Abstract
Critical care medicine developed out of other subspecialties' need to provide care for their most critically ill patients. Advanced technologies, the understanding of the pathophysiology of critical illness, and the development of the multidisciplinary team have made this care possible. Pediatric critical care medicine emerged in the 1960s and has expanded dramatically since then. The field has made major advances in the areas of lung injury, sepsis, traumatic brain injury, and postoperative care. We review here the evolution of modern pediatric critical care medicine from its roots in general pediatric and cardiac surgery, adult respiratory care medicine, neonatology, and pediatric anesthesiology to its current state as a unique discipline.
Similar content being viewed by others
Main
Pediatric intensive care has only been recognized as a distinct subspecialty for 20 y. The specialty grew out of a need for increasingly complex postoperative management, in the face of advances in surgical and medical subspecialties, and the development of sophisticated life-support technology. The intensivist now directs a multidisciplinary team that includes other subspecialists, nurse specialists, respiratory therapists, nutritionists, pharmacists, social workers, clergy, physical therapists, occupational therapists, and others. The pediatric intensivist's role is to provide supportive care during cardiorespiratory and/or multi-organ failure or recovery from surgical interventions or trauma. Intensivists coordinate complex treatment plans with multiple participants to further the care of critically ill children.
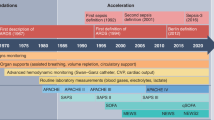
DEVELOPMENT OF THE PEDIATRIC INTENSIVE CARE UNIT
A number of factors led to the development of the subspecialty of pediatric critical care medicine. In 1992, John Downes identified five crucial fields of medicine in the 1950s that led to the emergence of pediatric critical care: adult respiratory intensive care, neonatology and neonatal intensive care, pediatric general surgery, pediatric cardiac surgery, and pediatric anesthesiology (1).
From the 1930s to 1950s, adult respiratory intensive care units were created to battle the scourge of the polio epidemic with “iron lung” ventilators. Out of necessity, these units also cared for children with polio (1). The neonatologists, in their newly created neonatal intensive care units, developed procedures for nutritional and environmental support of sick newborns and premature infants along with ventilation techniques and monitoring for treating hyaline membrane disease (also known as respiratory distress syndrome). The understanding and use of surfactant and continuous positive airway pressure mechanical ventilation greatly improved survival of infants with respiratory distress syndrome. By the 1960s, many infants with respiratory distress syndrome, who received extended mechanical ventilation, developed persistent lung disease, termed bronchopulmonary dysplasia (2). This created a need for extended care of older infants and children with the ensuing chronic lung disease (1).
During this period, advances in pediatric surgery necessitated that children receive complex postoperative monitoring and care not possible on a regular pediatric ward. In recognition of this need at the Children's Hospital of Philadelphia, C. Everett Koop (later the Surgeon General of the United States) developed the first discrete postsurgical care area for infants in 1956 with a dedicated nursing team. Its capacity and staffing increased in 1962 to become the first modern infant ICU in North America to primarily care for postsurgical neonates (1). Advances in other surgical subspecialties, notably in pediatric congenital heart surgery, led to a need to develop ICUs to provide complex postoperative care. The introduction of cardiopulmonary bypass for repair of congenital heart lesions accelerated this need (1).
In addition to these advances in ventilator management and surgery, the new field of pediatric anesthesiology came to the forefront. These anesthesiologists were the first to transfer principles of infant and pediatric physiology and pharmacology from the operating room to the ICU and the first to care for critically ill infants and children outside the operating room (1). Before the creation of fellowships in pediatric critical care, additional training in anesthesiology provided pediatricians with an entrée to the skills and expertise needed to care for critically ill and injured children. Many pediatric anesthesiologists assumed leadership roles by establishing or directing pediatric ICUs.
The first pediatric ICU was established in Europe by Goran Haglund in 1955 at Children's Hospital of Goteburg in Sweden, 10 y before the unit at Children's Hospital of the District of Columbia was developed by Cheston Berlin (1,3). John Downes opened the next recorded pediatric ICU at Children's Hospital of Philadelphia in 1967 (1). Over the next 40 y, hundreds of pediatric ICUs would be established in academic institutions, children's hospitals, and many community hospitals throughout North America and Europe. Randolph et al. (4) identified 306 general pediatric ICUs in the United States in 1995 and 349 in 2001.
DEVELOPMENT OF THE SUBSPECIALTY
The subspecialty of pediatric critical care soon followed the establishment of pediatric ICUs. The Society of Critical Care Medicine (SCCM), representing the adult intensive care community, recognized pediatric critical care as discrete, and created the section of pediatric critical care within the SCCM in 1981 (1). In 1983, guidelines defining the minimal requirements for pediatric ICUs were introduced by the Committee on Hospital Care and the Pediatric Section of the SCCM (5,6).
The American Academy of Pediatrics also created a section on critical care medicine in 1984. A sub-board in critical care medicine was established by the American Board of Pediatrics and the first certifying examination was offered in 1987 (1). Fellowship training programs began in the 1970s and early 1980s. The Hospital for Sick Children in Toronto, Children's Hospital of Philadelphia, National Children's Medical Center in Washington, DC, Children's Hospital of Boston, Children's Hospital of Dallas, Children's Hospital of Michigan, Children's Hospital of Pittsburgh, and The Johns Hopkins Hospital developed the first training programs in North America.
By 1990, there were 26 programs accredited by the Accreditation Council on Graduate Medical Education (ACGME) (1). Currently, there are 59 approved 3-y programs training 295 fellows (up from 249 fellows in 1997). In 1995, 68 of 2685 (2.5%) of first-time takers of the general pediatrics certifying exam had chosen to subspecialize in critical care (7). In 2004, there were 1134 diplomates in pediatric critical care medicine, making up 7.5% of all pediatric subspecialty diplomates.
Pediatric intensivists have had a significant impact on the survival of critically ill children. Pollack et al. (8) showed that there was an improved survival during hospitalization in a pediatric ICU with an intensivist [relative odds of dying, 0.65; 95% confidence interval (CI), 0.44–0.95; p = 0.027]. The risk of dying in a pediatric ICU with a critical care fellowship program versus a pediatric ICU without a critical care fellowship program also decreased (relative risk of dying, 0.714; 95% CI, 0.529–0.964, p = 0.028) (9).
BOOKS AND JOURNALS
Mark Rogers is credited with introducing the first comprehensive pediatric critical care textbook in 1987, Textbook of Pediatric Intensive Care (10). In 1995, David Nichols published the first pediatric cardiac critical care textbook, Critical Heart Disease in Infants and Children (11). In July of 2000, the specialty's first and only journal, Pediatric Critical Care Medicine, was established.
DATABASES AND COLLABORATIVE GROUPS
The first collaborative research group for pediatric critical care, the Pediatric Critical Care Study Group, was founded in the early 1990s by Gregory Stidham at LeBonheur Children's Medical Center. It was comprised of approximately 60 pediatric ICUs, mostly from the United States. It generated a number of studies related to pediatric ICU outcomes and length of stay, ribavirin use in infants, ECMO, and respiratory failure (12–17).
The next pediatric critical care collaborative research group, Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network, was founded by Adrienne Randolph at Children's Hospital of Boston in the late 1990s and included the participation of 48 pediatric ICUs throughout North America to study therapies for acute lung injury, sepsis, multi-organ failure, and other acute, life-threatening pulmonary or systemic inflammatory syndromes. It generated a number of studies related to mechanical ventilation weaning protocols, severity of illness and organ dysfunction scoring in children, and prone positioning and surfactant administration for acute lung injury (18–21).
In 2000, the first Internet database, The Virtual PICU, was founded by Randall Wetzel at Children's Hospital Los Angeles to create an international forum for pediatric intensivists to establish a shared patient database for outcomes analysis and improve critical care practices.
