 Over the past 20 years, sacral neuromodulation (SNM) has become an established treatment option for lower urinary tract symptoms (LUTS). In 1981, the SNM technique for treatment of bladder dysfunctions was first developed by Tanagho and Schmidt, and has since been refined.2 The introduction of an innovative percutaneous second stage implantation technique has increased the number of candidates for SNM, including those of neurogenic origin. This is because of the fact that, in the first stage, only the permanent electrode is implanted in the sacral S3 root and connected to a temporary external stimulator, allowing patients to be assessed for a longer period (minimum 1 month) and with a more accurate evaluation of possible clinical enhancement as the risk of lead migration with the peripheral nerve evaluation (PNE) test is eliminated.3 If the main symptoms improve by more than half during the first stage, compared with baseline, the patient proceeds to the second stage, the insertion of the implantable pulse generator (IPG). The range of SNM indications has been extended continuously beyond voiding disorders. These additional benefits have included re-establishment of pelvic floor muscle awareness and normalization of bowel function. More recently, literature documents the positive effects of SNM on sexuality in a heterogeneous group of female subjects, including spinal cord patients, when the method was used with the intent of improving neurogenic lower urinary tract symptoms (NLUTS).4 However, information about SNM efficacy and adverse events in subjects with LUTS of neurogenic origin is sparse, and includes few individuals with a range of various neurological pathologies responsible for LUTS. Moreover, literature reports contrasting results in people with neurogenic bladder dysfunctions, even though the group consists of a restricted number of patients with a short follow-up.5, 6 Nevertheless it has been shown recently that these patients are able to gain remarkable clinical and long-term benefits from SNM.7 The aim of this study was to evaluate efficacy and complications in a medium and long-term follow-up for partial SCI patients treated with SNM for chronic NLUTS.
Methods
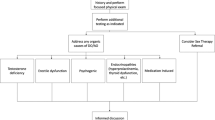
This is a retrospective study in incomplete spinal cord lesion patients with lower urinary tract symptoms refractory to conservative therapies, who underwent implantation of the SNM system (Medtronic, Inc.). Between January 1997 and January 2007, a total of 24 SCI patients (14 male, 10 female, mean age 46±12 years) underwent definitive SNM implantation. Four patients (16.7%) were permanently implanted during the original single surgical procedure. One patient (4.2%) underwent a two-stage ‘buttock’ procedure in which, during the second stage, the position of the implantable pulse generator was changed with respect to the original single surgical procedure from the subcutaneous pocket at the lower part of the anterior abdominal wall to the buttock.8 The remaining 19 individuals (79.1%) were implanted using the percutaneous second stage procedure. All patients underwent placement of unilateral implantation in the sacral S3 root. All SCI subjects underwent a physical examination, urine test, renal blood examination, bladder and kidney scans and a complete video-urodynamic investigation (uroflowmetry, cystometry, pressure/flow and external sphincter electromyography) before the peripheral nerve evaluation test. All methodologies of measurement and definitions were on the basis of the definitions of the International Continence Society 2002.9
Exclusion criteria
Age <18 years, known stress incontinence, presence of urological complications (such as bladder stones and vesico-ureteral reflux) and an abnormal serum creatinine level (normal: 0.8–1.4 mg 100 ml–1). Individuals with anatomical changes of the os sacrum (such as spina bifida), sacral agenesis and anatomical anomalies of the urinary tract. Subjects with a history of psychiatric conditions and those manifesting psychiatric disorders according to the Minnesota Multiphasic Personality Inventory questionnaire, and individuals with neurological diseases other than SCI.
Inclusion criteria
Inclusion criteria for SNM surgery were individuals with partial spinal cord lesions. The American Spinal Injury Association/International Medical Society of Paraplegia impairment scale was used to classify patients according to injury severity. Neurological assessment was done by a professional neurologist to determine stability of the case, and level and incompleteness of injury.10
The individuals were divided according to their urinary complaints: the urinary retention group consisted of 13 individuals, whereas 11 suffered from overactive bladder syndrome.
