Abstract
The epidermal permeability barrier, required for terrestrial life, is localized to lipid-enriched lamellar membranes in the extracellular spaces of the stratum corneum (SC). Immaturity of the SC is a significant contributor to morbidity and mortality in premature infants. Previous studies have shown that supraphysiologic concentrations of thyroid hormone accelerate epidermis/SC ontogenesis. Here we studied SC development in Hyt/Hyt mice who are genetically hypothyroid due to a mutation in the TSH receptor. In control mice on d 18 of gestation (term 19.5 d), only focal areas displayed a mature SC membrane pattern. By 19 d of gestation there was a mature multilayered SC with lamellar unit structures filling the extracellular spaces similar to that seen in mature mice. In Hyt/Hyt mice SC development was delayed at both 18 and 19 d of gestation. In both strains of mice, within the first day after birth there were no differences in epidermal or SC appearance, and the SC was fully mature. These findings indicate that thyroid hormone plays a physiologic role during normal intrauterine development of the SC. However, normal SC maturation ultimately occurs, indicating that thyroid hormone is not absolutely essential. Previous studies have shown that glucocorticoids accelerate SC development in euthyroid rats, and in the present study we demonstrate that glucocorticoids also accelerate SC ontogenesis in euthyroid mice. In contrast, in Hyt/Hyt mice glucocorticoids did not accelerate or normalize SC development, indicating that the glucocorticoid effect on SC maturation requires a euthyroid state or that glucocorticoids act via thyroid hormone. These studies demonstrate that thyroid hormone status is an important regulator of fetal SC development.
Similar content being viewed by others
Main
The major function of the epidermis is the formation of the SC, the outermost layer of the epidermis, which separates the predominantly aqueous organism from the xeric environment. The epidermal permeability barrier, whose formation is a prerequisite for terrestrial life, is localized to the extracellular spaces of the SC where it is mediated by lamellar membranes enriched in nonpolar lipids(1, 2). These lipids are delivered to the extracellular spaces of the SC by the exocytosis of lamellar bodies from keratinocytes in the upper epidermis(1, 2). Immaturity of the SC, leading to barrier incompetence, is a significant contributor to the morbidity and mortality of the premature infant(3, 4). The increased loss of fluid and electrolytes, as well as increased evaporative heat loss, which raises caloric requirements, are consequences of permeability barrier immaturity(3–7). Moreover, sepsis from normal skin bacterial and fungal flora is a consequence of a poorly developed SC with deficient barrier properties in very low birth weight infants(4).
Our laboratory has examined epidermal and, more specifically, SC ontogenesis in the fetal rat(8). On d 17 of gestation (term = 22 d) the epidermis is comprised of a basal layer, often an intermediate layer, and a periderm, completely lacking any cornified layers. By d 19 of gestation the epidermis has thickened, a multilayered stratum spinosum is present, and a granular layer is becoming evident. However, the SC, when present, is still immature (1-2 cell layers versus 8-10 layers in postnatal epidermis), and the extracellular lamellar membranes display an irregular pattern of foreshortened lamellae indicative of immature membranes. At this stage of development, the cutaneous permeability barrier is incompetent. By d 21 of gestation the epidermis has thickened further, and a well developed stratum spinosum and stratum granulosum are present. A multilayered, mature appearing SC is present. Moreover, the extracellular spaces of the SC are completely filled with basic lamellar membrane unit structures, characteristic of adult SC(2). In parallel with these structural changes the SC becomes resistant to water movement, and a competent permeability barrier is established.
The timetable of ontogenesis of the epidermis/SC in rodents and humans coincides with the timetable of lung development(9–12). Moreover, as in the lung, a number of hormones have been shown to regulate epidermal/SC development in vivo and in vitro, when given in supraphysiologic doses(9, 13, 14). Glucocorticoids, estrogens, and thyroid hormone accelerate, whereas androgens delay epidermis/SC formation(9, 13, 14). We have recently developed an in vitro model for fetal rat epidermis/SC development in which the formation of the epidermis/SC and permeability barrier closely parallels in vivo ontogenesis and occurs in hormone- and growth factor-free media(9). Thus, whether any of these hormones plays an obligatory physiologic role during normal intrauterine development of the epidermis/SC is unknown.
