Abstract
The role of adenosine in the modulation of respiration-related neurons was examined using an in vitro brainstem-spinal cord preparation from neonatal rats (0-4 d old). Respiratory activity was recorded from the C4 or C5 ventral roots by suction electrodes and from inspiratory related neurons (I neurons) in the rostral ventrolateral medulla by microelectrodes. The following substances were added to the preparation superfusate, and their effect was evaluated: the adenosine A1 receptor agonist N6-(2-phenylisopropyl)adenosine, R(-)isomer (R-PIA), the adenosine uptake blocker dipyridamole, the adenosine receptor antagonist theophylline, and the specific A1 receptor antagonist 8-cyclopentyl-1,3-dipropylxanthine (DPCPX). R-PIA and dipyridamole decreased the activity of I neurons and the C4 respiratory burst rate. Furthermore, these compounds induced a significantly more irregular respiratory rate in three-quarters of preparations from the youngest animals (<48 h old) compared with that of controls. Theophylline or DPCPX reversed the effects of both R-PIA and dipyridamole on respiratory rate, regularity of respiratory rate, inspiratory time, amplitude, and intra-burst frequency of I neurons. Thus, adenosine depresses both the I neurons in the rostral ventrolateral medulla and the respiratory motor output. This depression of I neurons and respiratory rate can be abolished by theophylline primarily through a blockade of medullary adenosine A1 receptors. An age-dependent correlation of the effects of R-PIA and dipyridamole, with a more pronounced decrease in respiratory activity in preparations from younger animals, indicates that adenosinergic modulation of medullary respiration-related neurons changes during the first days of postnatal life.
Similar content being viewed by others
Main
Adenosine has a number of physiologic effects [for reviews, see Berne(1) and Collis and Hourani(2)], including depression of respiration in fetal(3, 4), newborn(5, 6), and adult(7, 8) mammals. Adenosine is a constituent of ATP and is mainly formed by dephosphorylation of AMP. The breakdown of ATP during hypoxia (i.e. decrease in Po2) and the concomitant increase in adenosine levels in the brain(9) may contribute to the irregular breathing or apnea that is often seen both in preterm human infants and in preterm animal models(10, 11).
In the human neonate, apnea can be triggered by hypoxia(12, 13), whereas the adenosine antagonist 1,3,-dimethylxanthine (theophylline) blocks hypoxia-induced depression of breathing in rats(14), rabbits(6), and piglets(15, 16). Thus, the therapeutic effect of theophylline on neonatal apnea has been suggested to be due to its antagonistic action on adenosine receptors(17–19).
However, little is yet known about the site(s) at which adenosinergic inhibition of breathing occurs. Adenosine has been shown to inhibit excitatory postsynaptic currents in hippocampal neurons(20) and to decrease neurotransmitter release in prejunctional motoneurons(21). In addition to its inhibitory effect on central neurons, adenosine also decreases body temperature and oxygen consumption, which could indirectly decrease respiration(22). Thus, the extent to which adenosine influences breathing by decreasing body metabolism or by a direct action on central respiratory control mechanisms is not yet clear.
The involvement of adenosine in the depression of inspiratory depth, via modulation of synaptic transmission at the spinal level to phrenic motoneurons, has recently been demonstrated(23). However, the possible effects of adenosine on the RR in the neonate has not been determined. Nor has the possibility that the age dependency of the effects of adenosine on respiration, demonstrated in vivo(5), influences the central respiratory control mechanisms been examined.
In the present study we have characterized the effects of adenosine on central respiratory pattern generation. Subsequently, we examined the possible effects of adenosine on C4/C5 RR, inspiratory time and amplitude, and the firing rate of medullary neurons, as well as the possible dependency of these effects on the postnatal age.
To study the effects of adenosine on central respiratory control mechanisms during the neonatal period, we have used an in vitro neonatal rat brainstem-spinal cord preparation from newborn to 4-d-old pups. This preparation retains the functional circuits required for generating a complex, coordinated respiratory motor output of brainstem origin, resembling the respiratory pattern of vagotomized rats in vivo(24, 25). The brainstem-spinal cord preparation thus contains the neurons critical for rhythm generation and integration of respiratory drive, which have been demonstrated in vitro to be located in the rostral ventrolateral medulla(26), that also seems to contain vital respiratory neurons in vivo(27). Inspiratory neurons, which appear to be fundamental components of the inspiratory pattern generation, are found near the nucleus ambiguus, in a region corresponding to the rostral ventrolateral medulla in this brainstem-spinal cord preparation(28). We have thus focused our investigation of respiratory pattern modulation by adenosine on these neurons.
METHODS
Brainstem-spinal cord preparation. The experiments were performed on newborn (0-4-d-old) Sprague-Dawley rats (n = 62). The brainstem and spinal cord were dissected under deep ether anesthesia and isolated as described previously(24, 29). In short, the brainstem was rostrally decerebrated between the VIth cranial nerve roots and the lower border of the trapezoid body.
