Abstract
High intensity light-emitting diodes (LEDs) are being studied as possible light sources for the phototherapy of hyperbilirubinemic neonates. These power-efficient, low heat-producing light sources have the potential to deliver high intensity light of narrow wavelength band in the blue-green portion of the visible light spectrum, which overlaps the absorption spectrum of bilirubin (BR). We compared the efficacy between single LEDs of different color and then constructed a prototype phototherapy device using 300 blue LEDs. The efficacy of this device was compared with that of conventional phototherapy devices by measuring the in vitro photodegradation of BR in human serum albumin. When blue, blue-green, green, and white LEDs were compared, the blue light was the most effective in degrading BR by 28% of dark control, followed by blue-green (18% of control), and then white light (14% of control). Green light was the least effective (11% of control). The prototype device with three focused arrays, each with 100 blue LEDs, generated greater irradiance (>200 µW·cm-2·nm-1) than any of the conventional devices tested. It also supported the greatest rate of BR photodegradation. We conclude that light from LEDs should be considered a more effective treatment for hyperbilirubinemia than light from presently used phototherapy devices. Furthermore, the unique characteristics of this light source may make it especially suitable for use in safe and lightweight home phototherapy devices.
Similar content being viewed by others
Main
Phototherapy is the most frequently used treatment for the control of neonatal jaundice. Its efficacy is dependent upon irradiance (light intensity), the quality of the light (optimal in the blue-green, 400-550 nm), the exposed body surface area, and the duration of exposure. When initiated early, phototherapy can reduce serum BR levels to within clinically acceptable levels (<13 mg/dL or 222 µmol/L) (1). The most commonly used light sources are: fluorescent tubes (daylight, broad and narrow spectrum blue); halogen spotlights; and fiberoptic blankets (for contact use) (2). Each of these devices has a number of disadvantages that include high heat production and unstable (decreasing with age) broad wavelength light output. In severe cases of hyperbilirubinemia, the use of one device is often insufficient, and several different types are commonly used in combination to maximize light intensity and body exposure (1,3). However, in general it is likely that the administration of phototherapy is suboptimal (1).
Phototherapy is a relatively simple and safe method with few serious side effects. However, phototherapy has hazards that occasionally result in unexpected serious injury, especially in premature neonates (4,5). Also, phototherapy has been shown to cause a decrease in the endogenous levels of riboflavin, a natural photosensitizer (6).
We are studying a new type of light source, LEDs, for phototherapy, which have a narrow spectral band of high intensity monochromatic light (7,8) that overlaps the absorption spectrum of BR. Because of their small size, high light output, and low energy requirements, they have the potential to be used in overhead and pad-type devices for hospital-based, as well as for home, phototherapy.
Here we report on initial in vitro experiments that indicate that these small, power-efficient, durable, blue to green and white light sources may have several advantages over the presently used phototherapy devices. It was our objective to determine the efficacy between LEDs of various wavelength ranges (color) and conventional phototherapy units to degrade BR in vitro.
METHODS
The LEDs were purchased from Nichia Chemical Industries, Ltd. Some characteristics for each color type are given in Table 1.
For in vitro experiments comparing the BR photodegradation efficacy between different color LEDs, a single LED exposure device was constructed by mounting sets of five separate, 5-mm diameter LEDs of each color, which were connected in series on a circuit board (Fig. 1). Each set was powered by 24 VDC power supply through a 250-ohm load resistor.
Diagram of single-LED exposure device. Sets of five LEDs of each type were each mounted on the thin edge (1.5 mm) of a copper-clad circuit board (LED base), connected in series and powered by a 24-VDC power supply through a 200-ohm load resistor. An opaque black vial support block of Deldrin® with 12-mm diameter wells was placed over the LEDs so that the light source was located directly below the bottom of the vials. For in vitro tests, each vial was loaded with 25 µL of 20 mg of BR/dL, 4% HSA, and 75 µL of buffer. Light exposure was for 30 min at room temperature.
For the three-array prototype device, blue (3-mm diameter) LEDs, five each connected through a 220-ohm load resistor, were incorporated into nearly circular, densely packed arrays (5-cm diameter) of 100 each. Each array was cooled by a 4-cm diameter miniature fan. Three such arrays were interconnected through two hinges that allowed overlapping of the three projected light spots. The units were powered by a 24 VDC (2.4 A) power supply.
