Key Points
-
Our understanding of how the immune system deals with invading bacterial pathogens has been greatly improved by recent in vivo imaging studies. These studies commonly use novel imaging modalities such as spinning disk and multi-photon confocal microscopy, in combination with strains of mice that are genetically engineered to express fluorescent proteins under the control of cell subset-specific promoters.
-
These studies have revealed that intravascular migration is necessary for efficient transendothelial migration of neutrophils and monocytes. Also, monocytes (in the dermal vasculature and other sites) and invariant natural killer T (iNKT) cells (specifically in the hepatic microvasculature) undergo intravascular migration or crawling, potentially as a form of constitutive immune surveillance of the microvasculature.
-
Endothelial cells also contribute to innate immune responses to bacterial pathogens. They express the cellular machinery necessary for responses to bacteria (such as Toll-like receptors, MD2 and signalling adaptor molecules), but also potentially contribute to the inappropriate immune response in sepsis.
-
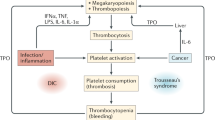
Neutrophils, which use neutrophil extracellular traps (NETs) consisting of chromatin and proteases to trap and kill bacteria, undergo platelet-dependent activation in the vasculature under conditions of high bacteraemia. This results in NET formation within the vasculature; under such circumstances, NETs can act as an additional form of intravascular immunity.
-
Bacteria have evolved a wide range of approaches for evading and/or combating the immune system. These include hiding from immune recognition by adhering to and invading endothelial cells, and inhibiting complement activation.
-
Many bacterial products actively antagonize leukocyte recruitment. These include lipopolysaccharide, which promotes leukocyte retention away from the site of infection and inhibits leukocyte migration, and Staphylococcus aureus proteins such as chemotaxis inhibitory protein of S. aureus and the extracellular adherence protein, which directly inhibit molecules that are involved in leukocyte adhesion and migration.
Abstract
The immune system provides an essential defence against invading pathogens. However, bacteria have evolved numerous strategies to overcome this defence, many of which facilitate systemic dissemination of the pathogen. Nevertheless, the host has evolved many mechanisms to detect and protect against pathogens in the vasculature. Recent studies using new imaging approaches and new mouse models are revealing previously unappreciated functions of this intravascular aspect of the immune system. In this Review, we summarize recent work in this field, highlighting in vivo imaging studies that examine the behaviour of both the immune system and bacteria in the highly dynamic microvasculature.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
von Andrian, U. H. et al. Two-step model of leukocyte–endothelial cell interaction in inflammation: distinct roles for LECAM-1 and the leukocyte β2 integrins in vivo. Proc. Natl Acad. Sci. USA 88, 7538–7542 (1991).
Fiebig, E., Ley, K. & Arfors, K. E. Rapid leukocyte accumulation by “spontaneous” rolling and adhesion in the exteriorized rabbit mesentery. Int. J. Microcirc. Clin. Exp. 10, 127–144 (1991).
Ley, K., Laudanna, C., Cybulsky, M. I. & Nourshargh, S. Getting to the site of inflammation: the leukocyte adhesion cascade updated. Nature Rev. Immunol. 7, 678–689 (2007).
Kansas, G. S. Selectins and their ligands: current concepts and controversies. Blood 88, 3259–3287 (1996).
Petri, B., Phillipson, M. & Kubes, P. The physiology of leukocyte recruitment: an in vivo perspective. J. Immunol. 180, 6439–6446 (2008).
Wong, J. et al. A minimal role for selectins in the recruitment of leukocytes into the inflamed liver microvasculature. J. Clin. Invest. 99, 2782–2790 (1997).
Mizgerd, J. P. et al. Selectins and neutrophil traffic: margination and Streptococcus pneumoniae-induced emigration in murine lungs. J. Exp. Med. 184, 639–645 (1996).
Doerschuk, C. M. et al. The role of P-selectin and ICAM-1 in acute lung injury as determined using blocking antibodies and mutant mice. J. Immunol. 157, 4609–4614 (1996).
Zhuo, L. et al. SHAP potentiates the CD44-mediated leukocyte adhesion to the hyaluronan substratum. J. Biol. Chem. 281, 20303–20314 (2006).
McDonald, B. et al. Interaction of CD44 and hyaluronan is the dominant mechanism for neutrophil sequestration in inflamed liver sinusoids. J. Exp. Med. 205, 915–927 (2008).
