Abstract
Neutrophils are physiologically associated with platelets in whole blood. Inflammatory reactions can be modulated by the presence of platelets. To investigate the influence of platelets on neutrophil activity, we studied the 5-lipoxygenase (5-LOX) metabolic pathway in normal human blood neutrophils stimulated with f-Met-Leu-Phe (fMLP) or monosodium urate monohydrate (MSUM) in the presence of autologous platelets. Platelets inhibited by more than 90% the synthesis of leukotriene B4 and 5-HETE in neutrophils activated with fMLP or MSUM. The addition of exogenous arachidonic acid did not reverse the inhibitory effect of platelets on 5-LOX–generated metabolites in fMLP- or MSUM-activated neutrophils. Preincubation of neutrophils with adenosine deaminase reversed the inhibitory effect of platelets in fMLP-treated neutrophils, indicating that adenosine was responsible for the platelet inhibition of leukotriene B4 and 5-HETE formation. In contrast, adenosine deaminase had no influence on the inhibitory effects of platelets in MSUM-stimulated cells. These results suggest that platelets can inhibit the synthesis of 5-LOX products (a) by acting mainly downstream to phospholipase A2 in cells stimulated by fMLP or MSUM, (b) through adenosine when neutrophils are activated with fMLP, and (c) by an adenosine-independent mechanism in MSUM-activated neutrophils by an as-yet-unidentified mediator.
Similar content being viewed by others
Introduction
Leukotriene B4 (LTB4) release leads to major biologic consequences associated with inflammation. This arachidonic acid (AA) metabolite is one of the most potent inflammatory chemoattractants of polymorphonuclear and mononuclear phagocytes (Ford-Hutchinson, 1990). Besides neutrophil chemotaxis and aggregation, LTB4 induces neutrophil degranulation and lysosomal enzyme release (Sha’afi et al, 1981) and neutrophil endothelial cell adhesion (Hoover et al, 1984), is involved in immune modulation (Henderson, 1994; Poubelle et al, 1991), and mediates inflammatory pain (Levine et al, 1984). LTB4 is generated through a cytosolic LTA4-hydrolase (Radmark et al, 1984). The unstable compound LTA4 is formed through the action of 5-lipoxygenase (5-LOX) on AA in the presence of a 5-LOX–activating protein (FLAP), leading to 5-hydroperoxyeicosatetraenoic acid (5-HPETE) (Rouzer et al, 1985). This intermediate metabolite is further converted into LTA4 by 5-LOX and into 5-HETE by glutathione peroxidase. Since its discovery in 1979 (Borgeat and Samuelsson, 1979), LTB4 and the other bioactive 5-LOX–derived products have been the focus of an intense research to obtain 5-LOX and FLAP inhibitors and more specifically LTB4 antagonists. Neutrophils also have the capacity to metabolize LTB4 directly into a less active mediator 20-OH-LTB4 and an inactive product 20-COOH-LTB4.
Deposits of platelets in inflamed tissues during neutrophil margination are associated with cell-to-cell interactions and modulation of the inflammatory process (Issekutz et al, 1983). Platelets and neutrophils exert multiple and complex functions in pathophysiologic conditions of inflammation (Poubelle and Borgeat, 2002). Activated platelets adhere to neutrophils (Jungi et al, 1986) through their α-granule membrane glycoprotein GMP-140 (or P-selectin) (Larsen et al, 1989) and the integrin complex GPIIb/IIIa-fibrinogen (Spangenberg et al, 1993). Aggregates of platelets and neutrophils lead to metabolic or functional interactions between these cells (Ginsburg and Quie, 1980; Marcus et al, 1982; McGarrity et al, 1988; Weksler, 1983). For instance, LTA4 from neutrophils is metabolized by platelets into LTC4 (Maclouf et al, 1989) and lipoxins (Serhan and Sheppard, 1990). However, 12-HETE from platelets is converted to 12,20-diHETE by unstimulated neutrophils (Marcus et al, 1984). Platelets activated with thrombin can increase LTB4 synthesis by neutrophils in the presence of zymosan, f-Met-Leu-Phe (fMLP), C5a, or PAF (Palmantier and Borgeat, 1991). Conversely, co-incubation of washed platelets with neutrophils activated by the nonphysiologic stimulus ionophore A23187 is associated with an increase of 12-HETE and a decrease of 5-HETE, LTB4, and thromboxane B2 (Maderna et al, 1993). In addition, neutrophils can inhibit the AA metabolism in platelets stimulated with thrombin, collagen, or ionophore (Chabannes et al, 1994). Platelets from healthy subjects also have the