The Mini Bili-Lite® with a quartz halogen light source and the Bili-Lite® (BB) fluorescent tube unit with four each alternating, cool-white and special blue (F20T12) tubes were purchased from Olympic Medical, Seattle, WA. The BiliBlanket® (Ohmeda, Columbia, MD) is a flexible fiberoptic pad, powered by a quartz halogen bulb. The Photo-Spot® device (model no. FPS-1000) was obtained from Healthdyne Technologies, Marietta, CA, and operated at maximal irradiance.
Irradiance was measured with the Joey® Dosimeter (Fiberoptic Medical Products, Inc., Allentown, PA). This instrument, used clinically, measures the mean irradiance over a narrow wavelength range of 420-480 nm and reports light intensity as µW cm-2 nm-1. This instrument does not measure light intensity outside this wavelength interval.
Light intensity was also measured with the Extech Instruments Corp. (Waltham, MA) model 401025 light meter, which measures irradiance as lux and foot-candles in the broad wavelength range of 400-750 nm. BR (Sigma Chemical Co., Inc., St. Louis, MO) was dissolved in a minimal amount of 1 N NaOH, diluted with saline, and HSA (Sigma Chemical Co.) was added. The pH was adjusted to 7.4 with 1 N HCl, and the volume WAS adjusted to yield a solution of 20 mg BR/dL of 4% HSA in saline, pH 7.4. BR concentrations were measured at 460 nm with a UB Analyzer (UA-1, Arrows Co., Ltd, Tokyo, Japan). The BR absorption spectrum was determined with a Shimadzu (Columbia, MD) UV-160 model spectrophotometer.
The LED and cool white and special blue fluorescent emission spectra were determined on a model 1470 spectrophotometer (EG & G Corp., Princeton, NJ) with John J. Mahoney at LifeScan, Inc., Milpitas, CA. In vitro photodegradation of BR was determined essentially as previously described (9). Briefly, 25 µL of the BR solution and 75 µL of 100 mM potassium phosphate at pH 7.4 (buffer) were pipetted into the bottom of 2-mL clear glass vials (n = 5). The vials were sealed and exposed to each light source from below at 23°C using the single LED exposure device (Fig. 1) or through a glass-bottomed water bath at 37°C using the prototype and commercial phototherapy devices. After 30 min of light exposure, 925 µL of buffer were added, and the BR content was measured with a UB Analyzer.
BR degradation (%) was calculated as the difference between the pre- and postexposure BR concentrations divided by the preexposure BR concentration times 100. The data are presented as mean ± SD. Statistical analysis was performed by ANOVA using Fisher's protected least significant difference. Significant difference between treatments is indicated when p ≤ 0.05.
RESULTS
Figure 2 shows the measured narrow emission spectra of the blue, blue-green, and green LEDs. The white LED has a broader spectrum because it is essentially a blue LED with a yellow phosphor that causes the unit to emit white light. The spectra of the cool white and special blue fluorescent tubes are given for comparison to demonstrate their broader wavelength band light with localized mercury-emission peaks. Irradiance was measured with narrow and broad wavelength band detectors. The absorption spectrum of BR is also displayed.
Emission spectra of phototherapy light sources. The spectra of the blue (A), blue-green (B), green (C), and white (F) LEDs and the two fluorescent lamps [cool white (D) and special blue (E)] were measured under identical conditions with a model 1470 spectrophotometer. The intensity (vertical axis) is expressed in arbitrary units. The dashed vertical line represents the absorption peak (459 nm) of the BR solution used for the experiments. Panel G displays the absorption spectrum of the BR solution diluted with buffer to 2.5 mg of BR/dL.
The efficacy of each type of LED to photodegrade BR at room temperature was determined with the device shown in Fig. 1. The results (Fig. 3) show that the blue LED light was the most effective, followed by blue-green, and white light. Green light was the least effective. All LEDs, except between white and green, were significantly different in their ability to degrade BR (p < 0.05).