Voiding symptoms were assessed using patient bladder diaries, which recorded 7 days both pre-SNM and before each follow-up. The efficacy of the SNM therapy was measured by voiding diary parameters per 24 h, and consisted of number of voids, voided volume per void, number of urinary leakages, pad use and nocturia for the urge category, whereas the retention category recorded number of voids, voided volume per void, urine volume per catheterization and number of clean intermittent self-catheterization. The following data were collected from the implanted patients' files: type of complaints, date of definite implantation, complete clinical results from baseline through final checkup, number of adverse events and whether they had sucessfully been addressed, and date of successive surgeries needed because of adverse events.
Patients submitted to the original single surgical procedure had reached a clinical improvement of at least 50% in voiding symptoms during a 7–14-day peripheral nerve evaluation test. Individuals who were submitted to a two-stage procedure using the InterStim system (Medtronic Inc.) reached an improvement in their urinary symptoms of at least 50% during the first stage, which lasted a minimum of 1 month, and returned to baseline condition when stimulation was discontinued. SCI subjects were included if they had a follow-up of longer than at least 12 months after permanent SNM implantation and if complete data were available. Follow-ups were scheduled at 1, 3 and 6 months, and then every 6 months, during which the stimulus parameters such as the amplitude in volts, pulse width (in μs) and rate, mode (cycling versus continuous) and possible battery depletion were telemetrically checked.
The patients were encouraged to contact the clinic when they suspected neuromodulation-related complaints. Battery depletion of IPG was recorded separately from any complications.
Statistical analysis
All tests used for data analysis were performed assuming a maximum α error of 5% (P<0.05). Analysis of results was done using the Wilcoxon test to compare the parameters selected for the NLUTS pre-SNM and during follow-up.
The study was conducted after consultation with the local ethical committee, which approved the study protocol. All participants provided written informed consent before enrolment, and the study was conducted in accordance with the regulatory standards of Good Clinical Practice and the Declaration of Helsinki (1996).
Results
Mean time from neurological diagnosis to SNM therapy was 5.4 years (range 1–12 years). Mean follow-up period from permanent implant to final visit was 60.7 months (range 18–132 months). SCI subjects in both groups presented C or D degrees of lesion according to the American Spinal Injury Association/International Medical Society of Paraplegia. The etiology of SCI was mainly traumatic: 69.2% in the urinary retention group and 72.7% in the urge category. Details of injury and etiology of SCI are reported in Table 1.
Urinary retention category
Before the peripheral nerve evaluation test, all subjects performed clean intermittent self-catheterization with a frequency of two to maximum five times daily. Four out of 13 patients (30.7%) were able to void (more than 50 ml per void) using the Valsalva manoevre with elevated post-void residual urine volume, whereas the remaining nine (69.3%) had complete urinary retention and emptied their bladders exclusively with intermittent catheterizations. A urodynamic evaluation at baseline showed detrusor underactivity in all patients, and two of them presented non-relaxing urethral sphincter obstruction as well. The mean maximum flow rate was 2.1 with ±3.3 s.d. and range 0–8.
Table 2 shows average voiding improvement compared with baseline by means of parameters selected in the first follow-up and final post-SNM visit. In all follow-ups, all but four patients with detrusor underactivity manifested a clinical improvement of at least 50% compared with baseline. In four subjects, three of whom were men with median follow-up of 40.7 months (range 26–59), clinical benefits immediately disappeared with the need for catheterization because of elevated post-void residual urine or inability to void. Neither a worsening of neurological status, nor a malfunction of IPG nor a breakage or displacement of the sacral eletrocatheter was detected. Several attempts at reprograming the stimulus parameters failed. Urodynamic findings showed, in all the four subjects, the presence of detrusor underactivity much similar to that at baseline. A possible bladder outlet obstruction was excluded in three males by measuring prostate volume through transabdominal ultrasonography, whereas a clinical examination did not reveal a cystocele in the female.
