Abstract
Complement degradation product C4d has become an important marker of humoral or antibody-mediated rejection in renal and heart allograft biopsies. Although there have been several reports on the detection of C4d in liver allografts, the significance of C4d in liver transplantation and its relationship with humoral rejection are still not clear. We investigated the frequency and pattern of C4d staining in liver allograft biopsies with reference to preoperative lymphocyte crossmatch tests, which detect donor-reactive lymphocyte antibody. Survival rates at 5 years were 77% for crossmatch-negative patients and 53% for crossmatch-positive patients (P=0.009). In crossmatch-negative patients, reproducible positive staining was obtained in 28 of 86 (33%) biopsies taken within 90 days after transplantation and 33 of 96 (34%) biopsies 90 days or after transplantation. Most C4d staining was observed in the portal areas, and no clear correlation was observed between C4d positivity and histological diagnosis. In crossmatch-positive patients, 9 of 11 (82%) biopsies showed positivity for C4d. C4d stained perivenular areas as well as portal areas. Histology of crossmatch-positive patients included acute rejection and cholangitis, but did not include periportal changes that were seen in humoral rejection in ABO-incompatible liver transplantation. In summary, focal C4d deposition was seen in various types of liver allograft injury and had little clinical impact on crossmatch-negative patients, but extensive C4d staining in crossmatch-positive patients may be associated with humoral rejection and poor graft survival.
Similar content being viewed by others
Main
The occurrence of cellular rejection or T-cell-mediated rejection is well known in any solid organ transplantation, but the significance of humoral or antibody-mediated rejection in liver allograft remains uncertain. In clinical practice, hyperacute rejection is very rare, and some initial reports suggested that liver allografts were much more resistant to humoral rejection than other solid organ allografts.1, 2, 3 It is natural for the liver to be considered an ‘immunologically privileged organ’, and cadaveric donor liver transplantation is usually performed without considering human leukocyte antigen (HLA) matching.4
However, other studies including the most recent reported that some cases of positive lymphocyte crossmatch or positive panel reactive antibody were associated with decreased liver graft survival.5, 6, 7 Histological changes included portal edema with neutrophilic infiltration and platelet thrombi in the venules, accompanied by ductular proliferation and cholestasis.5 These changes are similar to the changes seen in biliary stricture. Histological diagnostic criteria for humoral rejection have not been established in liver allografts.
In contrast, the importance of clinical humoral rejection caused by preformed anti-donor-HLA antibody is widely recognized in kidney and heart transplantation. For pathological evaluation, C4d deposition has now been accepted as an important marker for the assessment of humoral or antibody-mediated rejection, which causes acute and chronic allograft dysfunction and graft loss.8, 9, 10
The role of C4d in the evaluation of humoral rejection in liver allografts has not been clearly described.8 Recent papers reported the demonstration of C4d in liver allografts, especially in allografts showing cellular or apparent humoral rejection, but the status of anti-donor antibodies was not described in most cases.11, 12, 13, 14, 15, 16, 17, 18, 19 In ABO-incompatible transplantation, our group reported that portal stromal C4d immunostaining was associated with a high postoperative titer of anti-A/B antibody and reduced graft survival, suggesting the association of C4d deposition and ABO-incompatible humoral rejection.20
In this study, we focused on the role of C4d immunohistochemistry in ABO-identical/compatible liver allografts with reference to preformed alloantibodies evaluated by lymphocyte crossmatch tests. We also evaluated the pattern of C4d deposition and conventional morphology.
Materials and methods
Case Selection and Clinical Backgrounds
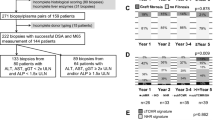
Between January 1996 and December 2005, 764 primary living donor liver transplantations were performed in Kyoto University without ABO incompatibility. This series included liver transplantation for both children (age under 16, 356 patients) and adults (age 16 or older, 408 patients). Deceased donor liver transplantation, ABO-incompatible transplantation and re-transplantation were not included in this study. The patients' characteristics are shown in Table 1. Among them, 749 (98%) were crossmatch-negative patients and 15 (2%) were crossmatch-positive. As of July 2006, 2627 allograft biopsies (crossmatch-negative, 2595; crossmatch-positive, 32) were taken after living donor liver transplantation. For the evaluation of crossmatch-negative patients, 10% of biopsies were selected from every other ten accession numbers, and biopsies that were not given definitive histological diagnosis or did not contain five or more portal tracts were excluded from the study. In this method, we selected 182 biopsies from 152 patients for C4d staining. For crossmatch-positive patients, 32 biopsies were obtained from 11 patients. Among them, all first postoperative biopsies and five follow-up biopsies were available for C4d staining.