Efficacy comparison between LEDs. The single LED device (Fig. 1) was used to compare the efficacy of each LED type to degrade BR. Twenty-five microliters of 20 mg of BR/dL, 4% HSA, and 75 µL of buffer in the bottom of each vial (n = 5 per LED type per experiment) was exposed to each LED for 30 min at 23°C. After addition of 925 µL of buffer, the concentration of the remaining BR was determined with the UB Analyzer. A total of three experiments were performed. Irradiance was measured with the Joey® Dosimeter. Significant (p < 0.05) difference in BR degradation was determined by ANOVA and is indicated by a and b, where a denotes a significant difference from all other LEDs, and b denotes no significant difference from one another.
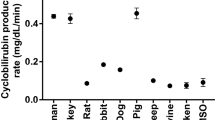
The in vitro efficacy of degrading BR with the prototype LED device with three focused arrays of 100 blue LEDs was compared with that of several conventionally used phototherapy devices (Fig. 4). Under the conditions given, the blue LED array had the greatest irradiance and was also the most effective light source for BR photodegradation. All light sources were significantly different in their ability to degrade BR (p < 0.05), except between the Mini Bili-Lite® and the BiliBlanket®.
Comparison of in vitro efficacy of light sources. BR degradation was measured (n = 4) through exposure of 25 µL of 20 mg of BR/dL and 75 µL of buffer in the vial bottoms to the indicated light sources for 15 min at 37°C. After addition of 925 µL of buffer, the concentration of the remaining BR was determined with the UB Analyzer. A significant (p < 0.05) difference in BR degradation was determined by ANOVA and is indicated by a and b, where a denotes a significant difference from all other light sources, and b denotes no significant difference from one another. All light sources were significantly different in their ability to degrade BR (p < 0.05), except between the Mini Bili-Lite® and the BiliBlanket®.
DISCUSSION
Visible LEDs have been available as light-generating devices since the 1960s, but their spectral quality and intensity were not suitable for use in phototherapy (10). Recently, Nakamura at the Nichia Chemical, Ltd. (Tokoshima, Japan) developed high intensity gallium nitride LEDs that emit light (7,8) in the blue-green wavelength range appropriate for the photochemical processes that determine the efficacy of phototherapy (11). In addition to the characteristics listed in Table 1, these solid-state light sources have several important advantages not found in the presently used devices such as: high and stable intensity (no light meter is needed); long life (>1 y of continuous use); narrow luminous spectrum; no infrared or UV radiation; no ozone generation; the ability to be focused with a lens or through spatial orientation; high energy efficiency (3.0 mW/LED); low voltage (5 VDC); use of direct current (no flickering/no vertigo); the ability to be battery-powered; no glass parts; small in size (3 or 5 mm diameter × 9 mm high for lamps or 3 × 2 × 1 mm for chips); light in weight (0.3 g); and shock and vibration proof. Diodes of different color can be combined into arrays of unlimited size, which can be adapted for contact use as pads and/or jackets or be used at any distance with or without focusing to deliver high intensity, narrow wavelength band light.
The rate of removal of unconjugated BR from the body by means of phototherapy depends on the rate of BR photoalteration, the transport of photoproducts from the skin to the circulation, and their excretion via the liver and kidney. It appears that photoalteration is the rate-limiting step in the process of BR elimination. Phototherapy in turn affects three different mechanisms of BR alteration (1,11). Photooxidation destroys BR to form colorless products. This reaction is thought to occur slowly, and its clinical significance is still being debated. Configurational isomerization occurs when native 4Z, 15Z BR absorbs a photon to form the more water-soluble E isomers (4Z, 15E; 4E, 15Z; and 4E, 15E) via reversible reactions. The serum of infants treated with phototherapy has been found to contain primarily the 4Z, 15E isomer. However, the 4Z, 15E isomer is excreted slowly, if at all. This process is wavelength-dependent with formation of the 4Z, 15E isomer at the shorter (blue) wavelengths and a reconversion of this isomer to the Z, Z form of native BR by the longer (green) wavelengths. Light intensity does not affect the reaction equilibrium, but it does affect the time it takes to reach the steady state. The third BR conversion reaction is that of structural isomerization, which irreversibly rearranges the atoms in BR to produce a new molecule with an even-membered ring. This compound, named lumirubin, can occur as four optically active isomeric forms. Lumirubin has a polarity between that of mono- and diglucuronides. It is believed to be the major photoproduct excreted with bile and urine in newborn infants. Lumirubin formation is not only a wavelength-dependent process, but its formation is also stimulated by higher light intensities (12). The greater understanding of the BR photoconversion processes has led to the general conclusion that presently used phototherapy devices have suboptimal intensity. This is underscored by a study which reported that double phototherapy with high irradiance devices shortens the duration of hyperbilirubinemia when compared with the use of single conventional phototherapy devices (13). Furthermore, Ennever et al. (14) suggested that "if a method for conveniently delivering phototherapy of much higher intensity were developed without attendant problems associated with high intensity, tungsten filament sources, it could provide substantial improvement in the efficacy of phototherapy." We believe that the use of LEDs may be such a method.