capacity to modulate neutrophil superoxide anion production and chemiluminescence depending on the stimulus used in vitro (Carulli et al, 1995; Colli et al, 1996). However, platelets from uremic or allergic patients are altered and are unable to decrease the production of superoxide anion (Carulli et al, 1995) or LTB4 by A23187-activated neutrophils (Hosni et al, 1991). Circulating platelets bind to neutrophils, and platelet-neutrophil complexes have been demonstrated in whole blood (Rinder et al, 1991). Such a satellitism, already described in 1974 (Kjeldsberg and Swanson, 1974), may have potent pathophysiologic relevance because at rest, 25% of blood neutrophils are complexed with platelets, and after platelet activation with ADP or thrombin, such complexes rise to 70% (Peters et al, 1997). Besides their phlogogenic activity through interactions with neutrophils, platelets can counterbalance neutrophil activation. Platelets from healthy donors can reduce LTB4 synthesis in A23187-stimulated neutrophils from allergics (Hosni et al, 1991). Thus, unactivated platelets might act as a natural inhibitor of LTB4 formation by neutrophils in diseases such as bacterial infection or arthritis. To address this question, we investigated the effects of normal human blood platelets on the 5-LOX activity of autologous neutrophils stimulated with the pathophysiologic stimuli fMLP, a biologically active ligand produced by bacteria, or monosodium urate monohydrate (MSUM) crystals, the causal agent of gout. The results of the present study demonstrate that platelets have the capacity to abrogate the synthesis of LTB4 and 5-HETE in fMLP- and MSUM-activated neutrophils. The inhibitory influence of platelets on the synthesis of LTB4 and 5-HETE was not reversed by the addition of exogenous AA, suggesting an effect of platelets downstream to the neutrophil phospholipase A2 (PLA2). A candidate to this platelet inhibitory factor could be adenosine, an endogenous product that down-regulates ligand-stimulated LTB4 biosynthesis in neutrophil suspensions (Krump et al, 1997). As suspected, adenosine was the platelet inhibitory factor of LTB4 and 5-HETE generated by fMLP-activated neutrophils, whereas platelet inhibition of MSUM-stimulated neutrophils was independent of adenosine.
Results
Effects of Autologous Platelets on LTB4 and 5-HETE Synthesis by Neutrophils
As fMLP and MSUM crystals alone are weak agonists to stimulate the production of leukotrienes detected by HPLC, all of the experiments were conducted in conditions in which the available endogenous substrate AA could be increased. Therefore, studies of the effects of fMLP were carried out with neutrophils pretreated with thimerosal to inhibit the reacylation of AA into phospholipids. In these conditions, the 5-lipoxygenase products measured were previously reported to be approximately 200 pmol/ml of incubate compared with 1000 pmol/ml when neutrophils were stimulated by 0.5 μm ionophore A23187 in the absence of thimerosal (Chabannes et al, 1997). Studies of the effects of MSUM crystals were performed with neutrophils primed by GM-CSF, a factor that has been reported to increase the production of leukotrienes induced by phagocytosis (Poubelle et al, 1989) through an enhancement of the release of AA (DiPersio et al, 1988). Note that despite a pretreatment of neutrophils with thimerosal or GM-CSF, platelets were shown to exert a significant effect on AA metabolism in neutrophils activated by a soluble or a particulate agonist (see below). It is also useful to stress that MSUM, unlike fMLP, can stimulate platelets to release AA (Serhan et al, 1984).
Figure 1 shows the amounts of LTA4-derived products (LTB4 + 20-OH-LTB4 + trans-isomers of LTB4) and 5-HETE synthesized by neutrophils (N) stimulated with 1 μm fMLP in the absence or in the presence of autologous platelets (P) with a ratio of P/N = 30/1. Inhibition of the synthesis of 5-LOX–derived products was correlated to platelet concentration and was almost complete (80% to 90% inhibition) at a ratio of 30P/1N; a 50% inhibition was recorded at 10P/1N (not shown). Unactivated platelets significantly inhibited the accumulation of LTA4-derived products and 5-HETE by 90% and 89%, respectively (n = 20, p < 0.001). In these experimental conditions, LTB4, 20-OH-LTB4, Δ6-trans-LTB4, and 12-epi-Δ6-trans-LTB4 represent 70%, 21%, 6%, and 3% of LTA4-derived metabolites, respectively.