The baseline immunosuppression protocol consisted of tacrolimus and low-dose steroids. For tacrolimus, the post-transplant target whole-blood trough level was 10–12 ng/ml during the first 2 weeks and the dose was tapered thereafter. Maintenance trough level after 3 months transplantation was around 5 ng/ml in most cases. Steroids were started at graft reperfusion at a dose of 10 mg/kg, and then gradually reduced and discontinued. Biopsy-proven rejection was treated with steroid bolus therapy. Around 2000, mycophenolate mophetil was administered for selected patients with steroid-resistant rejection.
Lymphocyte Crossmatch Test
Pretransplant lymphocyte crossmatch test was performed using both direct complement-dependent cytotoxicity and anti-human globulin. Incubation was performed using 1 μl of donor lymphocyte suspension and 5 μl of recipient serum in a Terasaki plate (Nunc, Roskilde, Denmark) at room temperature for 30 min. For anti-human globulin-enhanced complement-dependent cytotoxicity, anti-human globulin (Goat IgG κ and λ light chains) was added and incubated at room temperature for 3 min. Five microliters of rabbit complement was added to each well and the mixture was incubated at room temperature for 60 min. Two microliters of 5% eosin solution was added and the cells were fixed with formalin. The plate was examined using phase contrast microscopy (IMT-2, Olympus; Tokyo, Japan). The results were considered positive when more than 20% of the donor lymphocytes were killed by the recipient's serum in either test.
Histological Examination
Eighteen-gauge liver core tissue biopsies were placed in 10% buffered formalin from several hours to overnight, processed routinely and sliced into 3 μm paraffin sections. The staining methods for routine histological evaluation included hematoxylin and eosin, Masson trichrome and immunostaining of cytokeratin 7 (OV-TL 12/30, DakoCytomation, Denmark, dilution 1:200). Staining was performed for two serial sections.
Histologic diagnosis was by pathologists (HS, HH, MCW and AMH) in routine clinical practice. The diagnosis of acute rejection and chronic rejection was made according to Banff criteria.21, 22 Diagnosis of HCV hepatitis was made considering the levels of serum HCV RNA. Combination of lobular changes with apoptotic hepatocytes and slight portal inflammation was diagnosed as ‘lobular hepatitis C’, suggesting early recurrent hepatitis C.23 Cholangitis was diagnosed using the standard criteria of surgical pathology and confirmed by the presence of biliary leak, biliary stricture, or infection.
To clarify the effect of antibody-mediated rejection in early and late postoperative courses, each biopsy was categorized as early (taken no earlier than 90 days posttransplantation) or late (obtained later than 90 days after transplantation).
C4d Immunostaining and Control Materials
The polyclonal antibody against C4d complement (BI-RC4D; Biomedica, Vienna, Austria, 1:50) was used for immunostaining with an automated immunostainer (BENCHMARK®XT, Ventana Medical Systems, Tucson, AZ, USA). For antigen retrieval, deparaffinized and rehydrated sections were treated with protease I (Ventana, 0.5 U/ml) at 37°C for 20 min.
We used lymphoid tissue with follicular hyperplasia as a positive control for C4d staining.24 A reticular staining pattern in germinal centers was confirmed in every C4d immunostaining. As for other positive control specimens, several liver allograft biopsies and one kidney allograft biopsy from ABO-incompatible transplantation were also available.25 ABO-incompatible humoral rejection showed strong portal and periportal C4d staining in the liver. Glomerular and peritubular capillary staining was seen in the kidney. Five needle biopsies of living donor candidates with near-normal histology and 10 wedge biopsies of the liver allografts taken during graft resection (time-zero biopsy) were used as negative controls.