In addition, Pratesi et al. (3,15) have suggested that two light sources of different wavelengths would be the most ideal form of phototherapy. A narrow spectrum short wavelength light (e.g. blue) of relatively low intensity would excite BR to form excretable lumirubin, whereas longer intense wavelength light (e.g. green) would reconvert Z, E BR, formed as a by-product of blue irradiation, to native (Z, Z) BR. However, these authors in a later communication found that lumirubin formation in vivo is optimal with blue-green light (12). Recently, Donzelli et al. (16) have reported results of 24-h phototherapy with narrow spectrum blue-green lamps that appeared to be two times more efficient than special blue lamps in decreasing plasma BR in low birth weight neonates. They ascribe this greater phototherapeutic efficacy to a combination of factors, including a higher quantum yield of lumirubin, lower quantum yield of Z, E BR, and skin effects that favor the greater transmission of green over blue light. Our present results show that photooxidation is most strongly supported by blue light, but even blue-green and green light significantly photodegrade BR (Fig. 3), hinting that the process of photooxidation, in addition to lumirubin formation, may play a greater role in BR degradation than is presently accepted. LEDs may be the most practical light sources available for testing the various hypotheses in vitro and in vivo, and for designing clinical devices that can take full advantage of BR photodynamics.
The decreases in the A460 nm we have observed may have been mediated by the processes of photooxidation, photocyclization to lumirubin, or a combination of both. According to Ennever et al. (17), the formation of Z, E isomers is not expected to affect the absorbance maximum or the molar extinction coefficient of a Z, Z BR-HSA solution upon light exposure. Furthermore, in humans, Z, E isomer formation does not significantly contribute to increased BR removal. Thus, when absorbance is measured after light exposure as in our experiments, only the mechanism of photooxidation and photocyclization are expected to contribute to the decrease in absorbance. Although, McDonagh and Lightner (11) state that "...predictions about the mechanism of phototherapy that are based exclusively on in vitro photochemical models should be made and viewed with circumspection," they also state that "in the presence of HSA therefore photocyclization is about two orders of magnitude less efficient than configurational isomerization, and perhaps only about as efficient as photooxidation of bilirubin." Furthermore, it has also been shown (11) that lumirubin has an absorbance maximum at 453 nm and a molar extinction coefficient of 33,000 A units·cm-1·M-1, which is approximately 70% of the value (A460 nm = 47,000 A units·cm-1·M-1) reported for Z, Z BR-HSA (18). As a result, we cannot state with certainty that the observed decrease in absorbance of our reaction media associated with light exposure is due to photooxidation of BR to colorless products or to lumirubin formation or to a combination of both processes. In addition, it has been established that lumirubin formation is favored by longer wavelength light so that the lumirubin formation may be greater with blue-green and green LEDs than with blue. Therefore, in our experiments under these conditions, we may have affected a greater rate of degradation of Z, Z BR-HSA than is indicated by the decrease in absorbance we have reported. For instance, for each unit of A460 nm lost due to photoalteration of Z, Z BR-HSA, colorless photoproducts may have formed or 0.7 A units may have been generated due to the formation of lumirubin. Thus, we can conclude that the photodegradation of Z, Z BR-HSA complex is at least as great as is indicated by the decrease in absorbance at A460 nm. Issues regarding the quantitative contributions of the two processes are beyond the scope of this communication.