The preparation was then transferred to a 2-mL chamber and continuously perfused at a rate of 3.0-3.5 mL/min with the following standard solution(mM): NaCl 124; KCl 5.0; KH2PO4 1.2; CaCl2 2.4; MgSO4 1.3; NaHCO3 26; glucose 30; and equilibrated with 95% O2 and 5% CO2 to pH 7.4 at 27.5 °C. The pH (membrane pH-m, HI 8314, Hanna Instruments, Leighton Buzzard, Bedfordshire, UK) and the temperature of the bathing solution were continuously monitored. Temperature was measured either directly in the bath (Quartz Digi-Thermo) or indirectly in the water-heating bath (Julabo UC, Julabo 5B), after calibration by direct measurement.
Recordings. Discharges of spinal motoneurons were recorded with suction electrodes applied to the proximal ends of cut C4 or C5 ventral root containing respiratory motoneuron axons (Fig. 1). This C4/C5 activity corresponds to phrenic nerve discharges(24, 25). The C4/C5 activity was amplified, rectified, and further processed (integrated) by a third order (Paynter) R-C filter (time constant 100 ms), to obtain signals approximating a moving average of the recorded activity (Int. C4).
The brainstem-spinal cord preparation. Schematic diagram of the neonatal rat brainstem-spinal cord preparation ventral surface. Respiration-related neurons were recorded extracellularly using a glass microelectrode. Respiratory motoneuron activity corresponding to inspiration was recorded from the C4/C5 ventral root through a glass suction electrode. Recordings to the right show spontaneous discharges from a Inspiratory neuron(top), C4 and the integrated C4 (bottom).Ttot = respiratory burst cycle, fi = intraburst firing frequency of I neuron, Ti = inspiratory time, I = duration of I neuron bursting, AICA = anterior inferior cerebellar artery, and XII = n. hypoglossus.
Extracellular recordings of the unit activity of respiration-related neurons in the ventrolateral medulla were performed using a glass microelectrode filled with 2% Pontamine sky blue in 0.5 M sodium acetate(resistance 2-8 megohms). The electrode was inserted through the ventral surface into the left or right rostral ventrolateral medulla using a micromanipulator (MW-4, Narishige, Tokyo). Respiration-related neurons were found 50-600 μm from the ventral surface(28) and identified by their characteristic firing pattern and correlation in time to the respiratory cycle of C4/C5 activity. Neuronal units that discharged only during the inspiratory phase (I neurons) were included in this study. Signals were amplified and band pass-filtered (10 Hz to 5 kHz, differential AC amplifier model 1700, A-M Systems, Everett, WA).
The C4/C5 and I neuronal activities were monitored via an analogue-digital converter (Digidata 1200, Axon Instruments, Foster City, CA) and data acquisition software (Axotape, Axon Instruments). Data were sampled (0.3-3 kHz) and stored for 1-4-min intervals every 10 min on a computer for off-line analysis. Continuous recordings of signals were performed with a strip chart recorder (ABB SE 120).
Drugs and chemicals. Adenosine is rapidly metabolized and transported from the extracellular space(30). We therefore used the metabolically stable adenosine A1 receptor agonist R-PIA to examine the effects of adenosine on respiratory activity. A solution of R-PIA (RBI, Natick, MA) was made by dissolving 4.0 mg in 0.10 mL of DMSO and 3.90 mL of standard solution to give a stock solution of 1000 μg/mL. This solution was further diluted in standard solution to yield final concentrations of 0.1, 1.0, and 10.0 μM.
Dipyridamole, a nucleoside transport inhibitor, was used in some preparations to increase the endogenous adenosine levels. Dipyridamole (RBI, Natick, MA) was prepared in the same way as R-PIA to give a concentration of 50 μM. The final concentration of DMSO in the solutions was less than 0.01%.
Theophylline, the clinically used adenosine receptor antagonist, with an A1/A2 receptor selectivity of 3:1(31), and the highly specific A1 receptor antagonist DPCPX were also used to establish the type of adenosine receptors involved. Theophylline (Sigma Chemical Co., Sweden) was used in a concentration of 10-20 mg/L (55-110μM). A 1 mM stock solution of DPCPX (Sigma) in ethanol was diluted in standard solution to a final concentration of 200 nM. In control experiments, corresponding amounts of DMSO or ethanol added alone to the standard solution did not change the respiratory activity. Drugs were added to the standard solution superfusing the preparation after an initial control period of 100± 6 min.
Data analysis. The inspiratory time (Ti) was defined as the interval during which a continuos discharge occurred in the ventral root. The respiratory cycle duration in seconds(Ttot), defined as the time between two consecutive bursts of Int. C4, was used to calculate the RR in respiratory bursts per min (Fig. 1). As an index of the regularity of the respiratory pattern, the CV, i.e. the ratio of the SD and the mean cycle duration, was calculated.
The Int. C4 was analyzed with regard to change in amplitude. In some experiments (n = 20), the mean fi of I neurons was calculated from the average number of spikes in 10 consecutive bursts (Fig. 1). The medullary respiration-related neuronal response and the C4 motoneuronal burst activity were analyzed under control conditions, during drug application; after 21 + 0.5 min of perfusion with R-PIA or theophylline or 26 ± 0.5 min of perfusion with dipyridamole; and after recovery with the standard solution.