Hyt/Hyt mice are genetically hypothyroid due to a mutation in the TSH receptor leading to a marked reduction in thyroid hormone production(15–17). Moreover, lung development is impaired in Hyt/Hyt mice(18). We studied epidermis/SC development in Hyt/Hyt mice to determine whether physiologic levels of thyroid hormones are required for normal fetal epidermis/SC ontogenesis.
METHODS
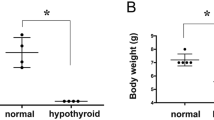
Animals. The colony of genetically hypothyroid mice was established in Pittsburgh from homozygous (Balb Hyt/Hyt) males and heterozygous (Balb Hyt/+) females (Jackson Laboratories, Bar Harbor, ME). Homozygous (Hyt/Hyt) males and females were identified by a high serum TSH and low serum-free T4 levels and were bred to obtain Hyt/Hyt pups (Table 1). During the breeding period these mice received T3 in the drinking water (0.2 μg/mL). This resulted in the pregnant hypothyroid animals having TSH and T4 levels in the normal range. Females were separated from the males after mating (positive vaginal plug = d 1 of pregnancy, term, ≈19.5 d). To ensure fetal hypothyroidism, T3 supplementation was stopped at d 12 of gestation(18). Balb/c (+/+) mice served as euthyroid controls. In some experiments pregnant animals were treated twice a day with betamethasone (2.5 mg/kg i.p.) on d 16 and 17, and fetuses were examined on d 18.
TSH assay. Serum TSH levels were measured using a specific RIA for rat serum TSH (Amersham Corp., Arlington Heights, IL) that cross-reacts with mouse TSH(18).
Free T4 assay. Serum-free T4 was quantitated using a commercially available RIA kit (Incstar, Stillwater, MN, free T4 two-step gamma coat assay).
Light microscopy. Skin samples were obtained in Pittsburgh, underwent initial processing, were coded, and then mailed to San Francisco for analysis. Samples were analyzed in San Francisco without knowledge of the specific age or treatment protocol. Sections (0.5 μm) of skin from the lower portion of the anterior abdominal wall were fixed in modified Karnovsky's fixative, Epon-embedded, and stained with toluidine blue for light microscopy. Parallel samples were frozen in OCT embedding compound (Miles Scientific, Naperville, IL) in liquid nitrogen and stored at -70 °C. Nile red was applied to 5-μm frozen sections and examined with a Leitz microscope equipped for epifluorescence (excitation 489 nm, emission 515 nm), as described previously(8, 19).
Electron microscopy. Samples for electron microscopy were minced and fixed in modified Karnovsky's fixative and post-fixed in reduced 1% osmium or buffered 0.2% ruthenium tetroxide with 0.5% ferrocyanide. The samples were dehydrated in graded ethanol, embedded in Epon, sectioned, and examined in a Zeiss electron microscope at 60 kV(8). Samples were evaluated in San Francisco without knowledge of the specific gestational age or treatment protocol. The figures shown for both light and electron microscopy are representative of the changes observed in samples obtained from several animals.
RESULTS
To determine the effect of intrauterine hypothyroidism on fetal epidermal/SC development, we examined the morphology by light and electron microscopy of skin samples from control and Hyt/Hyt mice at 18 and 19 d of gestation (term, 19.5 d) and 1 d postpartum.