Kuligowski, M. P., Kitching, A. R. & Hickey, M. J. Leukocyte recruitment to the inflamed glomerulus: a critical role for platelet-derived P-selectin in the absence of rolling. J. Immunol. 176, 6991–6999 (2006).
Phillipson, M. et al. Intraluminal crawling of neutrophils to emigration sites: a molecularly distinct process from adhesion in the recruitment cascade. J. Exp. Med. 203, 2569–2575 (2006). This is the first study to examine the molecular basis of neutrophil crawling in inflamed postcapillary venules, detailing the relative importance of LFA1 and Mac1 in this process.
Schenkel, A. R., Mamdouh, Z. & Muller, W. A. Locomotion of monocytes on endothelium is a critical step during extravasation. Nature Immunol. 5, 393–400 (2004). This paper adds an additional step to the paradigm of leukocyte migration, movement over the endothelial cell surface, and describes the molecular basis of this process.
Feng, D., Nagy, J. A., Pyne, K., Dvorak, H. F. & Dvorak, A. M. Neutrophils emigrate from venules by a transendothelial cell pathway in response to FMLP. J. Exp. Med. 187, 903–915 (1998).
Carman, C. V. & Springer, T. A. A transmigratory cup in leukocyte diapedesis both through individual vascular endothelial cells and between them. J. Cell Biol. 167, 377–388 (2004).
Kubes, P. & Kanwar, S. Histamine induces leukocyte rolling in post-capillary venules: a P-selectin-mediated event. J. Immunol. 152, 3570–3577 (1994).
Weninger, W. et al. Specialized contributions by α(1, 3)-fucosyltransferase-IV and FucT-VII during leukocyte rolling in dermal microvessels. Immunity 12, 665–676 (2000).
Hogg, J. C., Doerschuk, C. M., Wiggs, B. & Minshall, D. Neutrophil retention during a single transit through the pulmonary circulation. J. Appl. Physiol. 73, 1683–1685 (1992).
Wojciechowski, J. C. & Sarelius, I. H. Preferential binding of leukocytes to the endothelial junction region in venules in situ. Microcirculation 12, 349–359 (2005).
Cuvelier, S. L. & Patel, K. D. Shear-dependent eosinophil transmigration on interleukin 4-stimulated endothelial cells: a role for endothelium-associated eotaxin-3. J. Exp. Med. 194, 1699–1709 (2001).
Auffray, C. et al. Monitoring of blood vessels and tissues by a population of monocytes with patrolling behavior. Science 317, 666–670 (2007). This paper uses intravital microscopy of transgenic CX 3 CR1GFP/+ mice to provide the first demonstration of spontaneous monocyte intralumenal crawling, or 'patrolling', throughout the entire microvasculature.
Audoy-Remus, J. et al. Rod-shaped monocytes patrol the brain vasculature and give rise to perivascular macrophages under the influence of proinflammatory cytokines and angiopoietin-2. J. Neurosci. 28, 10187–10199 (2008).
Malaviya, R., Ikeda, T., Ross, E. & Abraham, S. N. Mast cell modulation of neutrophil influx and bacterial clearance at sites of infection through TNF-α. Nature 381, 77–80 (1996).
Rogers, D. E. Host mechanisms which act to remove bacteria from the blood stream. Bacteriol. Rev. 24, 50–66 (1960).
Wardle, E. N. Kupffer cells and their function. Liver 7, 63–75 (1987).
MacPhee, P. J., Schmidt, E. E. & Groom, A. C. Evidence for Kupffer cell migration along liver sinusoids, from high-resolution in vivo microscopy. Am. J. Physiol. 263, G17–G23 (1992).
Lee, W. Y. & Kubes, P. Leukocyte adhesion in the liver: distinct adhesion paradigm from other organs. J. Hepatol. 48, 504–512 (2008).
Helmy, K. Y. et al. CRIg: a macrophage complement receptor required for phagocytosis of circulating pathogens. Cell 124, 915–927 (2006). This study identifies and characterizes CRIg, which is a new member of the complement system that is expressed by Kupffer cells and has a crucial role in capture of C3-opsonized particles, including bacteria, from the circulation.
Johansson, A. G., Sundqvist, T. & Skogh, T. IgG immune complex binding to and activation of liver cells. An in vitro study with IgG immune complexes, Kupffer cells, sinusoidal endothelial cells and hepatocytes. Int. Arch. Allergy Immunol. 121, 329–336 (2000).
van Egmond, M. et al. FcαRI-positive liver Kupffer cells: reappraisal of the function of immunoglobulin A in immunity. Nature Med. 6, 680–685 (2000).
