Abstract
The contribution of molecular alterations in bone marrow mesenchymal stromal cells (BM-MSC) to the pathogenesis of acute myeloid leukemia (AML) is poorly understood. Thus we assessed genome-wide genetic, transcriptional and epigenetic alterations in BM-MSC derived from AML patients (AML BM-MSC). Whole-exome sequencing (WES) of AML BM-MSC samples from 21 patients revealed a non-specific pattern of genetic alterations in the stromal compartment. The only mutation present in AML BM-MSC at serial time points of diagnosis, complete remission and relapse was a mutation in the PLEC gene encoding for cytoskeleton key player Plectin in one AML patient. Healthy donor controls did not carry genetic alterations as determined by WES. Transcriptional profiling using RNA sequencing revealed deregulation of proteoglycans and adhesion molecules as well as cytokines in AML BM-MSC. Moreover, KEGG pathway enrichment analysis unravelled deregulated metabolic pathways and endocytosis in both transcriptional and DNA methylation signatures in AML BM-MSC. Taken together, we report molecular alterations in AML BM-MSC suggesting global changes in the AML BM microenvironment. Extended investigations of these altered niche components may contribute to the design of niche-directed therapies in AML.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Morrison SJ, Scadden DT . The bone marrow niche for haematopoietic stem cells. Nature 2014; 505: 327–334.
Boulais PE, Frenette PS . Making sense of hematopoietic stem cell niches. Blood 2015; 125: 2621–2629.
Calvi LM, Link DC . Cellular complexity of the bone marrow hematopoietic stem cell niche. Calcif Tissue Int 2014; 94: 112–124.
Geyh S, Rodriguez-Paredes M, Jager P, Khandanpour C, Cadeddu RP, Gutekunst J et al. Functional inhibition of mesenchymal stromal cells in acute myeloid leukemia. Leukemia 2015; 30: 683–691.
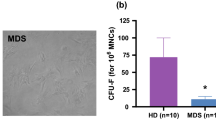
Geyh S, Oz S, Cadeddu RP, Frobel J, Bruckner B, Kundgen A et al. Insufficient stromal support in MDS results from molecular and functional deficits of mesenchymal stromal cells. Leukemia 2013; 27: 1841–1851.
Lim M, Pang Y, Ma S, Hao S, Shi H, Zheng Y et al. Altered mesenchymal niche cells impede generation of normal hematopoietic progenitor cells in leukemic bone marrow. Leukemia 2015; 30: 154–162.
Medyouf H, Mossner M, Jann JC, Nolte F, Raffel S, Herrmann C et al. Myelodysplastic cells in patients reprogram mesenchymal stromal cells to establish a transplantable stem cell niche disease unit. Cell Stem Cell 2014; 14: 824–837.
Schepers K, Pietras EM, Reynaud D, Flach J, Binnewies M, Garg T et al. Myeloproliferative neoplasia remodels the endosteal bone marrow niche into a self-reinforcing leukemic niche. Cell Stem Cell 2013; 13: 285–299.
Colmone A, Amorim M, Pontier AL, Wang S, Jablonski E, Sipkins DA . Leukemic cells create bone marrow niches that disrupt the behavior of normal hematopoietic progenitor cells. Science 2008; 322: 1861–1865.
Kim JA, Shim JS, Lee GY, Yim HW, Kim TM, Kim M et al. Microenvironmental remodeling as a parameter and prognostic factor of heterogeneous leukemogenesis in acute myelogenous leukemia. Cancer Res 2015; 75: 2222–2231.
Winkler IG, Barbier V, Nowlan B, Jacobsen RN, Forristal CE, Patton JT et al. Vascular niche E-selectin regulates hematopoietic stem cell dormancy, self renewal and chemoresistance. Nat Med 2012; 18: 1651–1657.
Jacamo R, Chen Y, Wang Z, Ma W, Zhang M, Spaeth EL et al. Reciprocal leukemia-stroma VCAM-1/VLA-4-dependent activation of NF-kappaB mediates chemoresistance. Blood 2014; 123: 2691–2702.