In 2004, The Collaborative Pediatric Critical Care Research Network was established by Carol Nicholson, the program director of Pediatric Critical Care and Rehabilitation Research at the National Institutes of Health. Six academic U.S. pediatric intensive care units were awarded funds to investigate the safety and efficacy of treatment and management strategies of critically ill children and investigate the pathophysiological bases of critical illness and injury in childhood.
MAJOR ADVANCES
The major advances in pediatric critical care can be categorized into those that impact care of specific disease processes, those that impact postoperative care of children, new technologies, and improvements in pediatric sedation and pain management. Acute respiratory distress syndrome (ARDS), septic shock, and traumatic brain injury are challenging disease processes that have received considerable attention because each is associated with high morbidity and mortality.
Acute respiratory distress syndrome.
ARDS is the most severe form of acute lung injury (ALI) in pediatric and adult patients. First described primarily in adults by Ashbaugh et al. (22) in 1967, patients with ARDS have profound respiratory failure and bilateral infiltrates on chest radiograph. ARDS originally stood for “adult respiratory distress syndrome” at the time, because it was thought to occur predominantly in adults and this moniker separated it from the respiratory distress syndrome seen in neonates, particularly premature infants, with surfactant deficiency. ARDS has since been renamed “acute respiratory distress syndrome” following an American-European consensus conference in 1994 (23).
ARDS may accompany sepsis, massive transfusions, multiple trauma, pneumonia (viral, bacterial, or fungal), burns, drownings, and inhalation injuries (24–28). All of these conditions include an acute, inflammatory process that causes diffuse alveolar-capillary damage with decreased pulmonary compliance and hypoxemia (24,25). The initial injury results from neutrophil migration and proinflammatory cytokine release, which then produces disruption of endothelial cells and noncardiogenic pulmonary edema (25). This is followed by an exudative alveolitis and degradation of surfactant that promotes atelectasis, further hypoxemia, and reduced lung compliance (25). Within several weeks, proliferation of type-2 epithelial cells, alveolar septal thickening, intra-alveolar granulation tissue formation, and collagen deposition heralds a fibrinoproliferative phase (25). Martin et al. (29) showed that ARDS patients with pulmonary fibrosis had a higher mortality rate than ARDS patients without pulmonary fibrosis (57% versus 0%; p < 0.02).
Petty and Ashbaugh (30) redefined ARDS in 1971 to include such symptoms as severe dyspnea and tachypnea, cyanosis refractory to oxygen therapy, with decreased pulmonary compliance, and diffuse alveolar infiltrates on chest radiograph. In 1988, Murray et al. (31) introduced a numerical lung injury score that categorized patients into three groups: no lung injury, mild-to-moderate lung injury (ALI), or severe lung injury (ARDS). Components of the score include the amount of alveolar consolidation on chest radiograph, the degree hypoxemia quantified by the Pao2/Fio2 ratio, the level of positive end-expiratory pressure during mechanical ventilation, and the quantified respiratory compliance (mL/cm H2O) (31). In 1994, Bernard et al. (23) introduced the most current and widely accepted clinical definition of ARDS: an acute onset, bilateral infiltrates on chest radiograph, pulmonary-artery wedge pressure ≤ 18 mm Hg and the absence of clinical evidence of left atrial hypertension, and a Pao2/Fio2 ratio of ≤ 200.
ARDS is rare in pediatrics and accounts for 0.2–2.7% of pediatric ICU admissions (27,32–34). ARDS accompanies 12% of children admitted for sepsis, viral pneumonia, smoke inhalation, or drowning (27). Most pediatric patients with ARDS are diagnosed with sepsis and pneumonia as well (34,35). Mortality from ARDS is not insignificant, ranging from 30% to 83% (32,34–40).
Numerous ventilation strategies have been explored to improve the outcome in ARDS, such as volutrauma, air leaks, and the development of chronic lung disease. The one proven strategy is low lung volume mechanical ventilation. Over-distention and cyclic inflation of injured lung with mechanical ventilation exacerbates lung injury and promotes systemic inflammation as well (41,42). These effects are minimized by utilizing low tidal volumes, which generate relatively lower inspiratory pressures, and applying positive end-expiratory pressure, to prevent alveolar collapse (42,43). The systemic release of inflammatory mediators from the lungs may explain why some ARDS patients develop multi-organ failure (44).
In 2000, the National Institutes of Health–sponsored Acute Respiratory Distress Syndrome Network low tidal volume study set the current standard for low tidal volume ventilation (6 mL/kg/breath) in ARDS because of its overall reduction in mortality in adult patients with ARDS compared with previously accepted larger volumes of 12 mL/kg/breath (31.0% versus 39.8%, p = 0.007) (45). Despite the lack of similar studies in children, the recommendation of using low tidal volumes for ventilation in ARDS (6 mL/kg/breath) has been applied to pediatric ICU patients. Other treatments, including pulmonary vasodilators (i.e. nitric oxide and prostacyclin), artificial surfactants, antiinflammatory agents, antioxidants, and antibiotics do not improve the outcome of ARDS (46).
Septic shock.
Sepsis and septic shock account for 3% of pediatric critical care transports and 6.3% of pediatric ICU admissions (47,48). In 1995, the cost for care of infants <1 y of age with severe sepsis was $1.1 billion dollars and for septic children, 1–19 y of age, the cost was $622 million (49).
Sepsis and septic shock have been defined and redefined, as our understanding of infection and the body's response to infection has changed. They have been defined in the 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference as a generalized systemic inflammatory response to infectious or noninfectious conditions, termed systemic inflammatory response syndrome (SIRS) (50). Laboratory markers such as IL-6, C-reactive protein, and procalcitonin may play an increasingly important role in defining and recognizing SIRS. Sepsis has been defined as SIRS resulting from infection. Severe sepsis has been defined as sepsis with the addition of organ dysfunction (50). Finally, septic shock has been defined as severe sepsis with acute circulatory collapse with signs of decreased end-organ perfusion (50,51).
The mortality of pediatric sepsis and septic shock has decreased over the last 50 y. Between 1958 and 1966, the mortality of children <16 y of age with Gram-negative bacteremia at the University of Minnesota Medical Center was 60% and 41% among medical and surgical categories, respectively (52). For those children who progressed to shock, the mortality rate was 98% (52). Since that time, the mortality of children with sepsis has been dramatically reduced. Stoll et al. (53) reported a 25% decline in mortality from bacterial sepsis for neonates <28 d and a 21% decline for infants 28 d to 1 y of age between 1979 and 1994. During that time period, the mortality from neonatal sepsis dropped from 51 to 38 per 100,000 live births and mortality from infant sepsis dropped from 72 to 56 per 100,000 live births (53). Other studies have documented a mortality rate of 10–29% in children with severe sepsis and septic shock (47–49,54).
Treatment—activated protein C, steroids, and goal-directed therapy.
Improved outcomes for children with sepsis and septic shock may be attributed to a better understanding of the pathophysiology of sepsis and aggressive therapeutic intervention. If left unchecked, proinflammatory and procoagulation processes progress to shock, disseminated intravascular coagulation, and multi-organ system dysfunction. Accordingly, attempts to inhibit inflammation or coagulation have been made (55). There has been limited success or, at times, even harm resulting from some of these efforts, which have included treatments targeting bacterial endotoxins, early host inflammatory cytokines, bioactive lipid mediators, nitric oxide, and replacement coagulation factors. Only activated protein C, an inhibitor of coagulation with antiinflammatory properties, and hydrocortisone, a suppressor of inflammation, have found their way into clinical therapeutics (55).