Evaluation of C4d Immunostaining
Two pathologists (HS and HH) independently evaluated the C4d immunostaining slides of the liver biopsies. To minimize false-negative cases, biopsies showing any portal stromal or endothelial staining were evaluated as positive.26 Stromal positivity was recorded with or without endothelial staining.20 Biopsies in which only vascular endothelium was stained were evaluated as endothelial-only positive. Staining involving 50% or more of the portal tracts was classified as diffuse, whereas less than 50% as focal. Staining of hepatocytes or sinusoids was recorded but not categorized as diffuse or focal. Faint connective tissue staining outside the liver parenchyma and staining of elastic fibers were regarded as nonspecific and considered negative. Completely negative staining was evaluated as negative.
Statistical Analysis
Statistical significance of differences among groups was assessed by Fisher's exact test or analysis of variance (ANOVA). Patient survival was determined by Kaplan–Meier analysis and differences in survival were analyzed by the log-rank test. For all analyses, P-values of less than 0.05 were taken as significant.
Results
Survival of Liver Allografts
As of July 2006, 175 crossmatch-negative patients and seven crossmatch-positive patients died or underwent retransplantation. Crossmatch-negative patients showed significantly better graft survival rate at 5 years than crossmatch-positive patients (77 vs 53%, P=0.009, Figure 1). Causes of graft loss in crossmatch-negative patients consisted of sepsis or multiorgan failure (47%), recurrence of original disease (16%), rejection or de novo autoimmune hepatitis (15%), anastomotic complication (7%), and others (14%). In crossmatch-positive patients, three (43%) died of sepsis, three (43%) died of anastomotic complication (two hepatic artery rupture and one massive hemorrhage), and one (14%) underwent retransplantation for probable portal overperfusion due to small-for-size graft.
C4d Immunostaining and Histology in Crossmatch-Negative Patients
Representative C4d staining patterns are shown in Figure 2. The intensity of endothelial-only staining varied, being usually focal but distinctly positive in capillaries in the portal tracts (Figure 2a). Sinusoidal staining was unusual and faint. Staining in the internal elastic lamina of the hepatic artery was occasionally seen in nontransplant settings and was considered nonspecific (Figure 2b). In portal stromal staining, C4d staining was observed in the stroma surrounding portal capillaries or bile ducts (Figure 2c).
Representative C4d staining in crossmatch-negative patients. Capillary staining of C4d in the portal area showing acute rejection (a). Internal lamina of the hepatic artery (b). Acute rejection with portal stromal staining surrounding blood vessels or bile ducts (c). Faint capsular staining in time-zero biopsy (d).
The hepatic capsule was usually negative and faint staining in time-zero biopsy was regarded as negative (Figure 2d).
Table 2 shows the results of early biopsies in crossmatch-negative patients. Among these, 28 of 86 cases (33%) showed stromal- or endothelial-positive staining. The highest frequency was seen in moderate to severe acute rejection (35%), but that was not significantly different from lobular hepatitis C (33%) or early chronic rejection (33%). The most common staining pattern was endothelial-only staining. The focal stromal staining pattern was most frequently seen in moderate to severe acute rejection showing C4d positivity (7/12, 58%), but was also observed in lobular hepatitis C (1/3, 33%) and early chronic rejection (1/2, 50%).
Table 3 shows the results of late biopsies in crossmatch-negative patients. Positive staining was seen in 33 of 96 (34%) biopsies. Chronic hepatitis C tended to show a lower frequency of C4d (2/13, 15%). Chronic rejection revealed positivity in four of five (80%), and all showed endothelial staining. The focal stromal staining pattern was seen in two cases of lobular hepatitis C, one case of chronic hepatitis C, one case of de novo autoimmune hepatitis, and one case of recurrent primary biliary cirrhosis. C4d staining did not affect those patients' graft survival (data not shown).
