Abstract
Study design: A case report of superior mesenteric artery syndrome (SMA syndrome) occurring in a paraplegic patient 3 months after injury.
Objectives: To report an unusual case and review the literature of SMA syndrome in spinal cord injured patients, focusing on paraplegic subjects and on tardive presentations.
Setting: A Physical Medicine and Rehabilitation Center in Garches (France).
Method: Current medical literature includes reports of only 14 spinal cord injured patients with SMA syndrome. This syndrome has been often described in anorexia nervosa, burns or other causes of cachexia, following correction of spinal deformities or after application of body casts.
Results: In spinal cord injured patients SMA usually occurs in tetraplegic patients during the first weeks after injury. Only four cases of SMA syndrome in paraplegic patients have been described. Late forms are less common than acute ones: only three cases among 14. SMA syndrome consists of a vascular compression of the third part of the duodenum between the ventrally oriented SMA and the aorta. The normal aorto-mesenteric angle ranges between 38° and 65° and can be as low as 6° in patients with SMA syndrome. The diagnosis is usually based on upper gastro-intestinal contrast X-ray study, which shows abrupt vertical compression of the third part of the duodenum. CT scan with angiography is useful in some difficult cases. Conservative management includes early correction of dehydration and electrolyte imbalance, insertion of a nasojejunal tube beyond the obstruction and renutrition. Duodenojejunostomy may be necessary in case of failure of conservative treatment.
Conclusion: SMA syndrome is an unusual gastro-intestinal complication that may occur in paraplegic patients, even late after injury.
Similar content being viewed by others
Introduction
Superior mesenteric artery syndrome (SMA syndrome) consists of compression of the third portion of the duodenum by the overlying superior mesenteric arteria. It was first described in 1842 by Rokitansky.1 This syndrome is also known as mesenteric root syndrome, cast syndrome, Wilkie's syndrome, chronic duodenal ileus and intermittent arterio-mesenteric occlusion.
SMA syndrome has been described in several situations: anorexia nervosa,2 rapid growth in length without simultaneous weight gain,3 following correction of spinal deformities,4,5 application of body casts,4 cerebral injury,6,7 burns or other causes of cachexia. It has also been described in spinal cord injured (SCI) patients,8,9,10,11,12,13,14,15 especially in tetraplegic subjects. It usually occurs during the initial stage of the injury but some delayed cases have been described.
We report a case of SMA syndrome in a paraplegic patient which occurred 3 months after spinal cord injury, during the rehabilitation programme.
Case Report
The 11th of June 2000, a 54-year-old man was involved in a bicycle accident in which he sustained D7–D8 vertebral fracture-luxation with ASIA A D6 paraplegia. Five days later, he underwent surgical treatment consisting in reduction of the luxation, laminectomy D7–D8 and posterior fusion procedure with Domino-II RRC instrumentation and postero-lateral bone graft. Body plaster cast for dorsal immobilisation was applied for 6 weeks and removed in July 2000. No medical complications occurred during the initial stage of the paraplegia: the patient was transferred to a Physical Medicine and Rehabilitation center 3 weeks after the accident. He began his rehabilitation programme and had no gastro-intestinal symptoms.
In August 2000 (3 months after injury), the patient began to experience nausea and vomiting, with abdominal pain. On clinical examination, he showed tympanic abdominal hypogastric distension. His weight loss since the accident was 12 kg.
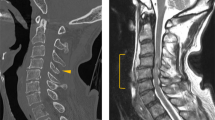
Symptomatic treatment with Metoclopramide did not improve the symptoms and the patient experienced a progressive further weight loss of 2 kg and vomiting became more frequent and abundant. He underwent plain abdominal radiographs which demonstrated a fluid level in a markedly distended stomach (Figure 1). Symptoms resolved with nasogastric tube placement and aspiration of stomach contents (2320 ml/day) but started again when the tube was removed.
Two days later, an upper gastro-intestinal contrast X-ray study was performed; it showed dilatation of the first and second portions of the duodenum and abrupt vertical compression of the third part (Figure 2); the cutoff of barium flow reversed when the patient was bending forward.