Day 18. On d 18 of gestation control epidermis (n = 3) displayed a well developed stratum spinosum and a multilayered granular layer as indicated by prominent keratohyalin granules (Fig. 1A). Nile red lipid histochemistry demonstrated a diffuse cytoplasmic staining pattern in the outer epidermal layers, a pattern indicative of immaturity (Fig. 2A). On electron microscopy lamellar bodies were present in the upper epidermis, and secreted lamellar contents were evident at the stratum granulosum-SC interface (not shown). Two to three SC layers were present, but only in focal areas did membranes in the SC interstices display a mature pattern (Fig. 3A1); in other areas the secreted lamellar membranes had not yet transformed into mature unit structures (Fig. 3A2). These results show that in comparison to postnatal mice where mature lamellar unit structures fill the interspaces of a multilayered SC (Fig. 3, inset), the SC in 18-d control skin was not yet fully mature.
Light microscopy photomicrographs of control and hypothyroid epidermis during SC development (A-F) and after prenatal β-methasone treatment (G and H). Epon-embedded sections (0.5 μm) were stained with toluidine blue. Eighteen-day control epidermis displays a multilayered stratum granulosum (A, brackets) with prominent keratohyalin granules. The granular layer is less distinct in 18-d hypothyroid epidermis (B) with smaller keratohyalin granules. Periderm is prominently stained (arrowheads). By d 19, keratohyalin granules are large and numerous, and a multilayered SC is present in control epidermis (C, brackets). Hypothyroid d 19 animals exhibit smaller keratohyalin granules and lack a well defined SC (D). Postpartum d 1 animals, both control (E) and hypothyroid (F), exhibit a multilayered SC (brackets). Pregnant mice were treated twice daily with β-methasone (on d 16 and 17), and fetuses were examined on d 18, as described in “Methods.” A multilayered SC is also seen in β-methasone-treated d 18 control animals, indicating accelerated maturation (G, brackets). Hypothyroid animals treated with β-methasone lack a well defined SC (H). Bar = 8 μm.
Lipid histochemistry of control and hypothyroid epidermis during SC development. Frozen sections (5 μm) were stained with the lipid probe Nile red. Epidermis from d 18 control (A) and hypothyroid (B) animals display similar immature cytosolic patterns of fluorescence. Control d 19 epidermis stains in a membrane pattern throughout a multilayered SC (C, arrows). In contrast, a less mature pattern of membrane fluorescence is present in hypothyroid d 19 epidermis, with membrane pattern staining evident only in localized areas (D, arrows). A mature pattern of membrane staining is present in both postpartum d 1 control (E) and hypothyroid (F) epidermis (arrows). After treatment with β-methasone (as described in Fig. 1), control epidermis displays a mature pattern of SC membrane staining (G, arrows). In contrast, a cytoplasmic pattern of staining persists in β-methasone-treated hypothyroid epidermis (H). Bar = 8 μm.
Ultrastructure of control and hypothyroid epidermis during SC development: (A) 18-d control (C-18); inset, newborn control (C-NB); (B) 18-d hypothyroid (Hyp-18; inset, lamellar bodies in Hyp-18); (C) 19-d hypothyroid (Hyp-19); (D) 18-d hypothyroid, treated with β-methasone (Hyp-18 + Dex). Solid arrows depict mature intercellular lamellae, open arrows depict incompletely processed, intercellular lamellae. SC, stratum corneum; SG, stratum granulosum. All samples were fixed in ruthenium tetroxide. Bars = 0.25 μm.
On d 18 of gestation Hyt/Hyt epidermis (n = 5) displayed a thinner, less distinct granular layer with smaller keratohyalin granules than d 18 controls (Fig. 1, B versus A). Like control epidermis, Nile red staining of Hyt/Hyt epidermis revealed an immature cytoplasmic staining pattern (Fig. 2B). On electron microscopy, lamellar body number, lamellar body substructure, and the quantity of secreted lamellar body-derived material in SC interstices appeared similar in 18-d Hyt/Hyt and control mice (Fig. 3B). However, in contrast to 18-d controls, Hyt/Hyt mice displayed a thinner SC of only one or two cell layers with uniformly immature, incompletely processed, intercellular lamellae (Fig. 3B). These observations indicate that the development of the epidermis and SC in Hyt/Hyt mice is delayed in comparison to gestational d 18 euthyroid controls.