In 2001, a large, randomized, double-blinded, placebo-controlled, phase III trial of activated protein C reduced the absolute 28-d mortality by 6% in adults with sepsis and septic shock (56). There was an increase in serious bleeding in patients treated with activated protein C compared with placebo (3.5% for activated protein C versus 2.0% in controls; p = 0.06) (56). A pediatric efficacy and safety study performed by the manufacturer was discontinued due to the lack of improvement over placebo and an increased risk for intracranial hemorrhage (57). Thus, while recommended in critically ill adults, activated protein C is not recommended in children because of the bleeding risk and the absence of definitive pediatric trials (58).
Hydrocortisone also reduced the mortality of vasopressor-dependent adult septic shock patients who were nonresponders to a corticotropin stimulation test. Annane et al. (59), in 2002, found that hydrocortisone reduced mortality from 63% to 53% (p = 0.02). Pizarro et al. (60) observed absolute or relative adrenal insufficiency in 44% of children with catecholamine-resistant shock. Studies are needed to examine the efficacy of hydrocortisone in pediatric septic shock.
Goal-directed therapy has arisen as a term to describe the aggressive support of physiologic homeostasis in critical care therapy. In the 1980s, Shoemaker et al. (61) found that treatment algorithms for resuscitated trauma patients improved mortality. In 2001, a hallmark study by Rivers et al. (62) showed that early goal-directed therapy improved the outcome of adults with sepsis, lowering mortality from 47% (standard therapy) to 31% (p = 0.009).
Although no similar pediatric studies of goal-directed therapy and sepsis are present, early administration of fluids improves survival of children with septic shock (47,63). Furthermore, Ceneviva et al. (54) noted that maintaining a cardiac index of >3.3 L/min/m2 and a systemic vascular resistance of > 800 dyne-sec/cm5/m2 by administering inotropes or vasodilators improved survival when compared with the historical controls. As a result of these studies, clinical practice parameters for hemodynamic support of pediatric and neonatal patients in septic shock have been established (64).
Traumatic brain injury.
Each year, an estimated 1.5 million Americans sustain a TBI (65). The major causes of TBI-related deaths are firearms, motor vehicles, and falls (66). As a result, 50,000 people die, 80,000–90,000 have long-term disability, and 230,000 are hospitalized (65,66). Among children ages 0–19 y old, motor vehicle accidents are the major cause for TBI deaths (66).
The incidence of pediatric TBI (including emergency room visits, hospitalizations, and deaths), in 1998, was 670 per 100,000 children ages 0–19 y (67). In children younger than 2 y of age, physical abuse is a leading cause of serious head injury (68). Keenan et al. (68) reported an incidence of 17.0 per 100,000 person-years for inflicted traumatic brain injury in the first 2 y of life. Perez-Arjona et al. (69) noted that inflicted head trauma represented 32% of all trauma under age 2. For all age groups in the United States, there has been a relative decline in the mortality rate; 22% in the period from 1979 to 1992 and 11% in the period from 1989 to 1998 (66). Nevertheless, the rate of a “good” outcome, i.e. survival without serious neurologic sequelae, may not have changed for severe brain injury (70). Whereas the mortality may have improved, moderate or severe TBI still carries a high morbidity with significant neurologic impairment (71).
In some TBI, the initial insult may cause irreversible brain damage but secondary events may continue to expand the damage. These secondary events are potentially reversible and are what the pediatric intensivist aims to minimize. Maintaining an adequate cerebral perfusion pressure while minimizing exuberant cerebral blood flow, decreasing cellular metabolism and nutrient demands, and reducing cellular swelling are the goals of treatment (72–74).
Evidence-based guidelines for the acute management of severe traumatic brain injury in infants, children, and adolescents were published in 2003 (75). Because there was a paucity of controlled trials in the pediatric population, most recommendations were derived from adult studies. Nonetheless, these guidelines have become the standard management for the child with TBI.
Postoperative care of congenital heart disease patients.
In 1953, John Gibbon, at Jefferson Medical College Hospital in Philadelphia, performed the first open heart surgery, utilizing the total cardiopulmonary bypass machine that he designed (76). Before that, infants and children with congenital heart disease were treated with closed heart surgery or were deemed inoperable. Robert Gross at Children's Hospital in Boston performed the first ligation of a patent ductus arteriosus in a 7-y-old girl in 1938 and repaired an aortic coarctation in1944 (77,78). Craafort and Nylin (79) of Sweden performed a repair of an aortic coarctation is 1944 as well.
In 1945, Alfred Blalock and his African-American laboratory technician, Vivien Thomas (who pioneered the procedure in animals and assisted Blalock in the operating room), performed an extracardiac shunt between the subclavian artery and the ipsilateral pulmonary artery (Blalock-Taussig shunt) in a 15-mo-old girl with tetralogy of Fallot at Johns Hopkins Hospital (80–82).
These procedures, and the introduction of cardiopulmonary bypass, revolutionized treatment of congenital heart disease and stimulated the development of pediatric cardiac intensive care units, and improved perioperative care. A team, consisting of cardiac surgeons, pediatric cardiologists, pediatric intensivists, cardiac intensive care nurses, respiratory therapists, pharmacologists, nutritionists, and others, was needed for the care of these patients. The pediatric intensivist must understand normal and abnormal cardiopulmonary physiology, must appreciate the anesthetic and surgical techniques used, must provide advanced airway and vascular access, must apply appropriate monitoring, and must supervise hour-to-hour life support (83). In recognition of the complexities of cardiac intensive care, some intensivists have received and are proponents of further training in the care of the pediatric cardiac intensive care unit patient, in addition to the usual 3-y critical care fellowship (84,85).
Perioperative transplantation management.
The development of bone marrow transplantation in 1968 and solid organ transplantation in the 1960s has added new conditions to be managed by the intensivist, in both the pre- and posttransplantation period (86–93). The pediatric intensivist may care for children with refractory leukemia or immunodeficiency, fulminant hepatic failure with coagulopathy and encephalopathy, congestive heart failure from myocarditis, cardiomyopathy, or failing corrected/palliated congenital heart disease, or respiratory failure from end-stage lung disease before the actual transplant, and will be intimately involved in ensuring that these children remain stable while awaiting transplantation surgery. After transplantation, the intensivist must be aware of possible transplant complications including graft rejection, graft versus host disease, bleeding, or infection, and will be closely involved in managing these conditions. The pediatric ICU and pediatric intensivists have played a crucial part in the evolution of transplant medicine and in the ongoing improved survival rates of children who undergo transplantation.
TECHNOLOGIC ADVANCEMENTS
Mechanical ventilation.
Some children require ventilatory assistance as part of their postoperative care; others require ventilatory assistance due to an underlying disease. The pediatric intensivist employs both noninvasive and invasive methods of mechanical ventilation to ensure adequate oxygenation and ventilation.
Noninvasive mechanical ventilation (NMV) was first introduced in the late 1980s for patients with nocturnal hypoventilation (94,95). NMV utilizes a mask that is placed over the nose and/or mouth or prongs that are inserted into the nares to provide positive pressure ventilatory assistance. Either bilevel positive airway pressure (BiPAP) that generates differing inspiratory and expiratory positive airway pressures, or continuous positive airway pressure (CPAP) may be used.
NMV is used to augment impaired respiratory effort in a variety of diseases including asthma, cystic fibrosis, neuromuscular disorders, and congestive heart failure. Some advantages of NMV include ease of oral feeding, earlier ambulation, and diminishing the risk of nosocomial pneumonia or other complications associated with endotracheal intubation (96). Use of NMV often avoids the sedation needed for invasive mechanical ventilation (96).
There is proof that NMV prevents intubation for adults, but not for children (97). However, Fortenberry et al. (98) and Padman et al. (99) showed a low incidence of intubation (11% and 8%, respectively) and improvement in oxygenation, ventilation, and dyspnea in children with hypoxemic respiratory failure treated with NMV. Pediatric intensivists often use NMV to transition children from invasive mechanical ventilation to nonassisted ventilation.