Treatment consisted of enteral and parenteral renutrition. A feeding tube was inserted beyond the obstruction, thus enabling progressive naso-jejunal feeding. A central catheter was also inserted in order to correct hydro-electrolytic imbalance and to begin renutrition. Two weeks later, the patient had regained 8 kg and experienced complete cessation of symptoms. The central catheter was then removed and total oral feeding was started. One month after the beginning of the symptoms, the patient had regained 12 kg.
The patient left hospital 5 months later, returned home and did not experience intestinal problems after discharge.
Discussion
The third portion of the duodenum is retroperitoneal and runs between the ventrally oriented SMA and the aorta. The normal aorto-mesenteric angle ranges from 38° to 65°,16,17 with a SMA-aorta distance of 13 to 34 mm where the third duodenum crosses the aorta.17
Under normal circumstances, retroperitoneal fat and lymphatic tissues serve as a cushion, holding the SMA off the spine and protecting the duodenum from compression by it.5 The theory of fat providing protection of the duodenum explains why weight loss is a major risk factor of SMA syndrome. Furthermore, hyperextension of the spine with increased lumbar lordosis, prolonged supine position, or visceroptosis due to flacid abdominal wall can favour SMA syndrome for anatomical reasons. Hypertrophy or a short suspensory ligament of Treitz can play a part by drawing the duodenum in the apex of the acute angle.
Clinical features of SMA syndrome are well documented. The diagnosis is suspected when symptoms of upper gastro-intestinal obstruction including nausea, vomiting, abdominal distension and abdominal pain are observed.6,9 Complications may be severe: delay in diagnosis may result in dehydration, metabolic imbalance or death. Respiratory distress syndrome18 and gastric perforations19 have been described. Early diagnosis is necessary to avoid complications.9
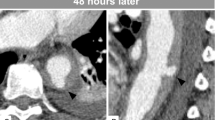
Confirmation of the diagnosis requires abdominal radiographs and upper gastro-intestinal tract study which reveals dilatation of the first and second part of the duodenum with an abrupt cutoff at the third part.17,20 Findings in these basic diagnostic techniques are evocative but not specific. Computed tomography with angiography provides aorta-SMA distance, duodenal distension and amount of intra-abdominal and retroperitoneal fat.17 Konen17 reported three cases of patients with SMA syndrome who underwent CT angiography: the mean measured aorta-SMA angle was 9° (range 8–10°) whereas the mean aorta-SMA distance was 8.1 mm (range 5.7–11 mm). Though not always necessary, CT angiography with 3D reconstruction may play a complementary diagnostic role when other techniques do not confirm the diagnosis.
The incidence of this syndrome in SCI population is not well known. Gore8 identified three patients among 567 SCI who developed SMA syndrome, which suggests an incidence of 0.53%. Medical literature reports about 14 cases of SMA syndrome in SCI patients (Table 1). Several factors may predispose SCI patients to this syndrome:14 spinal deformity, application of a body cast, rapid and severe weight loss, prolonged supine positioning, decreased abdominal tone.
In our patient, severe weight loss and prolonged supine position were the major precipitating factors of SMA syndrome. Surgical treatment of the spine in this case was necessary for reduction of the luxation to avoid post-traumatic kyphosis. It is unlikely that correction of spine deformity in this patient caused the SMA syndrome. SMA syndrome has been described after acute reduction of the spinal curvature in scoliosis or hyper-kyphotic deformities,5,21 when the spine was subjected to both high distraction forces and severe decreased thoracic kyphosis.
Current medical literature includes reports of traumatic quadriplegic patients with SMA syndrome.8,9,12,13,14 Only four cases of paraplegic patients developing SMA syndrome have been described. Ohry10,11 described two cases of paraplegic patients who developed SMA syndrome: the first was a non-operated patient and the second was a traumatic paraplegic patient who underwent spinal surgery during which Harrington instrumentation was used. This patient developed SMA syndrome 1 week after surgery. Loeb9 reported three cases of SMA syndrome concerning two tetraplegic and one paraplegic patient who developed this complication 3 weeks after the onset of the paraplegia. In 2000, Wilkinson15 described a paraplegic patient who experienced a SMA syndrome 1 month after his injury. The cause of SMA syndrome in this case study was multifactorial: quick weight loss, use of spinal instrumentation, and retrocaval haematoma. To our knowledge, no other report of paraplegic subjects developing SMA syndrome has been mentioned in medical literature.