Day 19. By d 19 of gestation control animals (n = 3) displayed larger and more numerous keratohyalin granules and a well developed, multilayered SC by light microscopy (Fig. 1C). Moreover, Nile red histochemical staining revealed a mature pattern of membrane pattern staining throughout the uppermost epidermis (Fig. 2C). Furthermore, electron microscopy demonstrated a multilayered SC with mature lamellar unit structures filling the extracellular spaces (data not shown), similar to that seen in newborn mice (Fig. 3, inset, C-NB).
In contrast, Hyt/Hyt epidermis at 19 d of gestation (n = 3) remained immature by light microscopy with fewer and smaller keratohyalin granules (Fig. 1D) and lacked a well defined SC. Nile red histochemistry revealed only localized areas of membrane pattern staining in the outer epidermis (Fig. 2D). Yet, despite a thin SC, by electron microscopy, mature, extracellular lamellar structures predominated (Fig. 3C). These results show that the developmental delay in Hyt/Hyt mice persists through d 19.
Postnatal d 1. By the first day after birth the light microscopic appearance of the epidermis of control (n = 3) and Hyt/Hyt (n = 3) mice was similar (Fig. 1,E and F). In both strains of mice a multilayered, mature SC was apparent, and no differences in either granular layer or in total epidermal thickness were observed. With Nile red staining, both controls and Hyt/Hyt mice displayed a multilayered SC, with staining in a mature, membrane pattern (Fig. 2,E and F). Intense staining was sometimes observed in the outermost layer of the SC, perhaps due to remnants of the periderm or to folding of the SC. Electron microscopy confirmed these findings, demonstrating a multilayered SC with mature lamellar unit structures filling the interstices in both control and Hyt/Hyt animals (Fig. 3, inset, C-NB, Hyt/Hyt not shown). Thus, in contrast to d 18 and 19 of gestation, by 1 d postpartum, the appearance of the epidermis/SC is identical in both control and hypothyroid mice.
Effect of maternal glucocorticoids on epidermal/sc development. Previous studies have shown that glucocorticoids accelerate SC development in euthyroid rats(9, 13). We next determined whether glucocorticoid therapy could normalize SC ontogenesis in hypothyroid mice. Betamethasone was administered to control (n = 3) and Hyt/Hyt (n = 3) mice twice daily on d 16 and 17 of gestation. In d 18 control mice treated with glucocorticoids, light microscopy revealed a multilayered SC (Fig. 1G), and Nile red staining demonstrated a mature membrane pattern in the SC (Fig. 2G). Similar to the postnatal d 1 samples, intense staining was sometimes observed in the outermost SC layer. Electron microscopy revealed a multilayered SC with the interstices filled with mature lamellae. Thus, the 18-d glucocorticoid-treated epidermis displayed a morphologic appearance similar to 19-d control epidermis, demonstrating accelerating SC ontogenesis, as seen in previous studies in fetal rats(9, 13).
In contrast, at d 18 of gestation, betamethasone-treated Hyt/Hyt mice still displayed an immature granular layer on light microscopy with virtually no SC (Fig. 1H). Furthermore, no membrane pattern of staining was seen in the upper epidermis with Nile red histochemistry (Fig. 2H). Finally, on electron microscopy only one or two layers of SC were seen, with scattered extracellular lamellae, which were predominantly immature (Fig. 3D). Thus, the appearance of the epidermis at d 18 of gestation in Hyt/Hyt mice treated with glucocorticoids was very similar to that of untreated Hyt/Hyt mice, i.e. it continued to display retarded epidermis/SC development. These studies indicate that glucocorticoids do not accelerate or normalize epidermis/SC development in hypothyroid animals.