Konopleva M, Konoplev S, Hu W, Zaritskey AY, Afanasiev BV, Andreeff M . Stromal cells prevent apoptosis of AML cells by up-regulation of anti-apoptotic proteins. Leukemia 2002; 16: 1713–1724.
Kode A, Manavalan JS, Mosialou I, Bhagat G, Rathinam CV, Luo N et al. Leukaemogenesis induced by an activating beta-catenin mutation in osteoblasts. Nature 2014; 506: 240–244.
Raaijmakers MH, Mukherjee S, Guo S, Zhang S, Kobayashi T, Schoonmaker JA et al. Bone progenitor dysfunction induces myelodysplasia and secondary leukaemia. Nature 2010; 464: 852–857.
Wu G, Feng X, Stein L . A human functional protein interaction network and its application to cancer data analysis. Genome Biol 2010; 11: R53.
Shannon P, Markiel A, Ozier O, Baliga NS, Wang JT, Ramage D et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res 2003; 13: 2498–2504.
Mondal T, Subhash S, Vaid R, Enroth S, Uday S, Reinius B et al. MEG3 long noncoding RNA regulates the TGF-beta pathway genes through formation of RNA-DNA triplex structures. Nat Commun 2015; 6: 7743.
Subhash S, Kanduri C GeneSCF: Gene set clustering based on functional annotation, 2014. http://github.com/santhilalsubhash/geneSCF.git.
Bindea G, Mlecnik B, Hackl H, Charoentong P, Tosolini M, Kirilovsky A et al. ClueGO: a Cytoscape plug-in to decipher functionally grouped gene ontology and pathway annotation networks. Bioinformatics 2009; 25: 1091–1093.
Bindea G, Galon J, Mlecnik B . CluePedia Cytoscape plugin: pathway insights using integrated experimental and in silico data. Bioinformatics 2013; 29: 661–663.
Rozen S, Skaletsky H . Primer3 on the WWW for general users and for biologist programmers. Methods Mol Biol 2000; 132: 365–386.
Baldus CD, Tanner SM, Ruppert AS, Whitman SP, Archer KJ, Marcucci G et al. BAALC expression predicts clinical outcome of de novo acute myeloid leukemia patients with normal cytogenetics: a Cancer and Leukemia Group B Study. Blood 2003; 102: 1613–1618.
Bakker E, Qattan M, Mutti L, Demonacos C, Krstic-Demonacos M . The role of microenvironment and immunity in drug response in leukemia. Biochim Biophys Acta 2016; 1863: 414–426.
Bentivegna A, Miloso M, Riva G, Foudah D, Butta V, Dalpra L et al. DNA methylation changes during in vitro propagation of human mesenchymal stem cells: implications for their genomic stability? Stem Cells Int 2013; 2013: 192425.
Blau O, Baldus CD, Hofmann WK, Thiel G, Nolte F, Burmeister T et al. Mesenchymal stromal cells of myelodysplastic syndrome and acute myeloid leukemia patients have distinct genetic abnormalities compared with leukemic blasts. Blood 2011; 118: 5583–5592.
Blau O, Hofmann WK, Baldus CD, Thiel G, Serbent V, Schumann E et al. Chromosomal aberrations in bone marrow mesenchymal stroma cells from patients with myelodysplastic syndrome and acute myeloblastic leukemia. Exp Hematol 2007; 35: 221–229.
Cai J, Miao X, Li Y, Smith C, Tsang K, Cheng L et al. Whole-genome sequencing identifies genetic variances in culture-expanded human mesenchymal stem cells. Stem Cell Reports 2014; 3: 227–233.
Palumbo Jr A, Da Costa Nde O, Bonamino MH, Pinto LF, Nasciutti LE . Genetic instability in the tumor microenvironment: a new look at an old neighbor. Mol Cancer 2015; 14: 145.