When combined into arrays of 100 LEDs, we found that the overlapping light of three such units had greater irradiance than any of the conventional light sources tested. Measurements of light intensity are of questionable significance because their magnitudes are solely dependent upon the wavelength range of the detector, which may not coincide with the action spectrum of the photochemical process being evaluated. The clinically used Joey® Dosimeter measures light intensity only over the range of 420-480 nm, which closely matches the absorption spectrum of BR. However, the results in Figs. 3 and 4 show that substantial photobleaching of BR occurs with light well outside this range, i.e. green (Fig. 2) and the Joey® Dosimeter readings do not correlate with the magnitude of the photochemical effects on BR. Light intensity readings with the Extech light meter, a broad band detector, in contrast, appears to more closely correspond to the observed effects on BR degradation with the narrow spectrum LEDs. Obviously, irradiance measurements need to be made over the entire action spectrum of the photochemical processes under study.
The prototype blue LED device photobleached BR at a higher rate than the conventional phototherapy devices (Fig. 4). However, these in vitro results do not necessarily reflect the clinical efficacy of the latter. Clinical studies are in progress at Bikur Cholim Hospital in Jerusalem comparing the efficacy of blue- and blue-green LED devices with that of conventional phototherapy units.
Because of their inherent safety characteristics, LED-based phototherapy devices can be placed in close proximity to the patient than can conventional devices (Fig. 4). For instance, through incorporation into pads, blankets, or jackets, lamp and chip LEDs can deliver higher light intensities and cover a larger body surface area than that achieved by presently used devices. Presently available commercial blankets or pads are limited in surface area due to the limited intensity of their light sources or the capacity of the fiberoptic light conduction cable. However, LED-containing rigid or flexible contact devices can be manufactured to any size and shape to deliver optimal intensity and maximal surface area exposure. The relatively low power requirements (0.1 W/LED) of this light source makes phototherapy during vehicular transport possible through use of battery power.
LEDs also allow selectability of the phototherapy wavelength band, which may offer additional in vivo benefits. BR photobleaching occurs at relatively high rates in green light, which has greater skin penetration and, in turn, may offset in vivo its somewhat lower (in vitro) efficacy. Furthermore, green light appears to have fewer side effects because it is less likely to be absorbed by endogenous photosensitizers, such as vitamin B6 (riboflavin), which will produce singlet oxygen when irradiated by blue light (19). This singlet oxygen may not only react with BR, but also with other organic compounds and cause photodamage and decreased riboflavin levels in some developing neonates (4,6). The effects of administration of photosensitizing drugs, such as propanolol, hydrochlorothiazide, and others (20,21) in conjunction with phototherapy may also be minimized though selection of the most appropriate light quality (color). For example, upon administration of tin protoporphyrin, an experimental antihyperbilirubinemic drug (22), some Greek neonates were reported to develop rashes upon phototherapy with broad wavelength light. Phototherapy with more appropriate narrow wavelength light sources may prevent such reactions.
In summary, because of their small size, high luminous intensity, and their narrow wavelength band light, LEDs may be an attractive light source for phototherapy not only for newborns, but also for other patients suffering from excessive hyperbilirubinemia, such as that caused by the Crigler-Najjar syndrome.
Abbreviations
- BR:
-
bilirubin
- LED:
-
visible light-emitting diode
- VDC:
-
volt direct current
- HSA:
-
human serum albumin
References
Ennever JF 1990 Blue light, green light, white light, more light: treatment of neonatal jaundice. Clin Perinatol 17: 467–481
Maisels MJ 1996 Why use homeopathic doses of phototherapy? Pediatrics 98: 283–287
Agati G, Fusi F, Pratesi R 1985 Configurational photoisomerization of bilirubin in vitro II. A comparative study of phototherapy fluorescent lamps and lasers. Photochem Photobiol 41: 381–392
Ente G, Klein SW 1970 Hazards of phototherapy [Letter]. N Engl J Med 283: 544–545
Porat R, Gilbert S, Magilner D 1996 Methylene blue-induced phototoxicity: an unrecognized complication. Pediatrics 97: 717–721
Sisson TRC 1987 Photodegradation of riboflavin in neonates. Fed Proc 46: 1883–1885
Fasol G 1997 Longer life for the blue laser. Science 278: 1902–1903
Nakamura S, Fasol G 1997 InGaN single-quantum-well LEDs. In: The Blue Laser Diode. Springer-Verlag, Berlin, pp 201–221.