DISCUSSION
Previous studies by our laboratory have demonstrated that supraphysiologic concentrations of T3 accelerate epidermal/SC formation in fetal rat skin explants, grown in hormone- and serum-free medium(9). Whether this in vitro observation is relevant for normal intrauterine development is unknown. The present study extends these observations and demonstrates that intrauterine hypothyroidism delays SC development in the intact animal. This finding indicates that thyroid hormone plays a physiologic role during normal intrauterine development of the SC. Yet, although SC formation is delayed in the hypothyroid animals, normal SC development ultimately occurs. These findings agree with our in vitro experiments where supraphysiologic concentrations of thyroid hormone accelerate SC development in fetal rat explants, but normal development occurs even in the absence of hormones(9).
Ontogenesis of the lung and the epidermis have a similar timetable of development with both maturing in the last trimester(3, 8, 10–12). Both lung and SC maturation involve the formation of organized, extracellular lipid structures at an air-tissue interface; and in both tissues, the delivery of lipids occurs via lamellar body secretion(3, 8, 10–12). Moreover, similar to the epidermis, lung development in vivo and in vitro is also accelerated by thyroid hormone(20, 21). Furthermore, lung development in vitro occurs normally, albeit more slowly in the absence of hormones(21). Finally, previous studies have shown that there is delayed lung maturation in Hyt/Hyt hypothyroid mice(18). Thus, the fetal development of both the lung and the epidermis are regulated by thyroid status of the animal.
The mechanism by which thyroid hormone stimulates SC development is unknown. Nuclear receptors for thyroid hormone are present in adult skin, and thyroid hormone induces a variety of alterations in the epidermis(22–24). T3 stimulates epidermal lipid synthesis(25). Endogenous lipid synthesis is required for the formation of a normal SC and a competent permeability barrier(26–28). Additionally, T3 increases the number of EGF receptors in the skin(29), and the binding of a number of EGF receptor ligands, such as transforming growth factor-α and EGF, plays a very important role in epidermal growth(30). EGF receptor knockout mice display a hypoplastic epidermis(31–33). Finally, T3 stimulates plasminogen activator, which has a key role in facilitating the migration of keratinocytes during wound healing(34). Whether these or other metabolic changes induced by thyroid hormone account for the effects on fetal SC development remains to be determined.
Previous studies have shown that glucocorticoids accelerate SC development when given to intact pregnant rats or when added to fetal explants in vitro(9, 13). In the present study we observed that glucocorticoid treatment also accelerates epidermis/SC formation in Balb/c control mice. However, glucocorticoid administration to Hyt/Hyt hypothyroid mice did not accelerate SC development. These results suggest that the glucocorticoid effect on SC formation requires either a euthyroid state or that the mechanism of action of glucocorticoids occurs via thyroid hormone. For example, studies have shown that glucocorticoids stimulate the conversion of T4 to the more active hormone, T3(35), a reaction that occurs in skin. Additionally, studies have shown that hypothyroid animals have reduced glucocorticoid receptors in the liver(36).
In summary, the present study demonstrates that thyroid hormone status is an important regulator of fetal SC development.
Abbreviations
- SC:
-
stratum corneum
- T3:
-
triiodothyronine
- T4:
-
thyroxine
- EGF:
-
epidermal growth factor
References
Elias PM 1983 Epidermal lipids, barrier function and desquamation. J Invest Dermatol 80: 44–49.
Elias PM, Menon GK 1991 Structural and lipid biochemical correlates of the epidermal permeability barrier. Adv Lipid Res 24: 1–26.
Vernon HJ, Lane AT, Wischerath LJ, Davis JM, Menegus MA 1990 Semi-permeable dressing and transepidermal water loss in premature infants. Pediatrics 86: 357–362.
Cartlidge PHT, Rutter N 1992 Skin barrier function. In: Polin RA, Fox WW (eds) Fetal and Neonatal Physiology. WB Saunders, Philadelphia, pp 569–585.