Another noninvasive, respiratory-assist device that has recently become increasingly popular is high-flow, humidified gas delivered most commonly via a nasal cannula. One unit, the Vapotherm 2000i (Vapotherm, Annapolis, Maryland), delivers up to 40 L/min of gas flow with >95% humidity (<6 L/min is tolerated via conventional nasal cannula) (100). The high humidity prevents nasal mucosal drying and increases comfort at the higher gas flows. The high-flow system theoretically generates CPAP. Although the high-flow nasal cannula has been used in premature infants to prevent apnea of prematurity, generating similar distending pressures as nasal CPAP, no studies are available in older infants, children, or adolescents (101). However, the device has become popular because of its comfort and anecdotal success due to subjective improvement of respiratory distress and possible prevention of intubation of infants, children, and adolescents with respiratory difficulties.
Many severely ill children require endotracheal intubation and mechanical ventilation for postoperative care or cardiorespiratory failure. Lawen and Sievers provided the first description of mechanical ventilation in 1910. Their ventilator provided positive and negative pressure via a piston cylinder. The next mechanical ventilators were “iron lungs,” electrically powered, negative-pressure body tanks that were used extensively from the 1920s through the 1950s for polio patients (1).
Modern mechanical ventilators use computers to provide different modes of ventilation (pressure versus volume), synchronize with the patient ventilatory effort, and adjust inspiratory flow patterns to improve distribution of gas flow.
HFOV, first described by Lunkenheimer (102) in 1972, has gained popularity for treating children refractory to conventional ventilation. HFOV delivers a tidal volume less than the dead space volume at a rate >150 breaths per minute and a higher mean airway pressure (96). HFOV maintains an open lung yet avoids large phasic volume and pressure changes, thus minimizing the cyclical stretch of the lungs and ventilator-induced lung injury (96,103).
Most studies of HFOV in ARDS have been conducted in children. Fedora et al. (39) found that early use of HFOV (within the first 24 h of mechanical ventilation) reduced the mortality by 46% compared with is use after 24 h of conventional mechanical ventilation. Paulson et al. (104) noted that the use of HFOV improved oxygenation and survival (89%) compared with the published studies of ARDS, without increasing the risk of pneumothorax or other air leaks (27,36,105). However, HFOV did not improve mortality in premature infants with a variety of diseases leading to acute pulmonary dysfunction (106).
Artificial organs.
There are various technologies used to support failing organs, and the more common ones now in use include continuous veno-venous hemofiltration (CVVH) with or without dialysis for renal failure, ventricular assist devices (VADs) for heart failure, and extracorporeal membrane life support (ECLS), also known as extracorporeal membrane oxygenation (ECMO), for medically unmanageable heart and respiratory failure. The goal of these therapies is to aid recovery or to buy time for the patient to ultimately undergo surgery or organ transplantation (so called “bridge to transplant”).
In renal failure, the generalized edema that may occur sometimes impairs ventilation and compromises cardiac output. Developed in the mid-1960s, CVVH was first used to remove excess fluid or treat renal insufficiency (107). Currently, CVVH is most often used when acute renal failure accompanies bone marrow transplantation or treatment of malignancy, or as a complication of congenital heart disease, heart or liver transplantation, severe sepsis, or intrinsic renal disease (108).
CVVH also facilitates nutritional support and blood product administration without fluid overload (108). Goldstein et al. (109) showed that the degree of fluid overload at CVVH (with dialysis) initiation was significantly lower in survivors (16.4% ± 13.8%) compared with nonsurvivors (34.0% ± 21.0%, p = 0.03), even when controlled for severity of illness.
VADs are used in patients with cardiomyopathy who are in acute cardiogenic shock or severe heart failure, as a bridge to heart transplantation or recovery (110,111). VADs are surgically attached to the failing ventricle with an extracorporeal or implantable pneumatic or electric pump that generates improved blood flow. The VAD allows for improved mobility and quality of life in children and adults that have failed medical management for their heart failure.
Although cardiopulmonary bypass was introduced in 1953, the use of this technology was not used outside the operating room until 1972, when Hill et al. used ECLS to support the victim of a motorcycle accident. Robert Bartlett was instrumental in introducing and studying ECLS in infants and children. In 1976, Bartlett et al. (112) reported the first use of ECLS in infants with postoperative cardiac failure, infant respiratory distress syndrome, massive meconium aspiration, and persistent fetal circulation.
In 1989, Bartlett founded the Extracorporeal Life Support Organization (ELSO), which now contains a registry of over 24,000 cases of ECLS in infants, children, and adults from over 145 centers around the world.
ECLS supports a patient in circumstances where the cardiac and/or respiratory disease is medically unmanageable by conventional means and ensures adequate tissue oxygen delivery to support end-organ function. The ECLS team includes a surgeon, pediatric intensivist, nurse specialist, respiratory therapist, and perfusionist. ECLS requires surgical placement of cannulae into a major vein and artery, for veno-arterial ECLS, or solely a major vein, for veno-venous ECLS. It substitutes the patient's impaired respiratory and cardiovascular system by circulating blood via a special hollow-fiber polymethylpentene oxygenator that both oxygenates and removes carbon dioxide as the patient's blood circulates through the circuit. In older infants and children, ECLS has been used for support during severe sepsis, ARDS, cardiac failure due to myocarditis/cardiomyopathy, hemodynamic instability after congenital heart surgery repairs/palliations, and, in some cases, as a bridge to heart transplantation (113).
In a randomized trial of neonatal extracorporeal membrane oxygenation by the UK Collaborative ECMO Trail Group, full-term neonates with respiratory failure due to a number of causes were randomized to receive or not receive ECLS. Its use reduced the absolute mortality by 26% (RR of 0.55; 95% CI = 0.39–0.77; p = 0.0005) (114). In the United Kingdom, survival for neonatal and pediatric cardiac ECLS is approximately 50% (113).
The survival rate for ECLS used for patients requiring cardiopulmonary resuscitation in adults is 32–36%, 61% in neonates without congenital heart disease, and 64% in children with cardiac arrest after open-heart surgery (115–118). Pediatric intensivists, working in centers with ECLS capabilities, must understand the unique physiology that ECLS creates, the problem associated with its use, its advantages, its costs, and its limitations.
Monitoring.
Monitoring of critically ill patients is crucial to the success of critical care medicine. Many invasive and noninvasive devices have been developed to continuously monitor vital signs, end-tidal carbon dioxide, intracranial pressure, and arterial oxygen saturation to facilitate rapid response to changes in critically ill patients. End-tidal carbon dioxide (ETCO2) monitors and pulse oximetry are the two most important noninvasive monitoring devices in use today.
Smallhout and Kalenda introduced continuous measurements of ETCO2 measurements in intubated patients during the 1970s (119). Because ETCO2 is affected by ventilation, metabolism, and circulation, ETCO2 measurements from an endotracheal tube can identify inadequate mechanical ventilation, poor pulmonary blood flow (i.e. due to pulmonary embolism or pulmonary hypertension), poor cardiac function, and the presence of lung disease (i.e. asthma) (119). Measurements of ETCO2 in mechanically ventilated, intubated patients has become the standard of care in the pediatric ICU, and is increasingly relied upon as a means of recognizing displacement of the endotracheal tube, thus contributing to patient safety.
George Stokes first recognized that oxygen in the blood was carried by its colored component in 1864, but it was not until 1935 that Karl Matthes developed the first system to measure oxygen saturation in vivo by transillumination (120). In 1974, Takuo Aoyagi produced the first pilot model of a pulse oximeter, based on pulse spectrophotometry, the precursor of the modern pulse oximeter (121). Shortly thereafter, noninvasive pulse oximetry became commercially available. Pulse oximetry became increasingly more available and accepted for use in the 1980s and it is now used routinely in many areas of medicine (120). Pulse oximetry has improved patient safety in the operating room and in the intensive care unit, and is standard of care for all patients who undergo surgery or are admitted to ICUs.
