Abstract
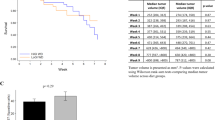
Epidemiological studies suggest a positive association between nutrient intake, hyperinsulinemia and risk of Benign prostatic hyperplasis (BPH). This study tests the hypothesis that a low-fat, high-fiber diet and daily exercise would lower serum insulin and reduce the growth of serum-stimulated primary prostate epithelial cells in culture. Serum samples were obtained from eight overweight men before and after the Pritikin residential, 2-week diet and exercise intervention and from seven men who were long-term followers of the low-fat, high-fiber diet and regular exercise lifestyle. The serum was used to stimulate primary prostate epithelial cells in culture. Growth was measured after 48 and 96 h and apoptosis after 96 h. At 48 h there was no significant difference in growth within the Pre, 2-week or Long-Term groups. At 96 h growth was significantly reduced in the 2-week (13%) and in the Long-Term (14%) groups compared to the Pre data. At 96 h, apoptosis was not significantly different among the three groups. Fasting insulin was reduced by 30% in the 2-week group and by 52% in the Long-Term group compared to the Pre data. Testosterone was unchanged in the 2-week group. The results of this study indicate that a low-fat, high-fiber diet and daily exercise lowers insulin and reduces growth of prostate primary epithelial cells and suggests that lifestyle may be an important factor in the development or progression of BPH. Future prospective trials should address the effects of this lifestyle modification on BPH symptomatology and progression.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Blom JH, Schroder FH . Epidemiology and natural course of benign prostatic hyperplasia. Urologe A 1992; 31: 129–134.
Phipps S, Yang TH, Habib FK, Reuben RL, McNeill SA . Measurement of tissue mechanical characteristics to distinguish between benign and malignant prostatic disease. Urology 2005; 66: 447–450.
Konig JE, Senge T, Allhoff EP, König W . Analysis of the inflammatory network in benign prostate hyperplasia and prostate cancer. Prostate 2004; 58: 121–129.
Kramer G, Mitteregger D, Marberger M . Is benign prostatic hyperplasia (BPH) an immune inflammatory disease? Eur Urol 2007; 51: 1202–1216.
Sciarra A, Di Silverio F, Salciccia S, Autran Gomez AM, Gentilucci A, Gentile V . Inflammation and chronic prostatic diseases: evidence for a link? Eur Urol 2007; 52: 964–972.
Untergasser G, Madersbacher S, Berger P . Benign prostatic hyperplasia: age-related tissue-remodeling. Exp Gerontol 2005; 40: 121–128.
Bravi F, Bosetti C, Dal Maso L, Talamini R, Montella M, Negri E et al. Food groups and risk of benign prostatic hyperplasia. Urology 2006; 67: 73–79.
Suzuki S, Platz EA, Kawachi I, Willett WC, Giovannucci E . Intakes of energy and macronutrients and the risk of benign prostatic hyperplasia. Am J Clin Nutr 2002; 75: 689–697.
Rohrmann S, Giovannucci E, Willett WC, Platz EA . Fruit and vegetable consumption, intake of micronutrients, and benign prostatic hyperplasia in US men. Am J Clin Nutr 2007; 85: 523–529.
Hammarsten J, Hogstedt B, Holthuis N, Mellström D . Components of the metabolic syndrome-risk factors for the development of benign prostatic hyperplasia. Prostate Cancer Prostatic Dis 1998; 1: 157–162.
Barnard RJ, Aronson WJ, Tymchuk CN, Ngo TH . Prostate cancer: another aspect of the insulin-resistance syndrome? Obes Rev 2002; 3: 303–308.
Tymchuk CN, Barnard RJ, Heber D, Aronson WJ . Evidence of an inhibitory effect of diet and exercise on prostate cancer cell growth. J Urol 2001; 166: 1185–1189.
Ngo TH, Barnard RJ, Tymchuk CN, Cohen P, Aronson WJ . Effect of diet and exercise on serum insulin, IGF-I, and IGFBP-1 levels and growth of LNCaP cells in vitro (United States). Cancer Causes Control 2002; 13: 929–935.
Hammarsten J, Hogstedt B . Hyperinsulinaemia as a risk factor for developing benign prostatic hyperplasia. Eur Urol 2001; 39: 151–158.