Dellabona, P., Padovan, E., Casorati, G., Brockhaus, M. & Lanzavecchia, A. An invariant V alpha 24-J alpha Q/V beta 11 T cell receptor is expressed in all individuals by clonally expanded CD4−8− T cells. J. Exp. Med. 180, 1171–1176 (1994).
Park, S. H. et al. The mouse CD1d-restricted repertoire is dominated by a few autoreactive T cell receptor families. J. Exp. Med. 193, 893–904 (2001).
Bendelac, A., Savage, P. B. & Teyton, L. The biology of NKT cells. Annu. Rev. Immunol. 25, 297–336 (2007).
Geissmann, F. et al. Intravascular immune surveillance by CXCR6+ NKT cells patrolling liver sinusoids. PLoS Biol. 3, e113 (2005). Using CXCR6GFP/+ transgenic mice, in which GFP is expressed exclusively in NKT cells, this study uses in vivo imaging to show that NKT cells spontaneously migrate throughout the hepatic sinusoids, where they respond to activating stimuli.
Velazquez, P. et al. Cutting Edge: activation by innate cytokines or microbial antigens can cause arrest of natural killer T cell patrolling of liver sinusoids. J. Immunol. 180, 2024–2028 (2008).
Campos, R. A. et al. Cutaneous immunization rapidly activates liver invariant Vα14 NKT cells stimulating B-1 B cells to initiate T cell recruitment for elicitation of contact sensitivity. J. Exp. Med. 198, 1785–1796 (2003).
Tupin, E., Kinjo, Y. & Kronenberg, M. The unique role of natural killer T cells in the response to microorganisms. Nature Rev. Microbiol. 5, 405–417 (2007).
Kudo, S., Matsuno, K., Ezaki, T. & Ogawa, M. A novel migration pathway for rat dendritic cells from the blood: hepatic sinusoids–lymph translocation. J. Exp. Med. 185, 777–784 (1997).
Winau, F. et al. Ito cells are liver-resident antigen-presenting cells for activating T cell responses. Immunity 26, 117–129 (2007).
Warren, A. et al. T lymphocytes interact with hepatocytes through fenestrations in murine liver sinusoidal endothelial cells. Hepatology 44, 1182–1190 (2006).
Hachem, P. et al. α-galactosylceramide-induced iNKT cells suppress experimental allergic asthma in sensitized mice: role of IFN-γ. Eur. J. Immunol. 35, 2793–2802 (2005).
Aird, W. C. Phenotypic heterogeneity of the endothelium: I. structure, function, and mechanisms. Circ. Res. 100, 158–173 (2007).
Dauphinee, S. M. & Karsan, A. Lipopolysaccharide signaling in endothelial cells. Lab. Invest. 86, 9–22 (2006).
Dunzendorfer, S., Lee, H. K. & Tobias, P. S. Flow-dependent regulation of endothelial Toll-like receptor 2 expression through inhibition of SP1 activity. Circ. Res. 95, 684–691 (2004).
Li, J. et al. CpG DNA-mediated immune response in pulmonary endothelial cells. Am. J. Physiol. Lung Cell. Mol. Physiol. 287, L552–L558 (2004).
Andonegui, G. et al. Endothelium-derived Toll-like receptor-4 is the key molecule in LPS-induced neutrophil sequestration into lungs. J. Clin. Invest. 111, 1011–1020 (2003).
Hollingsworth, J. W. et al. The critical role of hematopoietic cells in lipopolysaccharide-induced airway inflammation. Am. J. Respir. Crit. Care Med. 171, 806–813 (2005).
Ye, X., Ding, J., Zhou, X., Chen, G. & Liu, S. F. Divergent roles of endothelial NF-κB in multiple organ injury and bacterial clearance in mouse models of sepsis. J. Exp. Med. 205, 1303–1315 (2008).
Finlay, B. B. & McFadden, G. Anti-immunology: evasion of the host immune system by bacterial and viral pathogens. Cell 124, 767–782 (2006).
Foster, T. J. Immune evasion by staphylococci. Nature Rev. Microbiol. 3, 948–958 (2005).
Yipp, B. G. et al. Profound differences in leukocyte–endothelial cell responses to lipopolysaccharide versus lipoteichoic acid. J. Immunol. 168, 4650–4658 (2002).