The mean and SEM were calculated for all data, and the results are listed as an average percentage of the control values ± SEM (% ± SEM).
Statistical significance was assessed using two-way analysis of the variance, repeated measures design to compare the activity before, during, and after drug application. The difference between two means was analyzed using t test after the F test was performed. The difference between several independent means was analyzed by comparing all pairs using the Tukey-Kramer HSD test. A value of p < 0.05 was considered to be statistically significant.
RESULTS
Control respiratory activity during development. A representative recording from an inspiratory neuron and the concomitant C4 activity of a 1-d-old rat are shown in Figure 2A. The spontaneous activity of the inspiratory-related neurons in the rostral ventrolateral medulla and the respiratory bursts recorded from C4/C5 remained stable for more than 4 h under control conditions. In preparations from pups with postnatal age >2 h, the control RR was 9.15 + 0.3 bursts/min with regular C4/C5 respiratory rhythm, the CV being 0.18 ± 0.02 and the Ti 784 ± 35 ms (n = 56). Control respiratory parameters in the preparations from different age groups are presented in Table 1 and Figure 3C. A more irregular breathing pattern (CV = 0.37 ± 0.08) was seen in all(n = 5) the preparations from newborn pups (0-2 h old)(Fig. 3, A and C). This pattern was characterized by respiratory bursts appearing in clusters of two or even three with short periods (e.g. <500 ms) between bursts. This aberrant pattern was not modified to a more regular one, even after sectioning the medulla more caudallly (n = 3), in an attempt to exclude possible remaining pontine inhibition(25). These three (0-2 h) preparations were not included in the analysis of drug effects.
Effects of adenosine agonist. The effects of R-PIA and theophylline on inspiratory neurons (I neuron, upper traces), C4 activity (middle traces), and integrated C4 activity (lower traces) are shown. (A) The respiratory activities recorded with a preparation from a 1-d-old rat in standard solution. (B) As in(A), except after 21 min of perfusion with 1 μM R-PIA.(C) Washout 20 min after the R-PIA perfusion. (D) After 20 min of perfusion with 1 μM R-PIA and 55 μM theophylline.
The postnatal respiratory pattern. In the preparations made from pups within 2 h after birth, a pattern with respiratory bursts appearing in clusters was present. (A) Control respiratory C4 activity (C4) and Int. C4 of a preparation from a pup killed and dissected immediately after birth. (B) As in (A), except after 22 min of perfusion with 50 μM dipyridamole. (C) The regularity of the C4/C5 burst rhythm in relation to postnatal age. The CV of RR was significantly correlated to postnatal age (age vs CV; Spearman rank correlation p = 0.01) (P = postnatal age in days).
A similar irregular respiratory pattern (CV = 0.49 ± 0.09), significantly different from the normal control, was seen in 3 out of 12 preparations from the slightly older pups (2-24 h), but only in one (27 h; CV= 0.56) of 45 preparations from pups older than 24 h. In total, nine preparations demonstrated irregular RR. Of these, three were excluded from analysis of drug effect, after the caudal sectioning of the medulla, mentioned above, had been performed. The remaining six preparations with irregular control respiratory patterns did not show any significant differences in drug effects compared with the preparations with more regular respiratory activity.
Preliminary analysis by Spearman rank correlation revealed a significant age dependency with respect to the effects of R-PIA and dipyridamole (see Fig. 5A) When the data from the preparations were divided into groups with postnatal ages of 0-2 h, 3-24 h, 25-47 h (P1), 48-72 h (P2) and >72 h (P3), the RR was significantly higher in the youngest group of pups (0-2 h). The Ti was not significantly different between groups (Table 1), but the regularity of the respiratory pattern (CV) differed significantly between the youngest (0-2 h) group and the P2 and P3 groups (Fig. 3C).
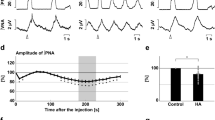
Age dependency of adenosinergic effects on respiration.(A) Scattergram of postnatal age plotted in relationship to the reduction of RR by 0.1 or 1.0 μM R-PIA and 50 μM dipyridamole.(B) Relationship between postnatal age and the inhibition of RR by R-PIA 0.1 (<48 h, n = 6, ≥48 h, n = 5) or 1.0 μM(n = 6 and 7, respectively) or 50 μM dipyridamole (n = 5 and 8, respectively). The effects of the adenosine agonist and the nucleoside transport inhibitor dipyridamole were correlated to postnatal age, with a more pronounced effect in the younger animals. (C) Theophylline, 55 μM (n = 5 and 9, respectively), increased the RR compared with control and could reverse the depression of respiratory activity if applied together with 1 μM R-PIA (R-PIA +Theophylline) (n = 5 and 5, respectively). Error bars are SEM (*p < 0.05).
Because it was only in preparations from younger (<48 h) pups that adenosinergic drugs could elicit an irregular breathing pattern and because the RR and Ti did not differ significantly (except in two(0-2 h) preparations), we divided the pups into two age groups. For analysis we thus compared the data both altogether and divided into two groups,i.e. preparations from pups with a postnatal age of 1) less than 48 h (<48 h, n = 27) and 2) of more than 48 h(≥48 h, n = 35) (Table 2).