Nandeesha H, Koner BC, Dorairajan LN, Sen SK . Hyperinsulinemia and dyslipidemia in non-diabetic benign prostatic hyperplasia. Clin Chim Acta 2006; 370: 89–93.
Dahle SE, Chokkalingam AP, Gao YT, Deng J, Stanczyk FZ, Hsing AW . Body size and serum levels of insulin and leptin in relation to the risk of benign prostatic hyperplasia. J Urol 2002; 168: 599–604.
Ozden C, Ozdal OL, Urgancioglu G, Koyuncu H, Gokkaya S, Memis A . The correlation between metabolic syndrome and prostatic growth in patients with benign prostatic hyperplasia. Eur Urol 2007; 51: 199–203.
Tymchuk CN, Barnard RJ, Ngo TH, Aronson WJ . The role of testosterone, estradiol, and insulin in diet and exercise-induced reductions in serum-stimulated prostate cancer cell growth in vitro. Nutr Cancer 2002; 42: 112–116.
Polychronakos CJU, Lehoux JG, Koutsilieris M . Mitogenic effects of insulin and insulin-like growth factors on PA0III rat prostate adenocarcinoma cells: characterization of the receptors involved. Prostate 1991; 19: 313–321.
Tymchuk CN, Tessler SB, Aronson WJ, Barnard RJ . Effects of diet and exercise on insulin, sex hormone-binding globulin, and prostate-specific antigen. Nutr Cancer 1998; 31: 127–131.
Ngo TH, Barnard RJ, Leung PS, Cohen P, Aronson WJ . Insulin-like growth factor I (IGF-I) and IGF binding protein-1 (IGFBP-1) modulates prostate cancer cell growth and apoptosis: a possible mediators for the effects of diet and exercise on cancer cell survival. Endocrinology 2003; 144: 2319–2324.
Plymate SR, Matej LA, Jones RE, Friedl KE . Inhibition of sex hormone-binding globulin production in the human hepatoma (Hep G2) cell line by insulin and prolactin. J Clin Endocrinol Metab 1988; 67: 460–464.
Barnard RJ, Aronson WJ . Preclinical models relevant to diet, exercise, and cancer risk. Recent Results Cancer Res 2005; 166: 47–61.
Yu H, Rohan T . Role of the insulin-like growth factor family in cancer development and progression. J Natl Cancer Inst 2000; 92: 1472–1489.
Cohen P, Peehl DM, Lamson G, Rosenfeld RG . Insulin-like growth factors (IGFs), IGF receptors, and IGF-binding proteins in primary cultures of prostate epithelial cells. J Clin Endocrinol Metab 1991; 73: 401–407.
Grant ES, Ross MB, Ballard S, Naylor A, Habib FK . The insulin-like growth factor type I receptor stimulates growth and suppresses apoptosis in prostatic stromal cells. J Clin Endocrinol Metab 1998; 83: 3252–3257.
Thomas JA, Keenan EJ . Effects of estrogens on the prostate. J Androl 1994; 15: 97–99.
Rosenthal MB, Barnard RJ, Rose DP, Inkeles S, Hall J, Pritikin N . Effects of a high-complex-carbohydrate, low-fat, low-cholesterol diet on levels of serum lipids and estradiol. Am J Med 1985; 78: 23–27.
Erbersdobler A, Augustin H, Schlomm T, Henke RP . Prostate cancers in the transition zone: Part 1; pathological aspects. BJU Int 2004; 94: 1221–1225.
Acknowledgements
This study was supported by National Cancer Institute (NCI) Specialized Program of Research Excellence Grant P50 CA-921310, NCI Grant R01 CA-100938 and a donation from the LB Research and Education Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barnard, R., Kobayashi, N. & Aronson, W. Effect of diet and exercise intervention on the growth of prostate epithelial cells. Prostate Cancer Prostatic Dis 11, 362–366 (2008). https://doi.org/10.1038/pcan.2008.6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2008.6
Keywords
This article is cited by
-
Comparative effects of Yi Jin Jing versus Tai Chi exercise training on benign prostatic hyperplasia-related outcomes in older adults: study protocol for a randomized controlled trial
Trials (2016)
-
The Role of Inflammation in the Progression of Benign Prostatic Hyperplasia
Current Bladder Dysfunction Reports (2013)