Abstract
Study design:
Retrospective study of 13 patients treated by the authors.
Objective:
To examine the course of the disease of malignant lymphoma (ML) presenting in the epidural area of the spine.
Setting:
Department of Neurosurgery, Third Department of Internal Medicine, Medical and Health Science Center, University of Debrecen, Debrecen, Hungary.
Subjects and methods:
The epidural presentation in eight patients was heralded by motor signs (paraparesis and plegia), in one by a lesion of the posterior columns of the spinal cord (ataxia), and in three by pain. One patient was free of complaints and symptoms. The affected epidural area was diagnosed previously by myelography and computerized tomography (CT), and later by magnetic resonance (MR), over the course of which the location was verified as thoracic in eight patients, cervical in one, and lumbar in four. The authors recommended surgical intervention in 9 out of 13 cases, in seven cases of Hodgkin's and six cases of non-Hodgkin's lymphoma. Seven patients were treated for recognized manifestations of malignant lymphoma while six were diagnosed by intraoperative-histological examination.
Results and conclusion:
The decompression operations for tumors resulted in limited improvement in seven patients (reduction in pain and return of ability to walk). Four patients were not operated on, two of which had significant improvement in their neurological symptoms. Paraparesis remained unchanged in one patient. One patient remained symptom-free. The authors emphasize the importance of interdisciplinary consultation and weighing individual priorities in the indications for operation on epidural ML.
Similar content being viewed by others
Introduction
Extranodal and spinal, epidural presentation of malignant lymphoma (ML) is rare. Non-Hodgkin's lymphoma (NHL) is about three times as common as Hodgkin's lymphoma (HL).1, 2, 3, 4, 5 The presentation of ML can be divided into two groups: (1) the primary extranodal, and (2) the advanced, disseminated forms of the disease. Advanced stage is more commonly encountered with epidural presentation and the primary extranodal form is more common in NHL. The rate of epidural occurrence in all case of MLs is rare (0.8–2.8%).3, 4, 5, 6, 7, 8, 9, 10 Due to this rate of occurrence small case number studies and case reports dominate the literature. Surgical intervention is recommended for epidural ML when myelocompression is found.2, 11 The analysis of our current retrospective study of the treatment of epidural ML found data comparable to that in the international literature.
Materials and methods
The third department of Internal Medicine and the department of Neurosurgery at Debrecen University Medical and Health Sciences Center conducted a retrospective study of data collected from patients treated for ML. Based on clinicopathological, diagnostic and therapeutic findings, epidural involvement was retrospectively analyzed in 512 patients treated for HL and 654 patients for NHL (Table 1). We represented the patients' sex, age, area of epidural involvement, the elapsed time between the discovery and the epidural manifestation of ML, survival time and treatment. The precise location of the tumor was determined by myelography, computerized tomography (CT) and magnetic resonance (MR). During the course of the operation, laminectomy and tumor reduction were carried out at the level of the tumor. We examined the neurological status of the patient, and response to treatment. Chemotherapy (KT) and radiotherapy (RT) were carried out in accordance with international recommendations adopted locally. Operation was contraindicated in the case of spinal cord compression by tumor only in advanced disease and poor general condition of the patient.
Results
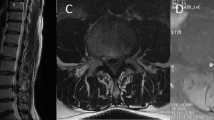
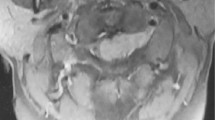
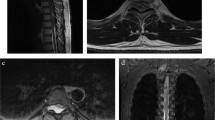
Of the 13 ML patients, 11 were men and two were women. The detailed data are shown on Table 1. The average age at the time of discovery of the epidural tumor was 39.07 years (range 16–66). We found HL in seven patients and NHL in six. The first symptom in 12 patients according to case history was pain, which with progression resulted in a radicular pattern, and long-path symptoms with or without sphincter dysfunction. In one patient a CT examination carried out for pulmonary lymphoma revealed involvement of the spinal cord without local symptoms. Involvement of the thoracic-8 vertebral body can be seen in Figure 1 and NHL invading the epidural space is apparent.