In the four non-responding individuals, a new peripheral nerve evaluation test, lasting a minimum of 7 days, and the first stage in the controlateral S3 sacral root led to a remarkable clinical improvement in more than 50% of them. The median time from the new definitive implant to the final visit was 34 months (range 14–69). In the final video-urodynamic evaluation, the mean maximum flow rate was 12.3 with ±4.1 s.d. (range 7–20) with P<0.05 using the Wilcoxon test compared with that at baseline. In addition, in all follow-ups post-SNM, 5 out of 13 patients (38.5%) showed a normal bladder contractility index with a score of more than 100. Post-SNM, normal urethral function was always noted in the two patients with non-relaxing urethral sphincter obstruction before SNM.
Figure 1 reports the percentage of reduction in catheterization use from the first to final observation for the urinary retention group.
Six revisions for battery depletion were needed for six patients. The mean life span of the replaced IPGs in these patients was 63 months (range 54–79).
Overactive bladder syndrome category
Before the peripheral nerve evaluation test, urodynamic studies showed, during the filling phase, the presence of neurogenic detrusor overactivity in all subjects. While voiding, 2 out of the 11 patients (18.2%) showed grade 1 and grade 2 detrusor sphincter dyssynergia, respectively, according to the Blaivas classification. All emptied <50 ml of low residual urine. At baseline, all but four patients had urge urinary incontinence with daily pad use.
Table 3 summarizes the average modification of voiding parameters in the first follow-up and final visit measured against baseline. In particular, a remarkable percentage reduction in the mean daytime frequency was observed after SNM. (see Figure 2) Moreover, three out of seven subjects (42.8%) with previous urge urinary incontinence stayed completely dry throughout this study.
Regarding urodynamic findings, the maximum bladder capacity increased from the median of 182.7 with ±25.7 s.d. at baseline to 335.5 with ±25.6 s.d. in the final urodynamic test, whereas in the filling phase, the mean maximum detrusor pressure decreased from 52.7 with ±14.9 s.d. cm H20 (range 35–75) to 27.2 with ±8.8 s.d. cm H20 (range 20–40) in the final examination. Using the Wilcoxon test P<0.05 compared with baseline was detected post-SNM for both the aforementioned urodynamic parameters. In the two patients with detrusor sphincter dyssynergia, no SNM effect was ever detected. In addition, the detrusor pressure at maximum flow rate, PdetQ(max), was similar post-SNM compared with baseline. In the final urodynamic investigation, PdetQ(max) was 40 and 54 cm H20 in the patient with detrusor sphincter dyssynergia of grade 1 and 2, respectively. Four revisions for battery depletion were needed in four patients. The mean life span of the replaced IPGs in these patients was 66 months (range 57–83).
Complications
Overall, a total of 1457 months of SNM experience with 22 adverse events occurred in 19 patients.
Table 4 reports the number and type of complications for both groups.
All complications prompted unscheduled visits. The main difference between the two groups concerns the loss of efficacy occurring only in the urinary retention category. An early side effect for patients submitted to the original single surgical procedure was the development of a wound infection where the IPG was placed, and a late complication resulting in loss of efficacy was the need for a new implant in the controlateral sacral S3 root. There were no irreversible or severe adverse events, and all were resolved.