Effect of autologous platelets on 5-LOX–derived products generation by human blood neutrophils stimulated by fMLP. Neutrophils preincubated with thimerosal were further incubated with 1 μm fMLP in the absence or presence of platelets (platelet/neutrophil ratio: 30/1) for 5 minutes at 37° C. LTA4-derived products (LTB4 + 20-OH-LTB4 + trans-isomers of LTB4) and 5-HETE were measured by RP-HPLC, and amounts are expressed in picomoles formed by 107 neutrophils/ml. Results are the mean ± sem of 20 separate experiments carried out in duplicate. Significant differences between fMLP-activated neutrophils (N) with or without platelets (P) were evaluated by the Wilcoxon paired rank-sum test.
Figure 2 shows the amounts of 5-LOX–derived metabolites released by neutrophils activated with 1 mg/ml MSUM crystals without or with platelets (P/N = 30/1). Neutrophils in the absence of platelets generated 64 ± 20, 76 ± 15, and 26 ± 12 pmol LTB4, 20-OH-LTB4, and 5-HETE, respectively. No trans-isomers of LTB4 were detectable in these experimental conditions. LTB4 and 20-OH-LTB4 represent 46% and 54% of LTA4-derived metabolites, respectively. The presence of platelets significantly inhibited the accumulation of 5-LOX metabolites in neutrophils from 166 ± 63 pmol to 16 ± 5 pmol (LTB4 + 20-OH-LTB4 + 5-HETE) with an inhibitory effect of 90% (n = 7, p < 0.02). Co-incubation of platelets with neutrophils stimulated by fMLP or MSUM did not lead to detectable amounts of 5,12-diHETE (not shown).
Effect of autologous platelets on 5-LOX–derived products generation by human blood neutrophils stimulated by MSUM crystals. Neutrophils preincubated with GM-CSF were further incubated with 1 mg/ml MSU in the absence or presence of platelets (platelet/neutrophil ratio: 30/1) for 15 minutes at 37° C. LTA4-derived products (LTB4 + 20-OH-LTB4 + trans-isomers of LTB4) and 5-HETE were measured by RP-HPLC, and amounts are expressed in picomoles formed by 107 neutrophils/ml. Results are the mean ± sem of seven separate experiments carried out in duplicate. Significant differences between MSU-activated neutrophils (N) with or without platelets (P) were evaluated by the Wilcoxon paired rank-sum test.
Noninvolvement of Platelet 12-LOX and COX in the Inhibition of Neutrophil LTB4 and 5-HETE Synthesis
No 12-HETE or HHT was detectable when neutrophils were incubated without addition of platelets. When platelets were incubated with neutrophils in the presence of MSUM, 12-HETE was 6-fold lower than when platelets were alone (245 ± 70 and 1552 ± 286 pmol/30 × 107 platelets/15 minutes, respectively) whereas HHT was 3.5-fold lower (269 ± 131 and 943 ± 398 pmol, respectively). Similar results were obtained with fMLP (not shown). Moreover, co-incubation of neutrophils and platelets pretreated with 2 μm 5,8,11,14-eicosatetraynoic acid (ETYA), a LOX inhibitor, and 200 μm aspirin, a COX inhibitor, led to similar inhibition of 5-LOX metabolites. Note that depending on the concentration used, ETYA can selectively inhibit 12-LOX in platelets without acting on 5-LOX in neutrophils (Salari et al, 1984). Under the present experimental conditions, ETYA at 2 μm induced no significant modification of the production of AA metabolites by activated neutrophils.
Effect of Platelets on 5-LOX–Derived Products from Neutrophils in the Presence of Exogenous AA
Figure 3 shows the amounts of LTA4-derived products synthesized by neutrophils activated by fMLP or MSUM with a simultaneous addition of AA in the presence or absence of platelets. The addition of 2 or 10 μm AA to fMLP-activated neutrophils alone was associated with an increase of the production of LTA4-derived products (173% and 392% of control, respectively) and 5-HETE (165% and 1265% of control, respectively). When fMLP-activated neutrophils were incubated in the presence of platelets, the addition of 2 or 10 μm AA to cell suspension did not abrogate the inhibitory effect of platelets on LTA4-derived products (Fig. 3A) and 5-HETE (not shown) synthesis by neutrophils. Neutrophils stimulated with MSUM in the presence of 2 or 10 μm AA had a similar increase of their production of LTA4-derived products. The addition of AA to MSUM-stimulated neutrophils in the presence of platelets did not reverse the inhibitory effect of platelets on the synthesis of LTA4-derived products (Fig. 3B). Although the inhibitory effect of platelets was persistent after the addition of AA, the increase of the production of 5-LOX–derived products by neutrophils with platelets was of the same order as that by neutrophils stimulated by the two agonists used, in the absence of platelets.