Welbourn, C. R. & Young, Y. Endotoxin, septic shock and acute lung injury: neutrophils, macrophages and inflammatory mediators. Br. J. Surg. 79, 998–1003 (1992).
Holman, J. M. Jr & Saba, T. M. Hepatocyte injury during post-operative sepsis: activated neutrophils as potential mediators. J. Leukoc. Biol. 43, 193–203 (1988).
Erzurum, S. C. et al. Mechanisms of lipopolysaccharide-induced neutrophil retention. Relative contributions of adhesive and cellular mechanical properties. J. Immunol. 149, 154–162 (1992).
Clark, S. R. et al. Platelet TLR4 activates neutrophil extracellular traps to ensnare bacteria in septic blood. Nature Med. 13, 463–469 (2007). This study shows that neutrophil binding of LPS-activated platelets leads to neutrophil activation and NET formation, even under flow conditions in vivo.
Ibbotson, G. C. et al. Functional α4-integrin: a newly identified pathway of neutrophil recruitment in critically ill septic patients. Nature Med. 7, 465–470 (2001).
Czermak, B. J. et al. Protective effects of C5a blockade in sepsis. Nature Med. 5, 788–792 (1999).
Rittirsch, D. et al. Functional roles for C5a receptors in sepsis. Nature Med. 14, 551–557 (2008).
Huber-Lang, M. et al. Generation of C5a in the absence of C3: a new complement activation pathway. Nature Med. 12, 682–687 (2006). This study shows that thrombin can function as a C5 convertase, thereby providing the first demonstration of a C3-independent pathway of complement activation and linking the complement and coagulation systems.
Nauseef, W. M. How human neutrophils kill and degrade microbes: an integrated view. Immunol. Rev. 219, 88–102 (2007).
Brinkmann, V. et al. Neutrophil extracellular traps kill bacteria. Science 303, 1532–1535 (2004). This study provides the first description of NETs.
Fuchs, T. A. et al. Novel cell death program leads to neutrophil extracellular traps. J. Cell Biol. 176, 231–241 (2007).
Brinkmann, V. & Zychlinsky, A. Beneficial suicide: why neutrophils die to make NETs. Nature Rev. Microbiol. 5, 577–582 (2007).
Sumby, P. et al. Extracellular deoxyribonuclease made by group A Streptococcus assists pathogenesis by enhancing evasion of the innate immune response. Proc. Natl Acad. Sci. USA 102, 1679–1684 (2005).
Buchanan, J. T. et al. DNase expression allows the pathogen group A Streptococcus to escape killing in neutrophil extracellular traps. Curr. Biol. 16, 396–400 (2006).
Wartha, F. et al. Capsule and D-alanylated lipoteichoic acids protect Streptococcus pneumoniae against neutrophil extracellular traps. Cell. Microbiol. 9, 1162–1171 (2007).
Marshall, B. T. et al. Direct observation of catch bonds involving cell-adhesion molecules. Nature 423, 190–193 (2003).
Sokurenko, E. V., Vogel, V. & Thomas, W. E. Catch-bond mechanism of force-enhanced adhesion: counterintuitive, elusive, but widespread? Cell Host Microbe 4, 314–323 (2008).
Laschke, M. W., Kerdudou, S., Herrmann, M. & Menger, M. D. Intravital fluorescence microscopy: a novel tool for the study of the interaction of Staphylococcus aureus with the microvascular endothelium in vivo. J. Infect. Dis. 191, 435–443 (2005).
Que, Y. A. et al. Fibrinogen and fibronectin binding cooperate for valve infection and invasion in Staphylococcus aureus experimental endocarditis. J. Exp. Med. 201, 1627–1635 (2005).
Kerdudou, S. et al. Fibronectin binding proteins contribute to the adherence of Staphylococcus aureus to intact endothelium in vivo. Thromb. Haemost. 96, 183–189 (2006).
Cundell, D. R., Gerard, N. P., Gerard, C., Idanpaan-Heikkila, I. & Tuomanen, E. I. Streptococcus pneumoniae anchor to activated human cells by the receptor for platelet-activating factor. Nature 377, 435–438 (1995).
Ho, M., Hickey, M. J., Murray, A. G., Andonegui, G. & Kubes, P. Visualization of Plasmodium falciparum–endothelium interactions in human microvasculature: mimicry of leukocyte recruitment. J. Exp. Med. 192, 1205–1211 (2000).
Moriarty, T. J. et al. Real-time high resolution 3D imaging of the Lyme disease spirochete adhering to and escaping from the vasculature of a living host. PLoS Pathog. 4, e1000090 (2008).