Adenosine receptor agonist decreases RR. A representative recording of the respiratory activity after administration of R-PIA is shown in Figure 2B. In all preparations, the respiratory activity was depressed during administration of 1 μM R-PIA (n = 13), mainly due to a reduction of the RR (-23 ± 4%, p < 0.01). Neither Ti (-14 ± 12%) nor the mean C4/C5 burst amplitude (-5 ± 6%) was significantly altered, although in 2 of 13 individual preparations a significant decrease in amplitude was observed. At a 10-fold lower concentration, i.e. 0.1 μM (n = 11), R-PIA also decreased the RR (-12.9 ± 0.7%, p < 0.05). The Ti (3 ± 12%) and the C4/C5 burst amplitude (-0.8± 2%) did not change significantly (Fig. 4B).
Irregular respiration induced by an adenosine agonist. In preparations from rats younger than 48 h, the effects on the RR were pronounced, and a reversible irregular RR could be induced. (A) The respiratory activity recorded with a preparation from a 20-h-old rat in standard solution. (B) As in (A), after 22 min of perfusion with 0.1 μM R-PIA. (C) As in (B), after 22 min of perfusion with 1 μM R-PIA. (D) As in (C), after 22 min of recovery with standard solution. C4, respiratory activity.
A block of adenosine uptake decreases C4/C5 respiratory activity. Upon application of the adenosine uptake blocker dipyridamole (50μM; n = 13), the respiratory activity decreased in a manner similar to that seen with R-PIA (RR -26 ± 4.2%, p < 0.01;Ti -10 ± 6.5%) as shown in Figure 3B. The C4/C5 burst amplitude did not change significantly when the data were pooled, but decreased significantly in three and increased significantly in one preparation.
Endogenous adenosine decreases C4/C5 respiratory activity. Theophylline (55 μM; n = 14) increased the RR (13 ± 2.1%) compared with controls (p < 0.01), whereas no significant change was observed in Ti (0.4 ± 3.8%). A significant increase in the C4/C5 burst amplitude was observed in two of the preparations, but in most cases (12/14) no significant increase was seen. DPCPX (50 μM;n = 5) had a similar effect, RR increased; 13.4 ± 1.8%,p < 0.01 and Ti did not change; 1.5 ± 8.4. None of the preparations had significant changes in the Int. C4/C5 amplitude. No significant difference between the effects of theophylline and DPCPX application was found (unpaired t test).
The effects of R-PIA and that of dipyridamole on fi, RR, CV, Ti, and amplitude could all be reversed or prevented by administration of theophylline or DPCPX. When 1 μM R-PIA was applied together with 55 μM theophylline (n = 10), no significant changes in RR (-2.8 ± 2.1%), CV (-3.6 ± 12.6%), amplitude (+4.7 ± 3.9%), or Ti (-7.2 ± 7.6%) were observed compared with the control (Figs. 2D and 5B).
An adenosine receptor agonist and uptake blocker decrease activity of I neurons (fi). Application of 1 μM R-PIA significantly decreased fi in 9 out of 10 I neurons examined (Table 3). When dipyridamole was applied, the fi decreased significantly in all three of the I neurons examined; 17.7 ± 1.6 spikes/s during control conditions and 6.9± 1 spikes/s (p < 0.01) during dipyridamole perfusion.
Theophylline increased the fi in all four of the I neurons examined, although this effect was statistically significant only in two individual experiments. For the total data this value was 16.1 ± 1.0 spikes/s under control conditions to 18.4 ± 1.5 spikes/s during theophylline perfusion. The effects of R-PIA on fi could be reversed by administration of theophylline together with R-PIA(Table 3).
DPCPX increased the fi in all three of the I neurons examined. The control value was in this case 14.5 ± 1.7 spikes/s compared with 18.7 ± 3.4 spikes/s during exposure to DPCPX.
No differences, at any given age, in control, drug, or post-drug C4/C5 respiratory parameters were detected between preparations in which I neuronal activity was recorded and preparations in which only C4/C5 activity was recorded. We therefore consider the I neuronal recordings to be representative for the whole population of animals.
Age-dependent effects of adenosine receptor agonist and uptake blocker on respiratory activity. As shown in Figure 5, R-PIA had a significantly more pronounced effect on RR in preparations from younger pups (<48 h) compared with those from older pups (≥48 h). This age-dependent difference in the effect on RR was significant with both 0.1 and 1.0 μM R-PIA (RR change; Spearman rank correlation; p = 0.003,n = 11 and p = 0.025, n = 12, respectively). The change in fi caused by 1.0 μM R-PIA also tended to be age-dependent, although this trend was not statistically significant (age versus fi change; Spearman rank correlation; p = 0.1 n = 10). When the two age groups <48 h and ≥48 h were compared, no significant age dependency was seen with regard to fi change (Table 3). Neither Ti nor the C4/C5 burst amplitude demonstrated any significant dependency on age. Like R-PIA, dipyridamole had a more pronounced effect on preparations from the youngest rats (RR change; age versus drug Spearman rank correlation; p = 0.02, n = 13)(Fig. 5). The effects of theophylline and DPCPX on RR,Ti, and fi showed no dependency on age.