Conclusions
Our study contains the largest series of implanted SCI patients ever published. In patients with incomplete SCI, SNM is very effective in the treatment of both overactive and retentive NLUTS. Hence, an SNM evaluation should be considered for incomplete SCI patients with overactive bladder syndrome in case of anticholinergic failure, as well as for SCI subjects with non-obstructive urinary retention.11, 12 However, in our sample, the percentage occurrence of late failures in urinary retention subjects because of loss of efficacy (30.7%) is to be taken into account, even though all patients developing device failure responded to controlateral sacral S3 lead placement. In addition, SNM is safe; in fact, the percentage of adverse events was low overall, and all were treated effectively with only five cases necessitating surgical intervention. The reason why subjects submitted to SNM permanent implantation may lose their clinical benefits during follow-up is still unknown. Literature offers a possible explanation related to the neuroplasticity of the micturition center.13 The exact mechanism by which neuromodulation using SNM works is still not completely known.14 In addition, new studies with a larger number of SCI subjects would confirm the clinical efficacy of SNM for NLUTS, and/or the possible correlation between clinical improvement and urodynamic investigations. Though this is exclusively a clinical study, for some urodynamic parameters a significant improvement as a result of SNM has been shown in all groups. Obviously, objective data, such as urodynamics correlated to clinical effects, would provide more confidence in the therapy's efficacy. Further research should focus on the recruitment of a larger number of SCI subjects with incomplete lesions, as one unusual aspect is the often-concomitant presence of bladder, bowel and sexual dysfunction because of the same neurological etiology.15 With SNM, these individuals would achieve remarkable clinical improvement in more than one of these functions. Thus, when we decide that SCI patients are good candidates for this therapy, we plan to give them a treatment the positive clinical effects of which can relate to more than one pelvic organ.16 To evaluate the possible benefits of SNM, a multidisciplinary medical team is needed for assessing the bladder, bowel and sexual function before and after SNM visits. Literature reports that the cost-effective analysis of SNM has shown to be an efficient measure with an incremental cost-effective ratio regarding bowel or lower urinary tract dysfunction, compared with earlier LUTS therapies such as catheters and anticholinergic drugs.17 In fact, it was recently shown that the managing of SCI bladder and bowel dysfunction through a neuroprosthesis implant of the anterior sacral nerves with posterior rhizotomy greatly reduces the cost of pharmacological therapies.18 Even the possibility for individuals with incomplete SCI lesions to have significant concomitant clinical positive benefits for LUTS, bowel function and sexuality with SNM could massively reduce the cost of therapy, compared with earlier chronic pharmacological treatments or time-consuming procedures such as intravesical electrostimulation or Stoller afferent neurostimulation, positively affecting the individual's psychological and social life as well.
At this time, there are few experimental studies of SNM stimulus parameters and/or neurophysiological monitoring. A successful trial stimulation remains the best indicator for patient selection, and should be used as a routine diagnostic test for NLUTS that cannot be adequately resolved by medications or behavioral interventions. The most promising research field for the future is treating neurogenic pelvic floor dysfunctions by electrical modulation, trying to find new sites and parameters of stimulation through the guidance of neurophysiological tests. However, the technique of detrusor electromyography, described recently in humans as a clinically useful investigation for evaluating the sacral parasympathetic system, which is crucial for lower urinary tract functioning, is still lacking.19 Neurophysiological monitoring could be important, not only in order to predict SCI subjects responding to SNM but also to try to obtain more information regarding its mechanism of action, evaluating, for example, whether clinical modifications are correlated to neurophysiological evidence, and in this way being able to choose the most suitable stimulation.20 It would then be possible to have a more selective or events-driven stimulator for voiding, bowel and sexual function, allowing either a more improved and durable response or appropriate patient selection, which at the moment remains quite empiric. However, our results stimulate research in this field to improve knowledge and further the use of SNM for the treatment of neurogenic patients.
References
Samson G, Cardenas DD . Neurogenic bladder in spinal cord injury. Phys Med Rehabil Clin N Am 2007; 18: 255–274.
Tanagho EA, Schmidt RA . Bladder pacemaker: scientific basis and clinical future. Urology 1982; 20: 614–619.
Kessler TM, Burkhard FC, Madersbacher H, Kofler A, Poewe W, Kiss G . Safety of prolonged sacral neuromodulation tined lead testing. Curr Med Res Opin 2008; 24: 343–347.
Lombardi G, Mondaini N, Macchiarella A, Cilotti A, Del Popolo G . Clinical female sexual outcome after sacral neuromodulation implant for lower urinary tract symptom (LUTS). J Sex Med 2008; 5: 1411–1417.
Hoenfellner M, Humke J, Hampel C, Dahms S, Matzel K, Roth S et al. Chronic sacral neuromodulation for treatment of neurogenic bladder dysfunction: long term results with unilateral implants. Urology 2001; 58: 887–892.