We did not perform operations on four patients. In one, a MR performed because of local pain revealed an early-stage epidural space occupation (without spinal cord compression), which regressed with KT. In the other three, the poor condition of the patient prevented operation. Patient number 2 was treated with KT and RT with the result of tumor regression. However, clinical improvement did not occur due to the advanced stage of illness. Three months after the recognition of epidural manifestations, the patient died from the further propagation of the disease. In patients 3 and 4, we did not perform expedient surgery due to the poor condition of patients. Combination therapy in the latter resulted in regression and improvement in neurological function, but the survival times were only 12 and 27 months, respectively.
We performed operations on nine patients, two for local and radicular pain, and seven for long path symptoms. Although laminectomy and tumor reduction resulted in complete spinal cord and cauda equina decompression in all patients, the paraparesis caused by myelopathy in patients 5 and 6 did not improve. The clinical condition of the other seven patients improved and they became ambulatory. The survival time after spinal presentation of ML for the members of this study was variable. Seven patients died between 3 and 120 months. Median survival time was 52.57 months. According to the last control, of our patients, six are still alive and in complete remission (3–185 months).
Discussion
Extranodal presentation can be found in 25–30% of patients with ML,12 although epidural presentation is relatively rare with a frequency of 0.8–2.8%.5, 13, 14 The extranodal form of ML can be found at any age, however it is most common in the 50s and 60s.15 The clinical picture is similar to metastatic carcinoma although the method of spread of the tumor is different. Malignant lymphoma spreads from the lymph node through the intervertebral foramina or may reach the epidural space from the vertebral body.5, 6, 8, 16, 17, 18 In contrast to carcinoma with epidural metastasis, in spinal presentation of ML months may pass before the development of the first local pain or spinal cord compression and consequent paraparesis.5 In one of our patients with an affected thoracic vertebra, the disease was discovered before any symptoms developed and remission was achieved with RT and KT. Malignant lymphoma is most commonly present in the mid-thoracic and lower lumbar segments.3, 17 Presentation in the cervical segments is rare because cancer appearing in the paracervical areas is usually discovered early.2 Similar to data found in the literature, among our patients there were one cervical, eight thoracic and four lumbar lymphoma cases.
Magnetic resonance is now indispensable in the diagnosis of the malignant diseases of the spine. CT has a role in some cases, primarily in evaluation of the effects on the vertebrae.17 A typical MR appearance of ML demonstrates a homogeneous, medium signal intensity, space occupying process spread beyond a single vertebral body with paravertebral extension. Computerized tomography imaging demonstrates osteolytic and osteoblastic alterations quite well. The unilateral involvement of a small joint on traditional X-ray, which may be the consequence of an osteolytic process, may also be the first visible sign. Current routine imaging technology cannot unambiguously differentiate ML from other cancers. In the future, time-consuming MR-spectrography may present a step forward.
Optimal treatment requires a multidisciplinary approach. The intraspinal extranodal form carries a poor prognosis, but no worse than the other extranodal-ML diseases. The fundamental goal of treatment is the best extension of the patient's life with the best quality. In as much as ML responds well to KT and RT, these modalities may form the basis of treatment of patients with the spinal form of ML. Most of the space occupying processes moving to the intraspinal space do not allow for delay. Spinal cord compression found in the neck and back can result in sensitive and relatively rapid irreversible alterations, which may cause cross-sectional lesions. In most of our patients, serious paraparesis was the first sign indicating a spinal tumor requiring urgent surgical decompression. In the lumbar area, the cauda equina is less sensitive to pressure and in this region local and radicular symptoms send the patient to the doctor. These symptoms do not present an absolute indication for urgent surgical intervention. The situation is different for primary epidural ML. In those patients the histological analysis of the surgical biopsy gives the diagnosis. According to Perry et al.2 the improvement in neurological symptoms is due to the decompression surgery. Patchell et al.11 likewise consider that surgery is important in spinal cord decompression. Bearing these in mind, three of our patients for whom surgery was contraindicated due to a poor cardiopulmonological condition, experienced significant improvement without surgery.