Age-dependent effects of adenosine receptor agonist and antagonists on the regularity of respiratory rhythm. The effect of R-PIA on the change of CV was found to depend significantly on age when all preparations were compared (CV control/CV drug; Spearman rank correlation;p = 0.004, n = 24). When comparing the age groups <48 h(0.55 ± 0.24, n = 12) with ≥48 h (1.21 ± 0.24,n = 12) no significant difference could be shown (p = 0.06, unpaired t test). Most (9/12) of the preparations from the younger pups (2-48 h) responded with a significantly more irregular breathing pattern when R-PIA was applied. In 6 of these 12 preparations, a respiratory pattern with clustered respiratory bursts, similar to the respiratory pattern of the youngest pups (CV 0.50 + 0.07), appeared (Fig. 4, A-C). In preparations from pups older than 48 h, R-PIA induced a significant increase in CV in 3/12 preparations compared with control, but in total there was no significant effect on CV. In this age group a respiratory pattern with clustered respiratory bursts could be evoked in only one preparation, and even in this case, a higher (10 μM) concentration of R-PIA was required to obtain this effect. When comparing the number of experiments in which R-PIA could induce a increase in CV, a significant difference between the two age groups (<48 h/≥48 h) was found (two-tail Fischer's exact test, p = 0.04).
With DPCPX the same tendency for age dependency was observed; <48 h (CV control/CV DPCPX 2.72 ± 1.27 n = 3) ≥48 h (CV control/CV DPCPX 0.67 ± 0.31 n = 2). However, the number of DPCPX experiments were not sufficient to make conclusions regarding DPCPX-induced changes of CV and age dependency. The effect of theophylline on the change of CV was, as with that of R-PIA, found to depend significantly on age when all preparations were compared (CV control/CV theophylline; Spearman rank correlation; p = 0.04, n = 13). When comparing the age groups <48 h (CV control/CV theophylline; 1.32 ± 0.18, n = 5) and ≥48 h (CV control/CV theophylline; 0.76 ± 0.15, n = 8) theophylline increased the regularity of RR compared with control in the young group significantly more than in the older age group (t test independent means, p = 0.04, n = 13).
DISCUSSION
We have found that the adenosine A1 receptor agonist R-PIA and the adenosine uptake blocker dipyridamole depress respiratory neuronal activity in the ventrolateral structures of the rostral medulla, as well as decreasing the frequency of respiratory bursts in brainstem-spinal cord preparations from the neonatal rat. This depression was reversed by theophylline and the specific A1 receptor antagonist DPCPX. Furthermore, we found that the reduction in RR by R-PIA and dipyridamole is inversely correlated to postnatal age.
Adenosine has a direct central depressive effect on RR. It has previously been suggested that adenosine decreases breathing by lowering body temperature and thus reducing the oxygen demand(22). Instead, our results corroborate with earlier findings in in vivo models of adult cat and rat, suggesting that both adenosine and xanthine derivatives have direct effects on the respiratory neural network in the brainstem(32, 33). Furthermore, our results indicate that adenosine decreases inspiratory neuronal activity and respiratory output by the activation of A1 receptors in the neonatal rat. This is in accordance with findings in adult cats demonstrating modulation of expiratory neurons and synaptic transmission by adenosine(34). Our present in vitro findings clearly demonstrate that adenosine inhibits respiration, not only via an indirect effect on body temperature and metabolism, but also by direct action on the functional network of respiratory neurons within the medulla oblongata.
Endogenous adenosine depresses respiration. The finding that the nucleoside uptake blocker, dipyridamole, inhibited respiratory activity in a manner similar to that of the A1 receptor agonist R-PIA suggests that endogenous adenosine has a modulatory effect on central respiratory control mechanisms.
This is further supported by the consistent increase in respiratory output by the receptor antagonists theophylline and DPCPX. Taken together, these findings imply that in this in vitro preparation, as is the case in vivo(34), respiration is modulated by the endogenous activation of adenosine receptors under control conditions.
Adenosine A1 receptors mediate the adenosinergic respiratory depression. The findings of responses to the unspecific theophylline and dipyridamole similar to the responses to specific A1 antagonist/agonists support the conclusion that the A1 receptor contributes significantly to the observed modulation of respiratory activity. However, we cannot exclude the possibility that adenosine A2 receptors may be involved in the observed responses to dipyridamole or theophylline.
Adenosine A1 receptors reduce presynaptic Ca2+ influx(35), which subsequently inhibits the release of excitatory transmitters(36), such as glutamate(37). Furthermore, postsynaptic A1 receptors can hyperpolarize the neuron by activating potassium channels(38). Such pre- and postsynaptic inhibition of neuronal activity could explain the observed depression of respiratory activity. One might speculate that this pre- and postsynaptic inhibition of neuronal activity and an ensuing decrease in activation of the voltage-dependent NMDA channel could explain the irregular breathing induced by the adenosine agonist in vitro. This is in agreement with the finding that blocking the glutaminergic NMDA receptor can induce irregular or apneustic breathing patterns in vivo(39, 40).