C4d Immunostaining and Clinicopathological Results in Crossmatch-Positive Patients
Clinicopathological features of crossmatch-positive patients are summarized in Table 4. Nine of 11 (82%) initial biopsies showed C4d positivity, which was significantly higher than biopsies from crossmatch-negative patients (82 vs 34%, P=0.002). Seven of nine (77%) stainings were associated with perivenular or lobular C4d deposition as well as portal stroma. Two late biopsies were included in C4d-positive biopsies. Representative portal and perivenular staining patterns in crossmatch-positive patients are shown in Figure 3.
C4d staining in crossmatch-positive patients. (a, b) Case 14 (day 8) showing acute rejection with portal stromal C4d staining; (c, d) case 11 (day 18) with minimal portal inflammation with portal stromal staining; (e, f) case 14 (day 8) centrilobular necrosis with perivenular and hepatocyte C4d staining; (g, h) case 15 (day 3) lobular inflammation with sinusoidal macrophage proliferation and steatosis demonstrating perivenular C4d deposition.
The histology of those seven stromal-positive cases varied: two cases of moderate to severe acute rejection, two acute cholangitis, one lobular inflammation, one hepatocanalicular cholestasis, and one portal hemorrhage were included. Typical periportal edema and periportal necrosis, which we observed in early humoral rejection in ABO-incompatible transplantation, were not evident in those patients.
Second postoperative biopsies were available in cases 6, 7, 13, 14, and 15. Cases 6 and 15 showed persistent endothelial and stromal staining at postoperative day 74 and 13, respectively. Cases 7, 13, and 14 were negative for C4d at days 723, 911, and F410, respectively.
Three of the four patients whose biopsy was not available died within 30 days after transplantation. Three of the seven with C4d stromal positivity died within 90 days after transplantation. One of two patients with endothelial staining died 118 days after transplantation. Two patients whose biopsy was negative for C4d were alive and well.
Discussion
In crossmatch-negative patients, more than half of the biopsies were completely negative for C4d, but various histologies showed C4d staining in early and late postoperative courses. As in other reports, late-phase chronic rejection tended to show a high percentage of C4d positivity and chronic hepatitis C showed low C4d positivity.15, 18 However, less than half of the acute rejection cases showed C4d positivity, and a similar frequency of C4d staining was observed in lobular hepatitis C, which makes it difficult to use C4d as a marker of acute rejection in patients with hepatitis C infection. In this series, C4d staining for crossmatch-negative and ABO-compatible/identical liver transplantation does not seem to be a useful marker for histological diagnosis. C4d deposition in those biopsies may be a reaction to nonspecific cellular injury including infection and rejection.
Controversy remains regarding the significance of C4d and its staining pattern in liver transplantation. So far, there is no consensus as to the anatomic pattern of C4d staining in liver allograft rejection. The differences of staining protocols including the type of materials (frozen or formalin-fixed tissue), type of C4d antibodies, and antigen retrieval can affect the results of C4d staining. At present, the only consensus is that there is virtually no immunoreactivity for C4d in normal liver or time-zero biopsy at liver transplantation. The Berlin group reported that half or more of patients diagnosed with acute rejection showed C4d deposits along portal vessels, mainly portal veins, and C4d may be a useful marker to distinguish acute rejection from recurrent hepatitis C.11, 14, 15 Other groups emphasized that hepatic lobules or sinusoidal deposition was more specific in hepatic rejection and may be useful to differentiate rejection from recurrent viral hepatitis.12, 16, 17, 18 Complement activation in the sinusoids may be seen in conditions other than rejection, and clinicopathological correlation is always necessary in the evaluation of C4d deposition.27, 28 Nonspecific staining should also be excluded using proper positive and negative controls. As proposed in the meeting report of a national conference to assess antibody-mediated rejection, humoral rejection should be characterized by (1) clinical, (2) morphologic, (3) immunopathologic, and (4) serologic evidence.9 Recently, Watson et al29 reported a clearcut case of antibody-mediated rejection including distinct sinusoidal C4d deposition. They also observed mild C4d deposition in the portal areas but described the changes as nondiagnostic, although hematoxylin–eosin-stained specimens showed significant morphological changes in portal tracts.