Of the KT and RT treated cases, three of the four experienced improvement in neurological symptoms, which was no worse a proportion than the operative cases (10 out of 13). In cases of spinal cord compression, rapid surgical decompression is nevertheless an advantage. Interdisciplinary consultation with an oncologist, hematologist, neurosurgeon and radiologist is unconditionally recommended in the case of spinal ML.
References
Macalchi M, Torselli P, Falaschi F, Dal Pozzo G . MRI of spinal epidural lymphoma. Neuroradiology 1995; 37: 303–307.
Perry JR, Deodhare SS, Bilbao JM, Murray D, Muller P . The significance of spinal cord compression as the initial manifestation of lymphoma. Neurosurgery 1993; 32: 157–162.
Toprak A, Kodalli N, Alpdogan TB, Giral A, Celikel CA, Gurmen N et al. Stage IV Hodgkin's disease presenting with spinal epidural involvement and cauda equina compression as the initial manifestation: case report. Spinal Cord 1997; 35: 704–707.
Nokes SR, Heury GM, Bucolo A, Harshfield DL . Radiological case of the month. J Arkansan Med Soc 1990; 87: 293–294.
Higgins SA, Peschel RE . Hodgkin's disease with spinal cord compression. Cancer 1995; 75: 94–98.
Moridaira K, Handa H, Murakami H, Uchiyama T, Takeuchi T, Saro S et al. Primary Hodgkin's disease of the bone presenting with an extradural tumor. Acta Haematol 1994; 92: 148–149.
Bender BL, Mayernik DG . Hodgkin's disease presenting with isolated craniospinal involvement. Cancer 1986; 58: 1745–1749.
Burch PA, Grossman SA . Treatment of epidural cord compressions from Hodgkin's disease with chemotherapy. Am JMed 1988; 84: 555–558.
Grubbs SS, Tilton DC . Oncologic emergencies. Del Med J 1990; 62: 1339–1347.
Miyakoshi N, Shimada Y, Suzuki T, Hongo M, Itoi E . Magnetic resonance imaging of spinal involvement by hematopoietic malignancies requiring surgical decompression. J Orthop Sci 2003; 8: 207–212.
Patchell AR, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet 2005; 366: 643–648.
Ferreri AJ, Reni M . Prognostic factors in primary central nervous system lymphomas. Hematol Oncol Clin North Am 2005; 4: 629–649.
Plotkin SR . Update on primary central nervous system lymphoma. Curr Opin Neurol 2005; 6: 645–653.
Gavrilovic IT, Abrey LE . Diagnosis and treatment of primary central nervous system lymphoma. Curr Oncol Rep 2005; 1: 47–54.
Epelbaum R, Haim N, Ben-Shahar M, Ben-Arie Y, Feinsod M, Cohen Y . Non-Hodgkin's lymphoma presenting with spinal epidural involvement. Cancer 1986; 58: 2120–2124.
Recht LD . Neurologic Complications of systemic lymphoma. Neurol Clin 1991; 9: 1001–1015.
Zimmerman RA . Central nervous system lymphoma. Radiol Clin N Am 1990; 28: 697–721.
Carde P, Burgers JM, Henry-Amar M, Hayat M, Sizoo W, Van der Schueren E et al. Clinical stage I and II Hodgkin's disease: a specifically tailored therapy according to prognosis factors. J Clin Oncol 1988; 6: 239–252.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Székely, G., Miltényi, Z., Mezey, G. et al. Epidural malignant lymphomas of the spine: collected experiences with epidural malignant lymphomas of the spinal canal and their treatment. Spinal Cord 46, 278–281 (2008). https://doi.org/10.1038/sj.sc.3102124
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102124