Earlier studies have shown that presynaptic A1 receptors modulate synaptic transmission to phrenic motoneurons(23). Furthermore, theophylline can attenuate both the hypoxic depression of respiration in vivo(5, 19) and the depression of C4 motoneuronal discharge in vitro(41). Adenosine could be a link between cellular energy metabolism(42) and the excitability of neurons, because breakdown of ATP increases substantially during hypoxia and more adenosine is formed. Therefore, the actions of adenosine on respiration-related neurons in the brainstem shown here, together with the observations on spinal motoneurons might explain, part of the respiratory decrease induced by hypoxia(43, 44).
Theophylline in high concentrations can increase cAMP levels by inhibiting phosphodiesterase and the excitatory effects of theophylline on respiration might thus be explained by such a rise in cAMP concentration. However, higher concentrations of theophylline than the ones used in the present study are required to affect phosphodiesterase in vitro(45). Furthermore, it has previously been reported that forskolin, which increases cAMP levels, has no effect on the RR in the brainstem-spinal cord preparation when the control RR is >5 bursts/min(46). We therefore suggest that the responses to theophylline observed in our study, can be attributed primarily to a blockade of other A1 receptor-mediated effects, rather than to a decrease in cAMP.
Age and the effect of adenosine on respiration. The effects of both R-PIA and dipyridamole on RR were found to be significantly different between the two postnatal age groups, i.e. 0-48 h and ≥48 h (Fig. 5). Furthermore, both the agonist of the adenosine A1 receptor and the blocker of adenosine uptake could induce reversible irregular breathing patterns in preparations from the yonger rat pups (Fig. 4).
The irregularity of RR increases with adenosine receptor agonists and uptake blocker in inverse relation to postnatal age. Furthermore, the irregularity of RR decreases with antagonists in inverse relation to postnatal age. These data indicates that adenosine is one of the factors contributing to the irregular respiratory pattern observed.
The instability of breathing in the newborn period has been attributed to the development of neuronal networks(47). It seems likely that such an immature neuronal network could be more susceptible to the influences of an inhibitory modulator such as adenosine.
This correlation between postnatal age and drug effects has not been described previously with this in vitro preparation. We therefore stress the importance of taking age into account when interpreting data from this neonatal preparation. Our results are in agreement with earlier findings in neonatal rabbits(5) and piglets(48), where a considerably more pronounced effect of adenosine agonists on respiration was found in newborn (1-3 d) compared with older animals (8 d and 3 wk). Thus, an increased sensitivity to adenosinergic agents in the neonatal rat immediately after birth could explain our observations.
The effects of theophylline on respiratory activities were not, however, found to be age-dependent, indicating that adenosinergic modulation under control conditions is the same in the newborn as in the 2-4-d-old pups. We are not able to explain this finding at present.
Irregular breathing can be induced in human infants by hypoxia(12) and reversed by theophylline, suggesting that adenosine released as a result of the hypoxia is involved. In the present study the effects of both the adenosine agonist R-PIA and dipyridamole could be reversed by theophylline, which is used in neonatal practice to treat apnea and irregular breathing. The present data supports the suggestion that the therapeutic effect of theophylline on recurrent neonatal apnea is due to its antagonism of central adenosine receptors(49).
Medullary respiratory neurons are responsible for respiratory central pattern generation(50, 51). Central application of an adenosine agonist or an uptake blocker to the in vitro preparation, where no afferent feedback is preserved, causes depression of both medullary respiratory neuronal units and the RR.
Thus, our data suggest that, in addition to its role at the level of the spinal cord(23), the adenosinergic system is also active within the brainstem and is involved in the modulation of respiratory neurons and the RR. We thus suggest that the changes in 1) inspiratory neuronal activity, 2) C4/C5 respiratory burst rate, and 3) irregularity caused by adenosinergic agents observed here are mediated at the level of the medulla oblongata.
In conclusion, we have found that adenosine depresses the activity of inspiratory-related neurons in the neonatal rat medulla oblongata as well as decreasing the RR and the regularity of respiratory rhythm. The potency of this modulatory effect of adenosine on respiration decreases during the first days after birth. Furthermore, theophylline can block this respiratory depression, primarily by acting on adenosine A1 receptors in the medulla.
Abbreviations
- R-PIA:
-
N6-(2-phenylisopropyl)adenosine, R(-)isomer
- DPCPX:
-
8-cyclopentyl-1,3-dipropylxanthine
- RR:
-
respiratory rate (bursts/min)
- Int. C4:
-
integrated C4/C5 activity
- I neuron:
-
inspiratory neuronal unit
- f i :
-
intraburst firing frequency of I neuron (spikes/s)
- T i :
-
inspiratory time
- CV:
-
coefficient of variation
- NMDA:
-
N-methyl-D-aspartate
References
Berne RM 1986 Adenosine: an important physiological regulator. Trends Neurosci 1: 163–167.
Collis MG, Hourani SM 1993 Adenosine receptor subtypes. Trends Pharmacol Sci 14: 360–366.