The most common presentation in non spinal cord injured patients is one of chronic illness, frequently associated with longstanding ematiating diseases.3,22,23 Acute forms have been found in previously healthy patients who suffered weight loss through severe illness or after surgery.
Acute presentation such as the one described in our observation is more common in spinal cord injured (SCI) patients. Only one case of subacute SMA syndrome is reported in medical literature13 in a young tetraplegic woman, suggesting intermittent occlusion of the duodenum.
Unlike in the present case, SMA syndrome usually occurs during the first weeks following spinal cord injury. In traumatic brain injury, Philip7 reports five cases of children who sustained SMA syndrome in the rehabilitation setting. There have been very few reports of occurrence of this clinical entity in SCI patients who were undergoing a rehabilitation programme, or after home discharge. Roth14 studies the cases of three patients with SMA syndrome, one of whom developed this syndrome 6 months after the accident. Ramos12 describes the case of a tetraplegic patient who developed a SMA syndrome 3 months after injury. Raptou13 reports the case of a tetraplegic patient with several medical complications who developed the syndrome 4 months after SCI.
Differential diagnosis concerns other gastro-intestinal complications encountered in SCI patients. Acute complications include reflex ileus and gastric dilatation.8 Reflex ileus, usually accompanied by gastric dilatation, is due to autonomic nervous system imbalance: since parasympathetic innervation remains intact, sympathetic input is frequently lost, resulting in unchecked parasympathetic activity. Cases of gastric dilatation without generalised ileus have been described:8,12,24 whether these cases corresponded to SMA syndrome remains unclear. Both gastric and duodenal peristaltism reduction associated with mechanical obstruction may contribute to the upper gastro-intestinal obstruction, which can be called either ‘SMA syndrome’ or ‘acute gastric dilatation’. The occurrence of diminished peristaltism in upper gastro-intestinal tract and relative obstruction due to SMA syndrome related to severe weight loss or spinal deformity may explain why this syndrome can often be seen during the initial stage of high spinal cord injuries.
Conservative non-operative treatment classically includes small frequent meals,3 positioning the patient in a side-lying or knee-to-chest position after meals,12,13 removing spinal hyper-extension orthoses.5
When the case is acute, a nasogastric tube must be inserted for gastric aspiration. Early correction of dehydration and prevention of electrolyte imbalance are necessary. In severe forms, a tube must be inserted beyond the obstruction to enable continued nutritional support,9 while parenteral nutrition is started. When inserting a tube beyond the obstruction is not possible, and if weight loss is considered as a precipitating factor, total parenteral nutrition is an effective adjunct because it produces a rapid increase in weight.4,6,9
Surgery may be indicated when conservative treatment is not efficient: duodenojejunostomy seems to be the best procedure.9,23,25 Cleavage of the ligament of Treitz is another option, enabling the duodenum to drop away from the apex of the sharpened aorto-mesenteric angle. Laparoscopic management is possible in both interventions.26 In children, duodenal derotation has been suggested.7
References
Rokitansky C. . Handbuch der Pathologischen Anatomie Vienna, Brandmiller and Siedel 1842
Elbadawy MH . Chronic superior mesenteric artery syndrome in anorexia nervosa Br J Psychiatry 1992 160: 552–554
Van Brussel JP, Dijkema WP, Adhin SK, Jonkers GJPM . Wilkie's syndrome, a rare cause of vomiting and weight loss: diagnosis and therapy Netherlands Journal of Medicine 1997 51: 179–181
Munns SW, Morrissy RT, Steivers Golladay E, McKenzie CN . Hyperalimentation for superior mesenteric-artery syndrome following correction of spinal deformity JBJS 1984 66A: 1175–1177