Norman, M. U. et al. Molecular mechanisms involved in vascular interactions of the Lyme disease pathogen in a living host. PLoS Pathog. 4, e1000169 (2008).
Benach, J. L., Coleman, J. L., Garcia-Monco, J. C. & Deponte, P. C. Biological activity of Borrelia burgdorferi antigens. Ann. NY Acad. Sci. 539, 115–125 (1988).
Tilly, K. et al. Borrelia burgdorferi OspC protein required exclusively in a crucial early stage of mammalian infection. Infect. Immun. 74, 3554–3564 (2006).
Alitalo, A. et al. Complement evasion by Borrelia burgdorferi: serum-resistant strains promote C3b inactivation. Infect. Immun. 69, 3685–3691 (2001).
Kraiczy, P., Skerka, C., Brade, V. & Zipfel, P. F. Further characterization of complement regulator-acquiring surface proteins of Borrelia burgdorferi. Infect. Immun. 69, 7800–7809 (2001).
Kraiczy, P., Skerka, C., Kirschfink, M., Brade, V. & Zipfel, P. F. Immune evasion of Borrelia burgdorferi by acquisition of human complement regulators FHL-1/reconectin and factor H. Eur. J. Immunol. 31, 1674–1684 (2001).
Caswell, C. C. et al. The Scl1 protein of M6-type group A Streptococcus binds the human complement regulatory protein, factor H, and inhibits the alternative pathway of complement. Mol. Microbiol. 67, 584–596 (2008).
Foxman, E. F., Campbell, J. J. & Butcher, E. C. Multistep navigation and the combinatorial control of leukocyte chemotaxis. J. Cell Biol. 139, 1349–1360 (1997). Using an under agarose in vitro migration assay, this study examines the behaviour of neutrophils that are exposed to a complex milieu of overlapping chemotactic gradients and shows that they can sequentially migrate along gradients generated by different chemoattractants to reach the target site.
Heit, B., Tavener, S., Raharjo, E. & Kubes, P. An intracellular signaling hierarchy determines direction of migration in opposing chemotactic gradients. J. Cell Biol. 159, 91–102 (2002).
Li, Z. et al. Regulation of PTEN by Rho small GTPases. Nature Cell Biol. 7, 399–404 (2005).
Heit, B. et al. PTEN functions to 'prioritize' chemotactic cues and prevent 'distraction' in migrating neutrophils. Nature Immunol. 9, 743–752 (2008).
Khan, A. I., Heit, B., Andonegui, G., Colarusso, P. & Kubes, P. Lipopolysaccharide: a p38 MAPK-dependent disrupter of neutrophil chemotaxis. Microcirculation 12, 421–432 (2005).
Lokuta, M. A. & Huttenlocher, A. TNF-α promotes a stop signal that inhibits neutrophil polarization and migration via a p38 MAPK pathway. J. Leukoc. Biol. 78, 210–219 (2005).
Jack, D. L., Klein, N. J. & Turner, M. W. Mannose-binding lectin: targeting the microbial world for complement attack and opsonophagocytosis. Immunol. Rev. 180, 86–99 (2001).
Hickey, M. J. et al. Molecular and cellular basis of microvascular perfusion deficits induced by Clostridium perfringens and Clostridium septicum. PLoS Pathog. 4, e1000045 (2008).
Rooijakkers, S. H. et al. Immune evasion by a staphylococcal complement inhibitor that acts on C3 convertases. Nature Immunol. 6, 920–927 (2005).
Rooijakkers, S. H. et al. Early expression of SCIN and CHIPS drives instant immune evasion by Staphylococcus aureus. Cell. Microbiol. 8, 1282–1293 (2006).
Wang, R. et al. Identification of novel cytolytic peptides as key virulence determinants for community-associated MRSA. Nature Med. 13, 1510–1514 (2007).
Bestebroer, J. et al. Staphylococcal superantigen-like 5 binds PSGL-1 and inhibits P-selectin-mediated neutrophil rolling. Blood 109, 2936–2943 (2007).
Bone, R. C. The pathogenesis of sepsis. Ann. Intern. Med. 115, 457–469 (1991).
Mavrommatis, A. C. et al. Coagulation system and platelets are fully activated in uncomplicated sepsis. Crit. Care Med. 28, 451–457 (2000).