In our study, lymphocyte crossmatch-positive patients showed reduced graft survival and strong C4d staining, which suggested the possible effect of humoral rejection. C4d deposition in crossmatch-positive patients was seen in perivenular areas as well as in portal areas.
It may be thought that the major drawback of this study was the lack of data from frozen tissue. C4d on paraffin sections tended to be less sensitive than on frozen sections.30 In our routine practice, obtaining frozen tissue was difficult. Possible low sensitivity, however, did not seem to affect the value of C4d staining in liver transplantation. Our results are that only strong and extensive staining can have clinical impact and that faint staining seems to be negligible in our routine practice.
In cellular rejection, most inflammatory response is localized in the portal tracts and perivenular areas, which are rich in HLA class II antigen.31, 32 Sinusoidal endothelium is generally not a main target for the cellular immune response; rather, liver sinusoidal endothelial cells might be associated with resistance of the liver to cellular-mediated rejection.33, 34
In humoral rejection, on the other hand, target cells with alloantigens would be directly recognized by alloantibodies, and the anatomic patterns of liver injury are expected to parallel the distribution of antigens. ABO antigens are relatively restricted to portal areas,35, 36 whereas HLA class I are expressed on all endothelial cells.37 There is also a report suggesting that antibodies against sinusoidal cells can be related to rejection episodes.38 Although our current protocol of C4d staining using paraffin-embedded sections did not always demonstrate sinusoidal endothelial staining, perivenular staining was observed in crossmatch-positive patients. Considering these facts, crossmatch-positive humoral rejection may be characterized by more widely distributed C4d deposition than the usual acute ‘cellular’ rejection or ABO-incompatible humoral rejection.
In this series, the histology of crossmatch-positive cases did not include typical periportal edema or hemorrhage, which was typical of ABO-incompatible rejection.25 Only one case showed massive hemorrhagic necrosis in biopsy, but was clinically attributed to small-for-size graft and portal overperfusion. Acute rejection and purulent cholangitis are the most frequent histology, but nonspecific changes such as lobular inflammation or cholestasis were also observed. It seems safe to conclude that conventional morphological evaluation is not diagnostic in crossmatch-positive humoral rejection, and immunopathological evaluation is necessary.5, 29
Clinically, causes of graft loss in crossmatch-positive patients were difficult to evaluate. It is of note that the patients died of sepsis or vascular complication or both. It has already been reported that crossmatch-positive patients were more likely to suffer from sepsis in the early period after transplantation.6, 7 Vascular complication may be explained by vascular damage caused by humoral rejection, but why sepsis relates to humoral rejection remains unclear. In cases of sepsis, humoral rejection might be masked by the histology of ‘septic cholangitis’ or unrecognized because of a lack of biopsy and immunopathological studies.
A previous study by our group demonstrated that positive flowcytometry crossmatch was associated with a higher rate of clinical rejection episodes in pediatric patients but was not associated with graft survival.39 That study did not include adult patients and flowcytometry was used instead of a complement cytotoxicity test. In this study, crossmatch positivity was associated with reduced graft survival, and all graft failures occurred in women. Complement-dependent cytotoxicity seemed less sensitive but more specific for the prediction of severe humoral rejection. Infants or young children often escape severe humoral rejection or achieve accommodation in ABO-incompatible transplantation, and this may be the case in crossmatch-positive transplantation.10, 40 On the other hand, caution should be taken for female patients with children or patients who received a transfusion since they have a higher risk of sensitization to allogenic HLA antigens.6
In conclusion, C4d deposit in ABO-compatible/identical liver transplantation, unlike in kidney or cardiac transplantation, is not always specifically associated with rejection histology; however, extensive staining of C4d suggested possible humoral rejection in crossmatch-positive patients. Clinicopathological correlation is essential in the evaluation of C4d immunostaining in liver transplantation.
References
Gordon RD, Fung JJ, Iwatsuki S, et al. Immunological factors influencing liver graft survival. Gastroenterol Clin N Am 1988;17:53–59.
Furuya T, Murase N, Nakamura K, et al. Preformed lymphocytotoxic antibodies: the effects of class, titer and specificity on liver vs heart allografts. Hepatology 1992;16:1415–1422.