Miniaturized equipment.
Pediatric patients range in size, from less than 1 to more than 100 kg, creating the need for an assortment of catheter sizes, endotracheal tubes, bronchoscopes, and other devices. Without the development of size-appropriate equipment, modern pediatric critical care would not be possible.
Before the 1950s, endotracheal tubes were made of reusable metal and rubber. Plastic polyvinyl chloride endotracheal tubes, introduced in the 1950s, soften at body temperature, are less rigid, and are less likely to cause subglottic stenosis (122). When smaller sizes of both cuffed and uncuffed endotracheal tubes were introduced, prolonged intubation of infants and children was made possible.
Similarly, intravenous access is crucial for the administration of fluids and medications to critically ill patients. Plastic catheters replaced rigid, metal needles in the mid-1940s and made long-term intravenous access possible (123). In 1958, George Doherty developed the present-day intravenous, flexible, catheter-around-the-needle device (123).
In the 1960s to 1970s, percutaneous central venous access was introduced. The introduction of pediatric-sized equipment enabled the placement of catheters for parenteral nutrition, monitoring of central venous pressures, and placement of pulmonary artery catheters to measure hemodynamic variables that include the cardiac output, vascular resistance, and pulmonary artery pressure.
TELEMEDICINE
The use of computer networks for video conferencing and computer-based data transmission now allows underserved areas or hospitals to benefit from the expertise of ICU specialists (124). In 2004, Marcin et al. (125) showed that a regional pediatric ICU-based telemedicine program providing live interactive consultations to a rural adult ICU was feasible and highly successful.
Rendina et al. (126) found that immediate echocardiogram interpretation via telemedicine significantly reduced the rate of transfer of neonates to academic medical centers. Kofos et al. (127) used telemedicine to assist with severity assessment and triage for transport. We anticipate that telemedicine will, by assisting in diagnosis, data interpretation, and treatment advice, reduce the rate of unnecessary transfers to sophisticated pediatric ICUs.
SEDATION AND PAIN MANAGEMENT
Sedation and analgesia are important components of optimal pediatric ICU care. Sedation and analgesia are often required when patients undergo intubation, mechanical ventilation, central venous catheter placement, chest tube placement, other invasive procedures, and to allow children to tolerate the often frightening ICU environment. Inadequate sedation or analgesia may also increase oxygen consumption and carbon dioxide production, and may produce a catabolic state that impairs recovery from critical illness or injury (128).
In 1993, Marx et al. (129) found that one-third of children in the ICU were inadequately sedated. There still is room for improvement with respect to the assessment and management of pain and anxiety in the pediatric ICU. In recognition of this problem, the California state legislature passed a law in October 2001 requiring all physicians in the state to participate in 12 h of education on pain management and treatment of the terminally ill by December 31, 2006.
Pediatric intensivists are increasingly aware of the need to use multiple modalities to improve the experience of the pediatric patient in the ICU. Numerous anesthetic, anxiolytic. and analgesic agents are used in the pediatric ICU, often by means of continuous infusions or via patient-controlled analgesia devices. Regional techniques including continuous epidural analgesia provide relief to pediatric patients after surgery or traumatic injuries. Parents are given unlimited access to their children in most pediatric ICUs and are often encouraged to participate in their care, and to remain present during painful or frightening procedures. In addition, nonpharmacologic strategies are being used in pediatric ICUs, including guided imagery, biofeedback, acupuncture, and relaxation techniques. Child life specialists engage with the patients to provide them with toys, mobiles, videos, and games that allow children to be distracted and engaged while in the ICU.
OTHER CHALLENGES
Pediatric critical care is a challenging and demanding subspecialty. Intensivists often work long hours, around the clock, to stabilize and manage seriously compromised children, to coordinate their care and to communicate with their families. The loss of patients is inevitable, and not all children will leave the ICU free of sequelae. These stresses, and others, contribute to “burnout” and dissatisfaction within the field, and each intensivist must develop coping strategies and definitions of work that will allow him or her to continue to practice in the face of these difficulties. Some intensivists offset their clinical responsibilities with academic pursuits, including laboratory or clinical research, teaching, and administrative duties. Those with a background in anesthesiology may provide anesthesia care when not working in the ICU. Others have become involved with efforts that define minimum standards for pediatric ICUs or the essential components of critical care fellowship training. Pediatric intensivists are involved in public policy work and with groups that address the challenges of funding critical care and the ethics of the care being provided. Still others divide their time between work as hospitalists and work as intensivists. Each intensivist must search for the balance needed to prevent “burnout.”
The cost of providing critical care to children is enormous and consideration of the ethics of distributing scarce or costly ICU resources is paramount. Many intensivists question providing care to children with limited chances of survival or meaningful recovery. Intensivists frequently encounter ethical dilemmas and may enlist the help of the hospital ethics committee, particularly with respect to futility and end of life issues. It is essential that all children have access to optimal critical care services, but it is also important that these services are used wisely and appropriately. Pediatric intensivists must be at the center of any debates about utilization of medical resources, health care funding, and access to care involving children in the years ahead.
SUMMARY
The pediatric ICU and the specialty of pediatric critical care medicine were created out of a necessity to care for the increasing number of children with critical illnesses and injuries. Advanced technologies, continuous monitoring, and specialized training in critical care have dramatically improved the care of infants and children with ARDS, septic shock, organ transplants, and many other diseases, and have contributed to improved outcomes and survivals for these and other disease processes.
Some critically ill children survive their initial admission but are left with sequelae or chronic problems that result in their return to the ICU with even more challenging problems. As advances have been made in other pediatric medical and surgical subspecialties, children are surviving extremely complex illnesses and surgical procedures, in part due to the careful ministration of pediatric intensivists. An intensivist must possess expertise in all but a few pediatric disciplines to coordinate and facilitate the care for the sickest children with a wide variety of problems. Thus, the pediatric intensivist has evolved into the generalist of the pediatric subspecialists.