Vreman, HJ, Stevenson, DK 1990 Metalloporphyrin-enhanced photodegradation of bilirubin in vitro. Am J Dis Child 144: 590–594
Forte VC 1997 The evolution of LEDs. EDN Products Edition, Cahners Publishing Co., Highlands Park, CO, p 24
McDonagh AF, Lightner DA 1988 Phototherapy and the photobiology of bilirubin. Semin Liver Dis 8: 272–283
Agati G, Fusi F, Donzelli GP, Pratesi R 1993 Quantum yield and skin filtering effect on the formation rate of lumirubin. J Photochem Photobiol B Biol 17: 173–180
Kang JH, Shankaran S 1995 Double phototherapy with high irradiance compared with single phototherapy in neonates with hyperbilirubinemia. Am J Perinatol 12: 178–180
Ennever JF, Knox I, Speck WT 1986 Differences in bilirubin isomer composition in infants treated with green and white light phototherapy. J Pediatr 109: 119–122
Pratesi R 1983 Two lights for phototherapy [Letter]. Lancet 2: 859
Donzelli GP, Pratesi S, Rapisardi G, Agati G, Fusi F, Pratesi R 1995 1-day phototherapy of neonatal jaundice with blue-green lamp [Letter]. Lancet 346: 184–185
Ennever JF, McDonagh AF, Speck WT 1983 Phototherapy for neonatal jaundice: optimal wavelengths of light. J Pediatr 103: 295–299
Lee KS, Gartner LM 1976 Spectrophotometric characteristics of bilirubin. Pediatr Res 10: 782–788
Sanvordeker DR, Kostenbauder HB 1974 Mechanism for riboflavin enhancement of bilirubin photodecomposition in vitro. J Pharmaceut Sci 63: 404–408
Roberts JE, Remé CE, Dillon J, Terman M 1992 Exposure to bright light and the concurrent use of photosensitizing drugs [Letter]. N Engl J Med 326: 1500–1501
Beijersbergen van Henegouwen GMJ 1991 New trends in photobiology (invited review). J Photochem Photobiol B Biol 10: 183–210
Ford FL, Gold J 1990 Phototoxicity of tin protoporphyrin, tin mesoporphyrin, and tin diiododeuteroporphyrin under neonatal phototherapy conditions. Pediatrics 84: 1031–1037
Acknowledgements
The authors thank Randy Reeve and Michael Philpott for technical advice on biomedical safety issues and the Opto-Electronic Division of Hewlett-Packard Co., San Jose, CA, for the circuit boards used in the prototype phototherapy device.
Author information
Authors and Affiliations
Additional information
Supported by the National Institutes of Health Grant HD14426, the Hess Research Fund, the Mary L. Johnson Research Fund, and a grant from the Stanford University Office of Technology Licensing.
The Stanford University Office of Technology Licensing has filed a patent application (No. 08/824, 631) for "Phototherapy of Jaundiced Newborns Using Semiconductor Light-Emitting Diodes (LEDs)" with the U.S. Patent and Trademark Office.
Rights and permissions
About this article
Cite this article
Vreman, H., Wong, R., Stevenson, D. et al. Light-Emitting Diodes: A Novel Light Source for Phototherapy. Pediatr Res 44, 804–809 (1998). https://doi.org/10.1203/00006450-199811000-00027
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199811000-00027
This article is cited by
-
Is neonatal phototherapy associated with a greater risk of childhood cancers?
BMC Pediatrics (2022)
-
LED-phototherapy does not induce oxidative DNA damage in hyperbilirubinemic Gunn rats
Pediatric Research (2019)
-
Low-cost photodynamic therapy devices for global health settings: Characterization of battery-powered LED performance and smartphone imaging in 3D tumor models
Scientific Reports (2015)
-
Intravenous Immunoglobulin G Treatment in ABO Hemolytic Disease of the Newborn, is it Myth or Real?
Indian Journal of Hematology and Blood Transfusion (2014)
-
The effect of hematocrit on the efficacy of phototherapy for neonatal jaundice
Pediatric Research (2013)