Donaldson PT, Thomson LJ, Heads A, et al. IgG donor-specific crossmatches are not associated with graft rejection or poor graft survival after liver transplantation. An assessment by cytotoxicity and flow cytometry. Transplantation 1995;60:1016–1023.
Wang-Rodriguez J, Rearden A . Effect of crossmatching on outcome in organ transplantation. Crit Rev Clin Lab Sci 1995;32:345–376.
Demetris AJ, Nakamura K, Yagihashi A, et al. A clinicopathological study of human liver allograft recipients harboring preformed IgG lymphocytotoxic antibodies. Hepatology 1992;16:671–681.
Charco R, Vargas V, Balsells J, et al. Influence of anti-HLA antibodies and positive T-lymphocytotoxic crossmatch on survival and graft rejection in human liver transplantation. J Hepatol 1996;24:452–459.
Muro M, Marin L, Miras M, et al. Liver recipients harbouring anti-donor preformed lymphocytotoxic antibodies exhibit a poor allograft survival at the first year after transplantation: experience of one centre. Transplant Immunol 2005;14:91–97.
Racusen LC, Colvin RB, Solez K, et al. Antibody-mediated rejection criteria—an addition to the Banff 97 classification of renal allograft rejection. Am J Transplant 2003;3:708–714.
Takemoto SK, Zeevi A, Feng S, et al. National conference to assess antibody-mediated rejection in solid organ transplantation. Am J Transplant 2004;4:1033–1041.
Colvin RB, Smith RN . Antibody-mediated organ-allograft rejection. Nat Rev Immunol 2005;5:807–817.
Krukemeyer MG, Moeller J, Morawietz L, et al. Description of B lymphocytes and plasma cells, complement, and chemokines/receptors in acute liver allograft rejection. Transplantation 2004;78:65–70.
Sawada T, Shimizu A, Kubota K, et al. Lobular damage caused by cellular and humoral immunity in liver allograft rejection. Clin Transplant 2005;19:110–114.
Moeller J, Krukemeyer MG, Morawietz L, et al. Molecular case report: IgVH analysis in acute humoral and cellular liver allograft rejection suggests a selected accumulation of effector B cells and plasma cells. Virchows Arch 2005;446:325–332.
Dankof A, Schmeding M, Morawietz L, et al. Portal capillary C4d deposits and increased infiltration by macrophages indicate humorally mediated mechanisms in acute cellular liver allograft rejection. Virchows Arch 2005;447:87–93.
Schmeding M, Dankof A, Krenn V, et al. C4d in acute rejection after liver transplantation—a valuable tool in differential diagnosis to hepatitis C recurrence. Am J Transplant 2006;6:523–530.
Bu X, Zheng Z, Yu Y, et al. Significance of C4d deposition in the diagnosis of rejection after liver transplantation. Transplant Proc 2006;38:1418–1421.
Jain A, Mohanka R, Orloff M, et al. Characterization of CD4, CD8, CD56 positive lymphocytes and C4d deposits to distinguish acute cellular rejection from recurrent hepatitis C in post-liver transplant biopsies. Clin Transplant 2006;20:624–633.
Lorho R, Turlin B, Aqodad N, et al. C4d: a marker for hepatic transplant rejection. Transplant Proc 2006;38:2333–2334.
Troxell ML, Higgins JP, Kambham N . Evaluation of C4d staining in liver and small intestine allografts. Arch Pathol Lab Med 2006;130:1489–1496.
Haga H, Egawa H, Fujimoto Y, et al. Acute humoral rejection and C4d immunostaining in ABO blood type-incompatible liver transplantation. Liver Transplant 2006;12:457–464.
International Panel. Banff schema for grading liver allograft rejection: an international consensus document. Hepatology 1997;25:658–663.
Demetris A, Adams D, Bellamy C, et al. Update of the International Banff Schema for Liver Allograft Rejection: working recommendations for the histopathologic staging and reporting of chronic rejection. An International Panel. Hepatology 2000;31:792–799.