Abbreviations
- ARDS:
-
acute respiratory distress syndrome
- CPAP:
-
continuous positive airway pressure
- CVVH:
-
continuous veno-venous hemofiltration
- ECLS:
-
extracorporeal membrane life support
- ECMO:
-
extracorporeal membrane oxygenation
- ETCO2:
-
end-tidal carbon dioxide
- HFOV:
-
high-frequency oscillatory ventilation
- ICU:
-
intensive care unit
- NMV:
-
noninvasive mechanical ventilation
- SIRS:
-
systemic inflammatory response syndrome
- TBI:
-
traumatic brain injury
- VAD:
-
ventricular assist device
References
Downes JJ 1992 The historical evolution, current status, and prospective development of pediatric critical care. Crit Care Clin 8: 1–22
Northway WH Jr, Rosan RC, Porter DY 1967 Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia. N Engl J Med 276: 357–368
Berlin CM 1970 The pediatric intensive care unit. Med Ann Dist Columbia 39: 483–486 passim
Randolph AG, Gonzales CA, Cortellini L, Yeh TS 2004 Growth of pediatric intensive care units in the United States from 1995 to 2001. J Pediatr 144: 792–798
1983 Guidelines for pediatric intensive care units. Pediatrics 72: 364–372
1983 Guidelines for pediatric intensive care units. Crit Care Med 11: 753–760
Oliver TK Jr, Tunnessen WW Jr, Butzin D, Guerin R, Stockman JA 3rd 1997 Pediatric work force: data from the American Board of Pediatrics. Pediatrics 99: 241–244
Pollack MM, Cuerdon TT, Patel KM, Ruttimann UE, Getson PR, Levetown M 1994 Impact of quality-of-care factors on pediatric intensive care unit mortality. JAMA 272: 941–946
Pollack MM, Patel KM, Ruttimann E 1997 Pediatric critical care training programs have a positive effect on pediatric intensive care mortality. Crit Care Med 25: 1637–1642
Rogers MC (ed) 1987 Textbook of Pediatric Intensive Care. Williams & Wilkins, Baltimore, pp 2 v( xvi, 1506)
Nichols DG, Greeley WJ, Lappe DG, Ungerleider RM, Wetzel RC 1995 Critical Heart Disease in Infants and Children. Mosby, St. Louis
Tilford JM, Simpson PM, Green JW, Lensing S, Fiser DH 2000 Volume-outcome relationships in pediatric intensive care units. Pediatrics 106: 289–294
Fiser DH, Tilford JM, Roberson PK 2000 Relationship of illness severity and length of stay to functional outcomes in the pediatric intensive care unit: a multi-institutional study. Crit Care Med 28: 1173–1179
Tilford JM, Roberson PK, Lensing S, Fiser DH 1998 Differences in pediatric ICU mortality risk over time. Crit Care Med 26: 1737–1743
Moler FW, Steinhart CM, Ohmit SE, Stidham GL 1996 Effectiveness of ribavirin in otherwise well infants with respiratory syncytial virus-associated respiratory failure. Pediatric Critical Study Group. J Pediatr 128: 422–428
Green TP, Timmons OD, Fackler JC, Moler FW, Thompson AE, Sweeney MF 1996 The impact of extracorporeal membrane oxygenation on survival in pediatric patients with acute respiratory failure. Pediatric Critical Care Study Group. Crit Care Med 24: 323–329
Timmons OD, Havens PL, Fackler JC 1995 Predicting death in pediatric patients with acute respiratory failure. Pediatric Critical Care Study Group. Extracorporeal Life Support Organization. Chest 108: 789–797
Randolph AG, Wypij D, Venkataraman ST, Hanson JH, Gedeit RG, Meert KL, Luckett PM, Forbes P, Lilley M, Thompson J, Cheifetz IM, Hibberd P, Wetzel R, Cox PN, Arnold JH, Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network 2002 Effect of mechanical ventilator weaning protocols on respiratory outcomes in infants and children: a randomized controlled trial. JAMA 288: 2561–2568
Lacroix J, Cotting J, for the Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network 2005 Severity of illness and organ dysfunction scoring in children. Pediatr Crit Care Med 6: S126–S134
Curley MA, Thompson JE, Arnold JH 2000 The effects of early and repeated prone positioning in pediatric patients with acute lung injury. Chest 118: 156–163
Willson DF, Thomas NJ, Markovitz BP, Bauman LA, DiCarlo JV, Pon S, Jacobs BR, Jefferson LS, Conaway MR, Egan EA, Pediatric Acute Lung Injury and Sepsis Investigators 2005 Effect of exogenous surfactant (calfactant) in pediatric acute lung injury: a randomized controlled trial. JAMA 293: 470–476
Ashbaugh DG, Bigelow DB, Petty TL, Levine BE 1967 Acute respiratory distress in adults. Lancet 2: 319–323
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R 1994 The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149: 818–824
Anderson MR 2003 Update on pediatric acute respiratory distress syndrome. Respir Care 48: 261–278
Redding GJ 2001 Current concepts in adult respiratory distress syndrome in children. Curr Opin Pediatr 13: 261–266
TenHoor T, Mannino DM, Moss M 2001 Risk factors for ARDS in the United States: analysis of the 1993 National Mortality Followback Study. Chest 119: 1179–1184
Davis SL, Furman DP, Costarino AT Jr 1993 Adult respiratory distress syndrome in children: associated disease, clinical course, and predictors of death. J Pediatr 123: 35–45
Milberg JA, Davis DR, Steinberg KP, Hudson LD 1995 Improved survival of patients with acute respiratory distress syndrome (ARDS): 1983–1993. JAMA 273: 306–309
Martin C, Papazian L, Payan MJ, Saux P, Gouin F 1995 Pulmonary fibrosis correlates with outcome in adult respiratory distress syndrome. A study in mechanically ventilated patients. Chest 107: 196–200
Petty TL, Ashbaugh DG 1971 The adult respiratory distress syndrome. Clinical features, factors influencing prognosis and principles of management. Chest 60: 233–239
Murray JF, Matthay MA, Luce JM, Flick MR 1988 An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis 138: 720–723
Walker TA 1999 The acute respiratory distress syndrome in children: recent UMMC experience. J Miss State Med Assoc 40: 371–375
Wang JD, Wang TM, Chi CS 2003 Clinical spectrum of acute respiratory distress syndrome in a tertiary pediatric intensive care unit. Acta Paediatr Taiwan 44: 202–207
Norrashidah AW, Azizi BH, Zulfiqar MA 1999 Acute respiratory distress syndrome in a paediatric intensive care unit. Med J Malaysia 54: 225–229
Paret G, Ziv T, Barzilai A, Ben-Abraham R, Vardi A, Manisterski Y, Barzilay Z 1998 Ventilation index and outcome in children with acute respiratory distress syndrome. Pediatr Pulmonol 26: 125–128
Timmons OD, Dean JM, Vernon DD 1991 Mortality rates and prognostic variables in children with adult respiratory distress syndrome. J Pediatr 119: 896–899
Chow JH, Jih KS, Shih CM, Chi CS 1993 Adult respiratory distress syndrome in children. Zhonghua Yi Xue Za Zhi (Taipei) 51: 111–115
Dahlem P, van Aalderen WM, Hamaker ME, Dijkgraaf MG, Bos AP 2003 Incidence and short-term outcome of acute lung injury in mechanically ventilated children. Eur Respir J 22: 980–985
Fedora M, Klimovic M, Seda M, Dominik P, Nekvasil R 2000 Effect of early intervention of high-frequency oscillatory ventilation on the outcome in pediatric acute respiratory distress syndrome. Bratisl Lek Listy 101: 8–13
Paret G, Ziv T, Augarten A, Barzilai A, Ben-Abraham R, Vardi A, Manisterski Y, Barzilay Z 1999 Acute respiratory distress syndrome in children: a 10 year experience. Isr Med Assoc J 1: 149–153
Gattinoni L, Vagginelli F, Chiumello D, Taccone P, Carlesso E 2003 Physiologic rationale for ventilator setting in acute lung injury/acute respiratory distress syndrome patients. Crit Care Med 31: S300–S304
Frank JA, Matthay MA 2003 Science review: mechanisms of ventilator-induced injury. Crit Care 7: 233–241
Frank JA, Gutierrez JA, Jones KD, Allen L, Dobbs L, Matthay MA 2002 Low tidal volume reduces epithelial and endothelial injury in acid-injured rat lungs. Am J Respir Crit Care Med 165: 242–249