Belgaumkar JK, Scott KE 1975 Effects of low humidity on small premature infants in servocontrol incubators. I. Decrease in rectal temperature. Biol Neonate 26: 337–347.
Lorenz JM, Kleinman LI, Kotagal UR, Rellar MD 1982 Water balance in very low birth weight infants: relationship to water and sodium intake and effect on outcome. J Pediatr 101: 423–432.
Maurer A, Micheli JL, Schuetz Y, Fregmond D, Jeguier E 1984 Transepidermal water loss and resting energy expenditure in preterm infants. Helv Paediatr Acta 39: 405–418.
Aszterbaum M, Menon GK, Feingold KR, Williams ML 1992 Ontogeny of the epidermal barrier to water loss in the rat: correlation of function with stratum corneum structure and lipid content. Pediatr Res 31: 308–317.
Hanley K, Rassner U, Elias PM, Williams ML, Feingold KR 1996 Epidermal barrier ontogenesis: Maturation in serum-free media and acceleration by glucocorticoids and thyroid hormone but not selected growth factors. J Invest Dermatol 106: 404–411.
Bourbon JR, Farrell PM, Doncet E, Brown DJ, Valenza C 1987 Biochemical maturation of fetal rat lung: a comprehensive study including surfactant determination. Biol Neonate 52: 48–60.
Schellhase DE, Emrie PA, Fisher JH, Shannon JM 1989 Ontogeny of surfactant apoproteins in the rat. Pediatr Res 26: 167–174.
Hodson WA 1992 Normal and abnormal structural development of the lung. In: Polin RA, Fox WW (eds) Fetal and Neonatal Physiology. WB Saunders, Philadelphia, pp 771–782.
Aszterbaum M, Feingold KR, Menon GK, Williams ML 1993 Glucocorticoids accelerate fetal maturation of the epidermal permeability barrier in the rat. J Clin Invest 91: 2703–2708.
Hanley K, Rassner U, Jiang Y, Vansomphone D, Crumrine D, Komuves L, Elias PM, Feingold KR, Williams ML 1996 Hormonal basis for the gender difference in epidermal barrier formation in the fetal rat. Acceleration by estrogen and delay by testosterone. J Clin Invest 97: 2576–2584.
Beamer WG, Eicher EM, Maltais LJ, Southard JL 1981 Inherited primary hypothyroidism in mice. Science 212: 61–62.
Beamer WG, Cresswell LA 1982 Defective thyroid ontogenesis in fetal hypothyroid (hyt/hyt) mice. Anat Rec 202: 387–393.
Stein SA, Zakarija M, McKenzie JM, Shanklin DR, Adams PM 1991 The site of molecular defect in the thyroid gland of the hyt/hyt mouse: abnormality in the TSH receptor-G protein adenyl cyclase complex. Thyroid 1: 257–265.
de Mello DE, Heyman S, Govindarajan R, Sosenko IRS, Devaskar UP 1994 Delayed ultrastructural lung maturation in the fetal and newborn hypothyroid (Hyt/Hyt) mouse. Pediatr Res 36: 380–386.
Grubauer G, Elias PM, Feingold KR 1989 Transepidermal water loss: the signal for recovery of barrier structure and function. J Lipid Res 30: 323–334.
Pope TS, Rooney SA 1987 Effects of glucocorticoid and thyroid hormones on regulatory enzymes of fatty acid synthesis and glycogen metabolism in developing fetal rat lung. Biochim Biophys Acta 918: 141–148.
Ballard PL 1989 Hormonal regulation of pulmonary surfactant. Endocrinol Rev 10: 165–178.
Holt PJ, Lazarus J, Marks R 1976 The epidermis in thyroid disease. Br J Dermatol 95: 513–518.
Holt PJ, Marks R 1977 The epidermal response to changes in thyroid status. J Invest Dermatol 68: 299–301.