Mercer, K. W., Macik, B. G. & Williams, M. E. Hematologic disorders in critically ill patients. Semin. Respir. Crit. Care Med. 27, 286–296 (2006).
Stohlawetz, P. et al. Effects of endotoxemia on thrombopoiesis in men. Thromb. Haemost. 81, 613–617 (1999).
Andonegui, G. et al. Platelets express functional Toll-like receptor-4. Blood 106, 2417–2423 (2005).
Acknowledgements
This work is supported by a programme grant (334067) from the National Health and Medical Research Council of Australia. M.J.H. is a National Health and Medical Research Council senior research fellow.
Author information
Authors and Affiliations
Corresponding author
Related links
Glossary
- Intravital microscopy study
-
An examination of biological processes, such as leukocyte–endothelial cell interactions, in living tissue. In general, translucent tissues are used, such as the mesentery or cremaster muscle, which can be exteriorized and mounted for microscopic observation.
- High endothelial venule
-
(HEV). A specialized venule that is found in secondary lymphoid organs, except the spleen. HEVs allow continuous transmigration of lymphocytes as a consequence of the constitutive expression of adhesion molecules and chemokines at their luminal surface.
- Shear stress
-
The force exerted by the flowing blood (dynes) on each unit of area of endothelial surface (cm2); measured in dynes per cm2.
- Kupffer cell
-
A large, specialized ramified macrophage that lines the sinusoidal vessels of the liver. Kupffer cells regulate local immune responses and remove microbial particles, endotoxins and other noxious substances that penetrate the portal venous system.
- Spinning disk confocal microscopy
-
Form of confocal microscopy in which confocality is achieved using a spinning disk with numerous pinholes, replacing the more conventional laser scanning process that is used in many confocal microscopes. The main advantage of this form of confocal microscopy is the rapid rate of image capture (up to ∼15 frames per second), which enables examination of rapidly motile cells and bacteria in the vasculature.
- C3 receptor
-
A receptor that mediates responses to the complement components C3 and C3a. Four C3 fragment receptors have been identified: CR1 (CD35), CR2 (CD21), CR3 (CD11b–CD18) and CR4 (CD11c–CD18). However, none of these receptors has been described to be functional on Kupffer cells.
- Contact sensitization
-
The inflammatory immune reactions that occur in the skin after the administration of a sensitizing antigen. These reactions occur after the second and subsequent exposures to a particular sensitizing antigen and involve the recruitment and responses of effector T cells.
- Ito cell
-
A type of pericyte that is found in the space of Disse and is the main reservoir of retinol in the liver.
- Space of Disse
-
The space between the sinusoidal endothelial cells and hepatocytes in which Ito cells are found. Given the discontinuous nature of the sinusoidal endothelium, this space is filled with blood plasma. Hepatocytes extend microvilli into the space of Disse, thereby increasing their surface area for metabolite exchange.
- Fenestrated endothelium
-
Large holes (fenestrations) of the endothelium of the hepatic sinusoids, which allow plasma in the sinusoids to freely access the space of Disse.
- Toll-like receptor
-
(TLR). A receptor belonging to a family that recognizes conserved products that are unique to microorganisms (such as lipopolysaccharide), which are known as pathogen-associated molecular patterns. TLR-mediated events signal to the host that a microbial pathogen is present.
- Caecal ligation and puncture
-
An experimental model of peritonitis in rodents, in which the caecum is ligated and then punctured, thereby forming a small hole. This leads to leakage of intestinal bacteria into the peritoneal cavity and subsequent peritoneal infection.
Rights and permissions
About this article
Cite this article
Hickey, M., Kubes, P. Intravascular immunity: the host–pathogen encounter in blood vessels. Nat Rev Immunol 9, 364–375 (2009). https://doi.org/10.1038/nri2532
Issue Date:
DOI: https://doi.org/10.1038/nri2532
This article is cited by
-
The roles of neutrophils in non-tuberculous mycobacterial pulmonary disease
Annals of Clinical Microbiology and Antimicrobials (2023)
-
Mechanisms of fungal dissemination
Cellular and Molecular Life Sciences (2021)
-
Taurine chloramine selectively regulates neutrophil degranulation through the inhibition of myeloperoxidase and upregulation of lactoferrin
Amino Acids (2020)
-
Nonlytic exocytosis of Cryptococcus neoformans from neutrophils in the brain vasculature
Cell Communication and Signaling (2019)
-
Effector CD4+ T cells recognize intravascular antigen presented by patrolling monocytes
Nature Communications (2018)