Yoshizawa A, Takada Y, Fujimoto Y, et al. Liver transplantation from an identical twin without immunosuppression, with early recurrence of Hepatitis C. Am J Transplant 2006;6:2812–2816.
Zwirner J, Felber E, Schmidt P, et al. Complement activation in human lymphoid germinal centres. Immunology 1989;66:270–277.
Haga H, Egawa H, Shirase T, et al. Periportal edema and necrosis as diagnostic histological features of early humoral rejection in ABO-incompatible liver transplantation. Liver Transplant 2004;10:16–27.
Nadasdy GM, Bott C, Cowden D, et al. Comparative study for the detection of peritubular capillary C4d deposition in human renal allografts using different methodologies. Hum Pathol 2005;36:1178–1185.
Demetris AJ, Jaffe R, Tzakis A, et al. Antibody-mediated rejection of human orthotopic liver allografts. A study of liver transplantation across ABO blood group barriers. Am J Pathol 1988;132:489–502.
Straatsburg IH, Boermeester MA, Wolbink GJ, et al. Complement activation induced by ischemia-reperfusion in humans: a study in patients undergoing partial hepatectomy. J Hepatol 2000;32:783–791.
Watson R, Kozlowski T, Nickeleit V, et al. Isolated donor specific alloantibody-mediated rejection after ABO compatible liver transplantation. Am J Transplant 2006;6:3022–3029.
Seemayer CA, Gaspert A, Nickeleit V, et al. C4d staining of renal allograft biopsies: a comparative analysis of different staining techniques. Nephrol Dial Transplant 2007;22:568–576.
Takacs L, Szende B, Monostori E, et al. Expression of HLA-DR antigens on bile duct cells of rejected liver transplant. Lancet 1983;2:1500.
Hubscher SG, Adams DH, Elias E . Changes in the expression of major histocompatibility complex class II antigens in liver allograft rejection. J Pathol 1990;162:165–171.
Katz SC, Pillarisetty VG, Bleier JI, et al. Liver sinusoidal endothelial cells are insufficient to activate T cells. J Immunol 2004;173:230–235.
Onoe T, Ohdan H, Tokita D, et al. Liver sinusoidal endothelial cells have a capacity for inducing nonresponsiveness of T cells across major histocompatibility complex barriers. Transpl Int 2005;18:206–214.
Tanaka Y, Haga H, Egawa H, et al. Intragraft expression of recipient-type ABO blood group antigens: long-term follow-up and histological features after liver transplantation. Liver Transpl 2005;11:547–554.
Terada T, Nakanuma Y . Expression of ABH blood group antigens, Ulex europaeus agglutinin I, and type IV collagen in the sinusoids of hepatocellular carcinoma. Arch Pathol Lab Med 1991;115:50–55.
Barbatis C, Woods J, Morton JA, et al. Immunohistochemical analysis of HLA (A, B, C) antigens in liver disease using a monoclonal antibody. Gut 1981;22:985–991.
Sumitran-Holgersson S, Ge X, Karrar A, et al. A novel mechanism of liver allograft rejection facilitated by antibodies to liver sinusoidal endothelial cells. Hepatology 2004;40:1211–1221.
Kasahara M, Kiuchi T, Takakura K, et al. Postoperative flow cytometry crossmatch in living donor liver transplantation: clinical significance of humoral immunity in acute rejection. Transplantation 1999;67:568–575.
Egawa H, Oike F, Buhler L, et al. Impact of recipient age on outcome of ABO-incompatible living-donor liver transplantation. Transplantation 2004;77:403–411.
Acknowledgements
We thank Ms Koyanagi, Ms Yamane, and Ms Tanaka for technical assistance with immunostaining. This work was partly supported by a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (17590301).
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure/conflict of interest
None declared.
Rights and permissions
About this article
Cite this article
Sakashita, H., Haga, H., Ashihara, E. et al. Significance of C4d staining in ABO-identical/compatible liver transplantation. Mod Pathol 20, 676–684 (2007). https://doi.org/10.1038/modpathol.3800784
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3800784
Keywords
This article is cited by
-
Current status of liver transplantation across ABO blood-type barrier
Journal of Hepato-Biliary-Pancreatic Surgery (2008)