Moloney ED, Griffiths MJ 2004 Protective ventilation of patients with acute respiratory distress syndrome. Br J Anaesth 92: 261–270
2000 Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 342: 1301–1308
Lumb AB, Nunn JF 2003 Nunn's Applied Respiratory Physiology. Butterworth-Heinemann, Oxford, UK
Han YY, Carcillo JA, Dragotta MA, Bills DM, Watson RS, Westerman ME, Orr RA 2003 Early reversal of pediatric-neonatal septic shock by community physicians is associated with improved outcome. Pediatrics 112: 793–799
Kutko MC, Calarco MP, Flaherty MB, Helmrich RF, Ushay HM, Pon S, Greenwald BM 2003 Mortality rates in pediatric septic shock with and without multiple organ system failure. Pediatr Crit Care Med 4: 333–337
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR 2001 Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 29: 1303–1310
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G 2003 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 31: 1250–1256
Carcillo JA 2003 Pediatric septic shock and multiple organ failure. Crit Care Clin 19: 413–440, viii
DuPont HL, Spink WW 1969 Infections due to Gram-negative organisms: an analysis of 860 patients with bacteremia at the University of Minnesota Medical Center, 1958–1966. Medicine (Baltimore) 48: 307–332
Stoll BJ, Holman RC, Schuchat A 1998 Decline in sepsis-associated neonatal and infant deaths in the United States, 1979 through 1994. Pediatrics 102: e18
Ceneviva G, Paschall JA, Maffei F, Carcillo JA 1998 Hemodynamic support in fluid-refractory pediatric septic shock. Pediatrics 102: e19
Marshall JC 2003 Such stuff as dreams are made on: mediator-directed therapy in sepsis. Nat Rev Drug Discov 2: 391–405
Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A, Steingrub JS, Garber GE, Helterbrand JD, Ely EW, Fisher CJ Jr, Recombinant human protein C Worldwide Evaluation in Severe Sepsis (PROWESS) study group 2001 Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med 344: 699–709
Eisenberg P 2005 Discontinuation of Study F1K-MC-EVBP, Investigation of the Efficacy and Safety of Drotrecogin Alpha (Activated) in Pediatric Severe Sepsis (Letter to FDA). Eli Lilly and Company, Indianapolis, Available at:http://www.fda.gov/medwatch/SAFETY/2005/Xigris. Accessed August 5, 2005
Giroir BP 2003 Recombinant human activated protein C for the treatment of severe sepsis: is there a role in pediatrics?. Curr Opin Pediatr 15: 92–96
Annane D, Sebille V, Charpentier C, Bollaert PE, Francois B, Korach JM, Capellier G, Cohen Y, Azoulay E, Troche G, Chaumet-Riffaut P, Bellissant E 2002 Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA 288: 862–871
Pizarro CF, Troster EJ, Damiani D, Carcillo JA 2005 Absolute and relative adrenal insufficiency in children with septic shock. Crit Care Med 33: 855–859
Shoemaker WC, Fleming AW 1986 Resuscitation of the trauma patient: restoration of hemodynamic functions using clinical algorithms. Ann Emerg Med 15: 1437–1444
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M, Early Goal-Directed Therapy Collaborative Group 2001 Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345: 1368–1377
Carcillo JA, Davis AL, Zaritsky A 1991 Role of early fluid resuscitation in pediatric septic shock. JAMA 266: 1242–1245
Carcillo JA, Fields AI, American College of Critical Care Medicine Task Force Committee Members 2002 Clinical practice parameters for hemodynamic support of pediatric and neonatal patients in septic shock. Crit Care Med 30: 1365–1378
Thurman DJ, Alverson C, Dunn KA, Guerrero J, Sniezek JE 1999 Traumatic brain injury in the United States: a public health perspective. J Head Trauma Rehabil 14: 602–615
Adekoya N, Thurman DJ, White DD, Webb KW 2002 Surveillance for traumatic brain injury deaths—United States, 1989–1998. MMWR Surveill Summ 51: 1–14
McCarthy ML, Serpi T, Kufera JA, Demeter LA, Paidas C 2002 Factors influencing admission among children with a traumatic brain injury. Acad Emerg Med 9: 684–693
Keenan HT, Runyan DK, Marshall SW, Nocera MA, Merten DF, Sinal SH 2003 A population-based study of inflicted traumatic brain injury in young children. JAMA 290: 621–626
Perez-Arjona E, Dujovny M, Vinas F, Park HK, Lizarraga S, Park T, Diaz FG 2002 CNS child abuse: epidemiology and prevention. Neurol Res 24: 29–40
Pfenninger J, Santi A 2002 Severe traumatic brain injury in children—are the results improving?. Swiss Med Wkly 132: 116–120
Dikmen SS, Machamer JE, Powell JM, Temkin NR 2003 Outcome 3 to 5 years after moderate to severe traumatic brain injury. Arch Phys Med Rehabil 84: 1449–1457
Hackbarth RM, Rzeszutko KM, Sturm G, Donders J, Kuldanek AS, Sanfilippo DJ 2002 Survival and functional outcome in pediatric traumatic brain injury: a retrospective review and analysis of predictive factors. Crit Care Med 30: 1630–1635
Vavilala MS, Bowen A, Lam AM, Uffman JC, Powell J, Winn HR, Rivara FP 2003 Blood pressure and outcome after severe pediatric traumatic brain injury. J Trauma 55: 1039–1044
Downard C, Hulka F, Mullins RJ, Piatt J, Chesnut R, Quint P, Mann NC 2000 Relationship of cerebral perfusion pressure and survival in pediatric brain-injured patients. J Trauma 49: 654–659
Adelson PD, Bratton SL, Carney NA, Chesnut RM, du Coudray HE, Goldstein B, Kochanek PM, Miller HC, Partington MD, Selden NR, Warden CR, Wright DW (eds); American Association for Surgery of Trauma; Child Neurology Society; International Society for Pediatric Neurosurgery; International Trauma Anesthesia and Critical Care Society; Society of Critical Care Medicine; World Federation of Pediatric Intensive and Critical Care Societies 2003 Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents. Pediatr Crit Care Med 4( 3 Suppl): S1–S75.
Gibbon JH Jr 1954 Application of a mechanical heart and lung apparatus to cardiac surgery. Minn Med 37: 171–180
Gross R, Hubbard JP 1939 surgical ligation of a patent ductus arteriosus: report of first successful case. JAMA 112: 729–731
Gross R, Hufnagel CA 1945 Coarctation of the aorta. Experimental studies regarding its surgical correction. N Engl J Med 233: 287–293
Craafort C, Nylin G 1945 Congenital coarctation of the aorta and its surgical treatment. J Thorac Surg 14: 347–361
Blalock A, Taussig HB 1945 The surgical treatment of malformations of the heart in which there is pulmonary stenosis or pulmonary atresia. JAMA 128: 189–202
Blalock A, Taussig HB 1984 Landmark article May 19, 1945: The surgical treatment of malformations of the heart in which there is pulmonary stenosis or pulmonary atresia. By Alfred Blalock and Helen B. Taussig. JAMA 251: 2123–2138
Brogan TV, Alfieris GM 2003 Has the time come to rename the Blalock-Taussig shunt?. Pediatr Crit Care Med 4: 450–453
Chang AC 2000 Pediatric cardiac intensive care: current state of the art and beyond the millennium. Curr Opin Pediatr 12: 238–246
Stromberg D 2004 Pediatric cardiac intensivists: are enough being trained?. Pediatr Crit Care Med 5: 391–392
Johnson FL 1981 Marrow transplantation in the treatment of acute childhood leukemia. Historical development and current approaches. Am J Pediatr Hematol Oncol 3: 389–395
McDiarmid SV 2003 Current status of liver transplantation in children. Pediatr Clin North Am 50: 1335–1374
Mittal NK, Tzakis AG, Kato T, Thompson JF 2003 Current status of small bowel transplantation in children: update 2003. Pediatr Clin North Am 50: 1419–1433, ix
Sweet SC 2003 Pediatric lung transplantation: update 2003. Pediatr Clin North Am 50: 1393–1417, ix
Benfield MR 2003 Current status of kidney transplant: update 2003. Pediatr Clin North Am 50: 1301–1334
Blume ED 2003 Current status of heart transplantation in children: update 2003. Pediatr Clin North Am 50: 1375–1391