Shapiro G, Green DW, Fatica NS, Boachie-Adjei O . Medical complications in scoliosis surgery Curr Opin Pediatr 2001 13: 36–41
Pedoto MJ, O'Dell MW, Thrun M, Hollifield D . Superior mesenteric artery syndrome in traumatic brain injury: two cases Arch Phys Med Rehabil 1995 76: 871–875
Philip PA . Superior mesenteric artery syndrome: an unusual case of intestinal obstruction in brain-injured children Brain Injury 1992 6: (4) 351–358
Gore RM, Mintzer RA, Calenoff L . Gastro-intestinal complications of spinal cord injury Spine 1981 6: 538–544
Loeb T, Loubert G, Morsly R, Gabillet JM, Pasteyer J . Syndrome de l'artère mésentérique supérieure Ann Fr Anesth Réanim 1999 18: 1000–1004
Ohry A, Zeilig G, Shemesh Y . Acute intermittent arteriomesenteric occlusion of the duodenum after use of Harrington's spinal instrumentation: case report Paraplegia 1988 26: 350–354
Ohry A, Perlmutter M . SMA syndrome in acute traumatic paraplegia Harefuah (Heb) 1985 108: 346–347
Ramos M . Recurrent superior mesenteric artery syndrome in a quadriplegic patient Arch Phys Med Rehabil 1975 56: 86–88
Raptou AD, Laban MM, Johnson EW . Intermittent arteriomesenteric occlusion of the duodenum in a quadriplegic patient Arch Phys Med Rehabil 1964 45: 418–423
Roth EJ, Fenton LL, Gaebler-Spira DJ, Frost FS, Yarkony GM . Superior mesenteric artery syndrome in acute traumatic quadriplegia: case reports and literature review Arch Phys Med Rehabil 1991 72: 417–420
Wilkinson R, Huang CT . Superior mesenteric artery syndrome in traumatic paraplegia: a case report and literature review Arch Phys Mred Rehabil 2000 81: 991–994
Derrick JR, Fadhli HA . Surgical anatomy of the superior mesenteric artery Am Surg 1965 31: 545–547
Konen E, Amitai M, Apter S, Garniek A, Gayer G, Nass S, Itzchak Y . CT Angiography of Superior mesenteric artery syndrome AJR 1998 171: 1279–1281
Banerjee A, O'Neil R, Bidstrup H . Adult respiratory distress syndrome caused by superior mesentery artery syndrome Anesth Intensive Care 1994 22: 602–604
Saul SH, Dekker A, Watson CG . Acute gastric dilatation with infarction and perforation. Report of fatal outcome in patient with anorexia nervosa Gut 1981 22: 978–983
Shetty AK, Schmidt-Sommerfeld, Haymon ML, Udall JN . Radiological case of the month: Superior mesenteric artery syndrome Arch Pediatr Adolesc Med 1999 153: 303–304
Sapkas G, O'Brien JP . Vascular compression of the duodenum (cast syndrome) associated with the treatment of spinal deformities Arch Orthop Traumat Surg 1981 98: 7–11
Gustafsson L, Falk A, Lukes PJ, Gamklou R . Diagnosis and treatment of superior mesenteric artery syndrome Br J Surg 1984 71: 499–501
Ylinen P, Kinnunen J, Höckerstedt K . Superior mesenteric artery syndrome: a follow-up study of 16 operated patients J Clin Gastroenterol 1989 11: 386–391
Todd SR, Marshall GT, Tyroch AH . Acute gastric dilatation revisited The Am Surg 2000 66: 709–710
Hines JR, Gore RM, Ballantine GH . Superior mesenteric artery syndrome Am J Surg 1984 148: 630–632
Massoud WZ . Laparoscopic management of superior mesenteric artery syndrome Int Surg 1995 80: 322–327
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Laffont, I., Bensmail, D., Rech, C. et al. Late superior mesenteric artery syndrome in paraplegia: case report and review. Spinal Cord 40, 88–91 (2002). https://doi.org/10.1038/sj.sc.3101255
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101255
Keywords
This article is cited by
-
Wilkie or Ogilvie?
Spinal Cord Series and Cases (2018)
-
Distal Duodenal Obstruction: a Surgical Enigma
Indian Journal of Surgery (2017)
-
Beyond broken spines–what the radiologist needs to know about late complications of spinal cord injury
Insights into Imaging (2015)
-
Superior Mesenteric Artery Syndrome: Where Do We Stand Today?
Journal of Gastrointestinal Surgery (2012)
-
Superior mesenteric artery syndrome in a tetraplegic patient, 11 years after a spinal cord injury: a case report
Spinal Cord (2010)