Andra K, Nikolic B, Stocher M, Drenckhahn D, Wiche G . Not just scaffolding: plectin regulates actin dynamics in cultured cells. Genes Dev 1998; 12: 3442–3451.
Lunter PC, Wiche G . Direct binding of plectin to Fer kinase and negative regulation of its catalytic activity. Biochem Biophys Res Commun 2002; 296: 904–910.
Bausch D, Thomas S, Mino-Kenudson M, Fernandez-del CC, Bauer TW, Williams M et al. Plectin-1 as a novel biomarker for pancreatic cancer. Clin Cancer Res 2011; 17: 302–309.
Sanna V, Nurra S, Pala N, Marceddu S, Pathania D, Neamati N et al. Targeted nanoparticles for the delivery of novel bioactive molecules to pancreatic cancer cells. J Med Chem 2016; 59: 5209–5220.
Huang JC, Basu SK, Zhao X, Chien S, Fang M, Oehler VG et al. Mesenchymal stromal cells derived from acute myeloid leukemia bone marrow exhibit aberrant cytogenetics and cytokine elaboration. Blood Cancer J 2015; 5: e302.
Binato R, de Almeida Oliveira NC, Du Rocher B, Abdelhay E . The molecular signature of AML mesenchymal stromal cells reveals candidate genes related to the leukemogenic process. Cancer Lett 2015; 369: 134–143.
Civini S, Jin P, Ren J, Sabatino M, Castiello L, Jin J et al. Leukemia cells induce changes in human bone marrow stromal cells. J Transl Med 2013; 11: 298.
Chen S, Zambetti NA, Bindels EM, Kenswill K, Mylona AM, Adisty NM et al. Massive parallel RNA sequencing of highly purified mesenchymal elements in low-risk MDS reveals tissue-context-dependent activation of inflammatory programs. Leukemia 2016; 30: 1938–1942.
Mosesson Y, Mills GB, Yarden Y . Derailed endocytosis: an emerging feature of cancer. Nat Rev Cancer 2008; 8: 835–850.
Sigismund S, Confalonieri S, Ciliberto A, Polo S, Scita G, Di Fiore PP . Endocytosis and signaling: cell logistics shape the eukaryotic cell plan. Physiol Rev 2012; 92: 273–366.
Sorkin A, von Zastrow M . Endocytosis and signalling: intertwining molecular networks. Nat Rev Mol Cell Biol 2009; 10: 609–622.
Kawamoto T, Ohga N, Akiyama K, Hirata N, Kitahara S, Maishi N et al. Tumor-derived microvesicles induce proangiogenic phenotype in endothelial cells via endocytosis. PLoS One 2012; 7: e34045.
Pavlova NN, Thompson CB . The emerging hallmarks of cancer metabolism. Cell Metab 2016; 23: 27–47.
Carito V, Bonuccelli G, Martinez-Outschoorn UE, Whitaker-Menezes D, Caroleo MC, Cione E et al. Metabolic remodeling of the tumor microenvironment: migration stimulating factor (MSF) reprograms myofibroblasts toward lactate production, fueling anabolic tumor growth. Cell Cycle 2012; 11: 3403–3414.
Moschoi R, Imbert V, Nebout M, Chiche J, Mary D, Prebet T et al. Protective mitochondrial transfer from bone marrow stromal cells to acute myeloid leukemic cells during chemotherapy. Blood 2016; 128: 253–264.
Iozzo RV, Sanderson RD . Proteoglycans in cancer biology, tumour microenvironment and angiogenesis. J Cell Mol Med 2011; 15: 1013–1031.
Baghy K, Iozzo RV, Kovalszky I . Decorin-TGFbeta axis in hepatic fibrosis and cirrhosis. J Histochem Cytochem 2012; 60: 262–268.
Goldoni S, Humphries A, Nystrom A, Sattar S, Owens RT, McQuillan DJ et al. Decorin is a novel antagonistic ligand of the Met receptor. J Cell Biol 2009; 185: 743–754.