Miniati DN, Robbins RC 2002 Heart transplantation: a thirty-year perspective. Annu Rev Med 53: 189–205
Benfield JR, Wain JC 2000 The history of lung transplantation. Chest Surg Clin N Am 10: 189–199, xi
Otte JB 2002 History of pediatric liver transplantation. Where are we coming from? Where do we stand?. Pediatr Transplant 6: 378–387
Ellis ER, Bye PT, Bruderer JW, Sullivan CE 1987 Treatment of respiratory failure during sleep in patients with neuromuscular disease. Positive-pressure ventilation through a nose mask. Am Rev Respir Dis 135: 148–152
Kerby GR, Mayer LS, Pingleton SK 1987 Nocturnal positive pressure ventilation via nasal mask. Am Rev Respir Dis 135: 738–740
Cheifetz IM 2003 Invasive and noninvasive pediatric mechanical ventilation. Respir Care 48: 442–458
Ferrer M, Esquinas A, Leon M, Gonzalez G, Alarcon A, Torres A 2003 Noninvasive ventilation in severe hypoxemic respiratory failure: a randomized clinical trial. Am J Respir Crit Care Med 168: 1438–1444
Fortenberry JD, Del Toro J, Jefferson LS, Evey L, Haase D 1995 Management of pediatric acute hypoxemic respiratory insufficiency with bilevel positive pressure (BiPAP) nasal mask ventilation. Chest 108: 1059–1064
Padman R, Lawless ST, Kettrick RG 1998 Noninvasive ventilation via bilevel positive airway pressure support in pediatric practice. Crit Care Med 26: 169–173
Waugh JB, Granger WM 2004 An evaluation of 2 new devices for nasal high-flow gas therapy. Respir Care 49: 902–906
Sreenan C, Lemke RP, Hudson-Mason A, Osiovich H 2001 High-flow nasal cannulae in the management of apnea of prematurity: a comparison with conventional nasal continuous positive airway pressure. Pediatrics 107: 1081–1083
Lunkenheimer PP, Rafflenbeul W, Keller H, Frank I, Dickhut HH, Fuhrmann C 1972 Application of transtracheal pressure oscillations as a modification of “diffusing respiration”. Br J Anaesth 44: 627
Bond DM, Froese AB 1993 Volume recruitment maneuvers are less deleterious than persistent low lung volumes in the atelectasis-prone rabbit lung during high-frequency oscillation. Crit Care Med 21: 402–412
Paulson TE, Spear RM, Silva PD, Peterson BM 1996 High-frequency pressure-control ventilation with high positive end-expiratory pressure in children with acute respiratory distress syndrome. J Pediatr 129: 566–573
DeBruin W, Notterman DA, Magid M, Godwin T, Johnston S 1992 Acute hypoxemic respiratory failure in infants and children: clinical and pathologic characteristics. Crit Care Med 20: 1223–1234
Henderson-Smart DJ, Bhuta T, Cools F, Offringa M 2003 Elective high frequency oscillatory ventilation versus conventional ventilation for acute pulmonary dysfunction in preterm infants. Cochrane Database Syst Rev CD000104
Burchardi H 1998 History and development of continuous renal replacement techniques. Kidney Int Suppl 66: S120–S124
Goldstein SL 2003 Overview of pediatric renal replacement therapy in acute renal failure. Artif Organs 27: 781–785
Goldstein SL, Currier H, Graf Cd, Cosio CC, Brewer ED, Sachdeva R 2001 Outcome in children receiving continuous venovenous hemofiltration. Pediatrics 107: 1309–1312
Matsuda H, Matsumiya G 2003 Current status of left ventricular assist devices: the role in bridge to heart transplantation and future perspectives. J Artif Organs 6: 157–161
Goldman AP, Cassidy J, de Leval M, Haynes S, Brown K, Whitmore P, Cohen G, Tsang V, Elliott M, Davison A, Hamilton L, Bolton D, Wray J, Hasan A, Radley-Smith R, Macrae D, Smith J 2003 The waiting game: bridging to paediatric heart transplantation. Lancet 362: 1967–1970
Bartlett RH, Gazzaniga AB, Jefferies MR, Huxtable RF, Haiduc NJ, Fong SW 1976 Extracorporeal membrane oxygenation (ECMO) cardiopulmonary support in infancy. Trans Am Soc Artif Intern Organs 22: 80–93
Walker G, Liddell M, Davis C 2003 Extracorporeal life support—state of the art. Paediatr Respir Rev 4: 147–152
1996 UK collaborative randomised trial of neonatal extracorporeal membrane oxygenation. UK Collaborative ECMO Trail Group. Lancet 348: 75–82
Chen YS, Chao A, Yu HY, Ko WJ, Wu IH, Chen RJ, Huang SC, Lin FY, Wang SS 2003 Analysis and results of prolonged resuscitation in cardiac arrest patients rescued by extracorporeal membrane oxygenation. J Am Coll Cardiol 41: 197–203
Younger JG, Schreiner RJ, Swaniker F, Hirschl RB, Chapman RA, Bartlett RH 1999 Extracorporeal resuscitation of cardiac arrest. Acad Emerg Med 6: 700–707
Doski JJ, Butler TJ, Louder DS, Dickey LA, Cheu HW 1997 Outcome of infants requiring cardiopulmonary resuscitation before extracorporeal membrane oxygenation. J Pediatr Surg 32: 1318–1321
del Nido PJ, Dalton HJ, Thompson AE, Siewers RD 1992 Extracorporeal membrane oxygenator rescue in children during cardiac arrest after cardiac surgery. Circulation 86: II300–II304
Bhende MS 2001 End-tidal carbon dioxide monitoring in pediatrics—clinical applications. J Postgrad Med 47: 215–218
Sinex JE 1999 Pulse oximetry: principles and limitations. Am J Emerg Med 17: 59–67
Aoyagi T 2003 Pulse oximetry: its invention, theory, and future. J Anesth 17: 259–266
Shann FA, Duncan AW, Brandstater B 2003 Prolonged per-laryngeal endotracheal intubation in children: 40 years on. Anaesth Intensive Care 31: 663–666
Zimmerman JJ, Strauss RH 1989 History and current application of intravenous therapy in children. Pediatr Emerg Care 5: 120–127
Wetzel RC 2001 The virtual pediatric intensive care unit. Practice in the new millennium. Pediatr Clin North Am 48: 795–814
Marcin JP, Nesbitt TS, Kallas HJ, Struve SN, Traugott CA, Dimand RJ 2004 Use of telemedicine to provide pediatric critical care inpatient consultations to underserved rural Northern California. J Pediatr 144: 375–380
Rendina MC, Carrasco N, Wood B, Cameron A, Bose C 2001 A logit model for the effect of telecardiology on acute newborn transfers. Int J Technol Assess Health Care 17: 244–249
Kofos D, Pitetti R, Orr R, Thompson A 1998 Telemedicine in pediatric transport: a feasibility study. Pediatrics 102: E58
Tobias JD, Rasmussen GE 1994 Pain management and sedation in the pediatric intensive care unit. Pediatr Clin North Am 41: 1269–1292
Marx CM, Rosenberg DI, Ambuel B, Hamlett KW, Blumer JL 1993 Pediatric intensive care sedation: survey of fellowship training programs. Pediatrics 91: 369–378
Acknowledgements
The authors thank the American Pediatric Society and its council for stimulating and supporting the activities of the work group on history, chaired by Drs. Lawrence Finberg and E. Richard Stiehm, which resulted in this manuscript. We also thank Dr. Gregory Stidham for providing information about the Pediatric Critical Care Study Group and the development of the pediatric ICU.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Epstein, D., Brill, J. A History of Pediatric Critical Care Medicine. Pediatr Res 58, 987–996 (2005). https://doi.org/10.1203/01.PDR.0000182822.16263.3D
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000182822.16263.3D
This article is cited by
-
Infant Intensive Care Unit: Is it Time to Change?
Indian Journal of Pediatrics (2024)
-
Utilizing big data from electronic health records in pediatric clinical care
Pediatric Research (2023)
-
The use of machine learning and artificial intelligence within pediatric critical care
Pediatric Research (2023)
-
Predicting long-term neurocognitive outcome after pediatric intensive care unit admission for bronchiolitis—preliminary exploration of the potential of machine learning
European Journal of Pediatrics (2023)
-
Mitigating Moral Distress: Pediatric Critical Care Nurses’ Recommendations
HEC Forum (2023)