Torma H, Rollman O, Vahlquist A 1993 Detection of mRNA transcripts for retinoic acid, vitamin D3 and thyroid hormone (C-erb-A) nuclear receptors in human skin using reverse transcription and polymerase chain reaction. Acta Dermato-Venereol 73: 102–107.
Rosenberg RM, Isseroff RR, Ziboh VA, Huntley AC 1986 Abnormal lipogenesis in thyroid hormone deficient epidermis. J Invest Dermatol 86: 244–248.
Feingold KR, Man MQ, Menon GK, Cho SS, Brown BE, Elias PM 1990 Cholesterol synthesis is required for cutaneous barrier function in mice. J Clin Invest 86: 1738–1745.
Holleran WM, Man MQ, Gao WN, Menon GK, Elias PM, Feingold KR 1991 Sphingolipids are required for mammalian barrier function: inhibition of sphingolipid synthesis delays barrier recovery after acute perturbation. J Clin Invest 88: 1338–1345.
Man MQ, Elias PM, Feingold KR 1993 Fatty acids are required for epidermal barrier function. J Clin Invest 92: 791–798.
Hoath SB, Lakshmanan J, Fisher DA 1985 Epidermal growth factor binding to neonatal mouse skin explants and membrane preparations-effect of triiodothyronine. Pediatr Res 19: 277–281.
King LE, Gates RE, Stoscheck CM, Nanney LB 1990 The EGF/TGF alpha receptor in skin. J Invest Dermatol 94: suppl 164S–170S.
Threadgill DW, Dlugosz AA, Hansen LA, Tennenbaum T, Lichti U, Yee D, LaMantia C, Mourton T, Herrup K, Harris RC, Barnard JA, Yuspa SH, Coffey RJ, Magnuson T 1995 Targeted disruption of mouse EGF receptor: effect of genetic background on mutant phenotype. Science 269: 230–234.
Sibilia M, Wagner EF 1995 Strain-dependent epithelial defects in mice lacking the EGF receptor. Science 269: 234–238.
Miettinen PJ, Berger JE, Meneses J, Phung Y, Pedersen RA, Werb Z, Derynck R 1995 Epithelial immaturity and multiorgan failure in mice lacking epidermal growth factor receptor. Nature 376: 337–341.
Isseroff RR, Chun KT, Rosenberg RM 1989 Triiodothyronine alters the cornification of cultured human keratinocytes. Br J Dermatol 120: 503–510.
Polk DH, Fisher DA 1995 Fetal and neonatal endocrinology. In: De Groot L (ed) Endocrinology, Vol 3. WB Saunders, Philadelphia, 2239–2257.
Coustaut M, Pallet V, Garcin H, Higueret P 1996 The influence of dietary vitamin A on triiodothyronine, retinoic acid and glucocorticoid receptors in liver of hypothyroid rats. Br J Nutr 76: 295–306.
Acknowledgements
The authors appreciate the excellent secretarial assistance of Pamela Herranz.
Author information
Authors and Affiliations
Additional information
Supported by a grant from the Magee Women's Research Institute, National Institutes of Health Grants HD29707, AR19098, PO39448, HL52839, and AR39639, and the Medical Service, Department of Veterans Affairs Medical Center.
Rights and permissions
About this article
Cite this article
Hanley, K., Devaskar, U., Hicks, S. et al. Hypothyroidism Delays Fetal Stratum Corneum Development in Mice. Pediatr Res 42, 610–614 (1997). https://doi.org/10.1203/00006450-199711000-00010
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199711000-00010
This article is cited by
-
The polarity protein Scrib mediates epidermal development and exerts a tumor suppressive function during skin carcinogenesis
Molecular Cancer (2015)
-
PPARδ Activation Promotes Stratum Corneum Formation and Epidermal Permeability Barrier Development during Late Gestation
Journal of Investigative Dermatology (2010)