Bissonette JM, Hohimer R, Chao CR, Knopp SJ, Notoroberto NF 1990 Theophylline stimulates fetal breathing movements during hypoxia. Pediatr Res 28: 83–86.
Koos BJ, Matsuda K 1990 Fetal breathing, sleep state, and cardiovascular responses to adenosine in sheep. J Appl Physiol 68: 489–495.
Runold M, Lagercrantz H, Fredholm BB 1986 Ventilatory effect of an adenosine analogue in unanesthetized rabbits during development. J April Physiol 61: 255–259.
Runold M, Lagercrantz H, Prabhakar NR, Fredholm BB 1989 Role of adenosine in hypoxic ventilatory depression. J Appl Physiol 67: 541–546.
Eldridge FL, Milhorn DE, Kiley JP 1984 Respiratory effects of a long-acting analog of adenosine. Brain Res 301: 273–280.
Yamamoto M, Nishimura M, Kobayashi S, Akiyama Y, Miyamoto K, Kawakami Y 1994 Role of endogenous adenosine in hypoxic ventilatory response in humans: a study with dipyridamole. J Appl Physiol 76: 196–203.
Winn HR, Rubio R, Berne RM 1981 Brain adenosine concentration during hypoxia in rats. Am J Physiol 241: 235–242.
Hedner T, Hedner J, Jonason J, Wessberg P 1984 Effects of theophylline on adenosine-induced respiratory depression in the preterm rabbit. Eur J Respir Dis 65: 153–156.
Lagercrantz H 1992 What does the preterm infant breathe for? Controversies on apnea of prematurity. Acta Paediatr 81: 733–736.
Rigatto H, Brady JP, Chir B 1972 Periodic breathing and apnea in preterm infants. II. Hypoxia as a primary event. Pediatrics 50: 219–28.
Miller MJ, Martin RJ 1992 Pathophysiology of apnea of prematurity. In: Polin, RF (ed) Fetal and Neonatal Physiology. WB Saunders, Philadelphia, pp 872–885.
Neylon M, Marshall JM 1991 The role of adenosine in the respiratory and cardiovascular response to systemic hypoxia in the rat. J Physiol 440: 529–545.
Moss IR, Runold M, Dahlin I, Fredholm BB, Nyberg F, Lagercrantz H 1987 Respiratory and neuroendocrine responses of piglets to hypoxia during postnatal development. Acta Physiol Scandinav 131: 533–541.
Lopes JM, Davis GM, Mullahoo K, Aranda JV 1994 Role of adenosine in the hypoxic ventilatory response of the newborn piglet. Pediatr Pulmonol 17: 50–55.
Lagercrantz H, Yamamoto Y, Fredholm BB, Prabhakar NR, Euler C 1984 Adenosine analogues depress ventilation in rabbit neonates. Pediatr Res 18: 387–390.
Hedner J, Hedner T, Wessberg P, Jonason J, Mueller RA 1985 Central respiratory effects of adenosine analogues, theophylline and enprofylline. In: Andersson, KE, Persson CGA (eds) Anti-Asthma Xanthines and Adenosine. Excerpta Medica, Copenhagen, pp 467–471.
Darnall RJ 1985 Aminophylline reduces hypoxic ventilatory depression: possible role of adenosine. Pediatr Res 19: 706–710.
Katchman AN, Hershkowitz N 1993 Adenosine antagonists prevent hypoxia-induced depression of excitatory but not inhibitory synaptic currents. Neurosci Lett 159: 123–126.
Mynlieff M, Beam KG 1994 Adenosine acting at an A1 receptor decreases N-type calcium current in mouse motoneurons. J Neurosci 14: 3628–3634.
Lagercrantz H, Runold M, Yamamoto Y, Fredholm BB 1986 Adenosine: a putative mediator of the hypoxic ventilatory response of the neonate. In: Euler H, Lagercrantz H (eds) Neurobiology of the Control of Breathing. Raven Press, New York, pp 133–139.
Dong XW, Feldman JL 1995 Modulation of inspiratory drive to phrenic motoneurons by presynaptic adenosine A1 receptors. J Neurosci 15: 3458–3467.
Suzue T 1984 Respiratory rhythm generation in the in vitro brainstem-spinal cord preparation of the neonatal rat. J Physiol 354: 173–183.
Smith JC, Greer JJ, Liu GS, Feldman JL 1990 Neural mechanisms generating respiratory pattern in mammalian brain stem-spinal cord in vitro. I. Spatiotemporal patterns of motor and medullary neuron activity. J Neurophysiol 64: 1149–1169.
Smith JC, Ellenberger HH, Ballanyi K, Richter DW, Feldman JL 1991 Pre-Bötzinger complex: a brainstem region that may generate respiratory rhythm in mammals. Science 254: 726–729.
Schwarzacher SW, Smith JC, Richter DW 1995 Pre-Bötzinger complex in the cat. J Neurophysiol 73: 1452–1461.
Arata A, Onimaru H, Homma I 1990 Respiration-related neurons in the ventral medulla of newborn rats in vitro. Brain Res Bull 24: 599–604.