Wallace PA, Lane FL, Noblett KL . Sacral nerve neuromodulation in patients with underlying neurologic disease. Am J Obstet Gynecol 2007; 197: 96.e101–105.
Braun PM, Böhler G . Results of sacral nerve modulation for treatment of overactive bladder. Urologe A 2006; 45: 835–840.
Scheepens WA, Weil EH, van Koeveringe GA, Rohrmann D, Hedlund HE, Schurch B et al. Buttock placement of the implantable pulse generator: a new implantation technique for sacral neuromodulation–a multicenter study. Eur Urol 2001; 40: 434–438.
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U et al. Standardisation of terminology: lower urinary tract function. Neurourol Urodyn 2002; 21: 167–178.
American Spinal Injury Association. International Standards for Neurological and Functional Classification of Spinal Cord Injury Revised 1996. American Spinal Injury Association: Chicago, 1996.
Datta SN, Chaliha C, Singh A, Gonzales G, Mishra VC, Kavia RB et al. Sacral neurostimulation for urinary retention: 10-year experience from one UK centre. BJU Int 2008; 101: 192–196.
Sutherland SE, Lavers A, Lavers A, Carlson A, Holtz C, Kesha J et al. Sacral nerve stimulation for voiding dysfunction: one institution'′s 11-year experience. Neurourol Urodyn 2007; 26: 19–28.
van Voskuilen AC, Oerlemans DJ, Weil EH, de Bie RA, van Kerrebroeck PE . Long term results of neuromodulation by sacral nerve stimulation for lower urinary tract symptoms: a retrospective single center study. Eur Urol 2006; 49: 366–372.
van der Pal F, Heesakkers JP, Bemelmans BL . Current opinion on the working mechanisms of neuromodulation in the treatment of lower urinary tract dysfunction. Curr Opin Urol 2006; 16: 261–267.
Benevento BT, Sipski ML . Neurogenic baldder, neurogenic bowel and sexual dysfunction in people with spinal cord injury. Phys Ther 2002; 82: 601–612.
Jarrett ME, Matzel KE, Christiansen J, Baeten CG, Rosen H, Bittorf B et al. Sacral nerve stimulation for faecal incontinence in patients with previous partial spinal injury including prolapse. Br J Surg 2005; 92: 734–739.
Aboseif SR, Kim DH, Rieder JM, Rhee EY, Menefee SA, Kaswick JR et al. Sacral neuromodulation: cost considerations and clinical benefits. Urology 2007; 70: 1069–1073.
Creasey GH, Dahlberg JE . Economic consequences of an implanted neuroprosthesis for bladder and bowel management. Arch Phys Med Rehabil 2001; 82: 1520–1525.
Podnar S . Neurophysiology of the neurogenic lower urinary tract disorders. Clin Neurophysiol 2007; 118: 1423–1437.
Zeller FL, Lassalle G . Importance of the neurophysiological evoked potential register during the implantation of a sacral neuromodulator. Arch Esp Urol 2007; 60: 51–54.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lombardi, G., Del Popolo, G. Clinical outcome of sacral neuromodulation in incomplete spinal cord injured patients suffering from neurogenic lower urinary tract symptoms. Spinal Cord 47, 486–491 (2009). https://doi.org/10.1038/sc.2008.172
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.172
Keywords
This article is cited by
-
Neuromodulation Following Spinal Cord Injury for Restoration of Bladder and Erectile Function
Current Bladder Dysfunction Reports (2023)
-
Systematic Literature Review and Meta-Analysis of Sacral Neuromodulation (SNM) in Patients with Neurogenic Lower Urinary Tract Dysfunction (nLUTD): Over 20 Years’ Experience and Future Directions
Advances in Therapy (2021)
-
Surgical management of the neurogenic bladder after spinal cord injury
World Journal of Urology (2018)
-
Role of sacral neuromodulation in modern urogynaecology practice: a review of recent literature
International Urogynecology Journal (2018)
-
Sakrale Nervenstimulation bei Stuhlinkontinenz
coloproctology (2017)