Hu Y, Sun H, Owens RT, Wu J, Chen YQ, Berquin IM et al. Decorin suppresses prostate tumor growth through inhibition of epidermal growth factor and androgen receptor pathways. Neoplasia 2009; 11: 1042–1053.
Oda G, Sato T, Ishikawa T, Kawachi H, Nakagawa T, Kuwayama T et al. Significance of stromal decorin expression during the progression of breast cancer. Oncol Rep 2012; 28: 2003–2008.
Sofeu Feugaing DD, Gotte M, Viola M . More than matrix: the multifaceted role of decorin in cancer. Eur J Cell Biol 2013; 92: 1–11.
Jarvinen TA, Prince S . Decorin: a growth factor antagonist for tumor growth inhibition. Biomed Res Int 2015; 2015: 654765.
Ichii M, Frank MB, Iozzo RV, Kincade PW . The canonical Wnt pathway shapes niches supportive of hematopoietic stem/progenitor cells. Blood 2012; 119: 1683–1692.
Bernasconi P, Farina M, Boni M, Dambruoso I, Calvello C . Therapeutically targeting self-reinforcing leukemic niches in acute myeloid leukemia (AML): a worthy endeavour? Am J Hematol 2016; 91: 507–517.
Matsunaga T, Takemoto N, Sato T, Takimoto R, Tanaka I, Fujimi A et al. Interaction between leukemic-cell VLA-4 and stromal fibronectin is a decisive factor for minimal residual disease of acute myelogenous leukemia. Nat Med 2003; 9: 1158–1165.
Gao Z, Zhang L, Hu J, Sun Y . Mesenchymal stem cells: a potential targeted-delivery vehicle for anti-cancer drug, loaded nanoparticles. Nanomedicine 2013; 9: 174–184.
Acknowledgements
We gratefully acknowledge funding of the project by Deutsche Krebshilfe as well as German Cancer Translational Consortium (DKTK) and the DKTK joint funding project 'Evaluation of new therapeutic concepts in AML'. Moreover, we thank the High Throughput Sequencing Unit at the DKFZ Genomics and Proteomics Core Facility for providing the Illumina Whole-exome sequencing, whole-genome expression and methylation arrays and related services. Furthermore, we thank Vera Arnemann and colleagues of the Charité Institute of Pathology for helpful assistance with the immunohistochemical stainings.
Author contributions
Conception and design of study: PAG and CDB; patient and donor samples: DN, WKH, CDB; experiments, collection and assembly of data: EKvdH, JOT, KI, CS, ML, LHM, KJ, IA; data analysis and interpretation: EKvdH, MN, SV, ARJ, MPS, PAG, CDB; manuscript writing and editing: EKvdH, MN, LHM, PAG, CDB.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Leukemia website
Supplementary information
Rights and permissions
About this article
Cite this article
von der Heide, E., Neumann, M., Vosberg, S. et al. Molecular alterations in bone marrow mesenchymal stromal cells derived from acute myeloid leukemia patients. Leukemia 31, 1069–1078 (2017). https://doi.org/10.1038/leu.2016.324
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2016.324
This article is cited by
-
Mesenchymal stromal cell senescence in haematological malignancies
Cancer and Metastasis Reviews (2023)
-
Aberrant DNA methylation impacts HOX genes expression in bone marrow mesenchymal stromal cells of myelodysplastic syndromes and de novo acute myeloid leukemia
Cancer Gene Therapy (2022)
-
Bone marrow-derived mesenchymal stem/stromal cells in patients with acute myeloid leukemia reveal transcriptome alterations and deficiency in cellular vitality
Stem Cell Research & Therapy (2021)
-
Bone marrow derived stromal cells from myelodysplastic syndromes are altered but not clonally mutated in vivo
Nature Communications (2021)
-
Is Myelodysplasia a Consequence of Normal Aging?
Current Oncology Reports (2021)