Yamamoto Y, Onimaru H, Homma I 1992 Effect of substance P on respiratory rhythm and pre-inspiratory neurons in the ventrolateral structure of rostral medulla oblongata: an in vitro study. Brain Res 599: 272–276.
Möser GH, Schrader J, Deussen A 1989 Turnover of adenosine in plasma of human and dog blood. Am J Physiol 256: 799–806.
Stone T 1991 Adenosine in the Nervous System. Academic Press, London
Eldridge FL, Millhorn DE, Kiley JP 1985 Antagonism by theophylline of respiratory inhibition induced by adenosine. J Appl Physiol 59: 1428–1433.
Thomas T, Elnazir BK, Marshall JM 1994 Differentiation of the peripherally mediated from the centrally mediated influences of adenosine in the rat during systemic hypoxia. Exp Physiol 79: 809–822.
Schmidt C, Bellingham MC, Richter DW 1995 Adenosinergic modulation of respiratory neurones and hypoxic responses in the anaesthetized cat. J Physiol 483: 769–781.
Fredholm BB, Dunwiddie TV 1988 How does adenosine inhibit transmitter release? Pharmacol Sci 9: 130–134.
Fredholm BB, Dunér-Engström M, Fastbom J, Jonzen B, Lindgren E, Nordstedt C, Pedata F, van der Ploeg I 1987 Interactions between the neuromodulator adenosine and the classic transmitters. In: Gerlach E, Becker BF (eds) Topics and Perspectives in Adenosine Research. Springer-Verlag, Berlin, pp 509–520.
Héron A, Lekieffre D, Le Peillet E, Lasbennes F, Seylaz J, Plotkine M, Boulu RG 1994 Effects of an A1 adenosine receptor agonist on the neurochemical, behavioral and histological consequences of ischemia. Brain Res 641: 217–224.
Trussel LO, Jackson MB 1987 Dependence of an adenosine-activated potassium current on a GTP-binding protein in mammalian central neurons. J Neurosci 7: 3306–3316.
Feldman JL, Windhorst U, Anders K, Richter DW 1992 Synaptic interaction between medullary respiratory neurones during apneusis induced by NMDA-receptor blockade in cat. J Physiol 450: 303–323.
Connelly CA, Otto SM, Feldman JL 1992 Blockade of NMDA receptor-channels by MK-801 alters breathing in adult rats. Brain Res 596: 99–110.
Kawai A, Okada Y, Mückenhoff K, Scheid P 1995 Theophylline and hypoxic ventilatory response in the rat isolated brainstem-spinal cord. Respir Physiol 100: 25–32.
Lloyd HG, Lindström K, Fredholm BB 1993 Intracellular formation and release of adenosine from rat hippocampal slices evoked by electrical stimulation or energy depletion. Neurochem Int 23: 173–185.
Cross K, Warner P 1951 The effect of inhalation of high and low oxygen concentration on the respiration of the newborn infant. J Physiol 114: 283–295.
Haddad GG, Mellins RB 1984 Hypoxia and respiratory control in early life. Annu Rev Physiol 46: 629–643.
Bergstrand H 1985 Xanthines as phosphodiesterase inhibitors. In K.-E. Andersson, K-E, Persson CGA (eds) Anti-Asthma Xanthines and Adenosine. Excerpta Medica, Copenhagen, pp 16–22.
Arata A, Onimaru H, Homma I 1993 Effects of cAMP on respiratory rhythm generation in brainstem-spinal cord preparation from newborn rat. Brain Res 605: 193–199.
Bryan AC, Bryan MH 1978 Control of respiration in the newborn. Clin Perinatol 5: 269–281.
Elnazir B, Marshall JM, Kumar P 1996 Postnatal development of the pattern of respiratory and cardiovascular response to systemic hypoxia in the piglet: the roles of adenosine. J Physiol 492: 573–585.
Hedner T, Hedner J, Bergman B, Mueller RA, Jonason J 1985 Characterization of adenosine-induced respiratory depression in the preterm rabbit. Biol Neonate 47: 323–332.
von Euler C 1991 Neuronal organization and rhythm generation. In: Crystal RG, West JB (eds) The Lung. Raven Press, New York, pp 1–12.
Bianchi AL, Denavit-Saubié M, Champagnat J 1995 Central control of breathing in mammals: neuronal circuitry, membrane properties, and neurotransmitters. Physiol Rev 75: 1–45.
Author information
Authors and Affiliations
Additional information
Supported by the Swedish Medical Research Council (SMFR 14X-0907 and 19X-5234), The Fraenkel and Laerdal Fund, and Wera-Ekströms Fund for Pediatric Research.
Rights and permissions
About this article
Cite this article
Herlenius, E., Lagercrantz, H. & Yamamoto, Y. Adenosine Modulates Inspiratory Neurons and the Respiratory Pattern in the Brainstem of Neonatal Rats. Pediatr Res 42, 46–53 (1997). https://doi.org/10.1203/00006450-199707000-00008
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199707000-00008
This article is cited by
-
Purinergic signalling during development and ageing
Purinergic Signalling (2015)
-
Rhythm generation by the pre-Bötzinger Complex in medullary slice and island preparations: Effects of adenosine A1receptor activation
BMC Neuroscience (2008)