Effect of exogenous AA on the platelet-induced inhibition of LTA4-derived metabolites synthesized by neutrophils stimulated with fMLP (A) or MSUM (B). Neutrophils preincubated with thimerosal (A) or GM-CSF (B) were further incubated with 1 μm fMLP for 5 minutes at 37° C or 1 mg/ml MSU for 15 minutes at 37° C in the absence or presence of platelets (platelet/neutrophil ratio: 30/1). AA at 2 or 10 μm was simultaneously added to the cell suspensions. LTA4-derived metabolites (LTB4 + 20-OH-LTB4 + trans-isomers of LTB4) were measured by RP-HPLC, and amounts are expressed in picomoles formed by 107 neutrophils/ml. Results are the mean ± sem of three separate experiments carried out in duplicate.
Influence of Adenosine Deaminase on Platelet Inhibition of 5-LOX–Derived Products from Neutrophils
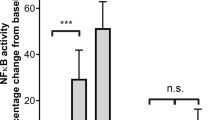
As platelets contain large amounts of nucleotides (D’Souza and Glueck, 1977) that can be converted to adenosine, an endogenous product with anti-inflammatory effects (Cronstein, 1994) and suppressive influence on LTB4 synthesis by ligand-activated neutrophils (Krump et al, 1996), we investigated the effect of adenosine deaminase (ADA) in our experimental conditions of neutrophil-platelet suspensions in the presence of fMLP or MSUM crystals. Figure 4 shows that the effect of ADA depended on the stimulus used to activate neutrophils. ADA completely reversed the inhibitory effect of platelets in fMLP-stimulated neutrophils (Fig. 4A), whereas it had no reversal effect on the platelet inhibition of LTB4 synthesis induced by MSUM (Fig. 4B). These data indicated that adenosine was responsible for the inhibitory effect of platelets when neutrophils were activated by fMLP and that platelet inhibition of LTB4 synthesis by MSUM-activated neutrophils was independent of adenosine.
Effect of ADA on the platelet-induced inhibition of LTA4-derived metabolites synthesized by neutrophils stimulated with fMLP (A) or MSUM (B). ADA at 0.1 U/ml was simultaneously added with platelets to neutrophil suspensions. Neutrophils (N) preincubated with thimerosal (A) or GM-CSF (B) were further incubated with 1 μm fMLP for 5 minutes at 37° C or 1 mg/ml MSU for 15 minutes at 37° C in the absence or presence of platelets (P) at a platelet/neutrophil ratio of 30/1. LTA4-derived metabolites (LTB4 + 20-OH-LTB4 + trans-isomers of LTB4) were measured by RP-HPLC, and amounts are expressed in picomoles formed by 107 neutrophils/ml. Results are the mean ± sem of five separate experiments carried out in duplicate (*p < 0.05).
Discussion
Inflammation is a natural and pathophysiologic process by which mediators originating from the circulation as well as from blood and resident cells are involved in concert to generate a local and/or a systemic reaction of which the final objective is to maintain homeostasis. Interactions between cells can be an important step in controlling the inflammatory reaction. In such a control, the inhibition of production of inflammatory lipid mediators such as LTB4 remains a major therapeutic objective to avoid amplification of the inflammatory process. From this point of view, platelet-neutrophil complexes occurring in whole blood at 25% and increasing up to 70% after stimulation (Peters et al, 1997) is an interesting example of where platelets have been demonstrated to induce activation or inhibition of neutrophil functions depending on the experimental conditions and the parameters studied (Ginsburg and Quie, 1980; Marcus et al, 1982). We present evidence of a direct inhibitory effect of platelets on the generation of LTB4 by human blood neutrophils activated by pathophysiologic agonists of different types, a soluble agonist such as the chemotactic bacterial peptide fMLP, and a particulate agent inducing phagocytosis such as the causal agent of gout MSUM crystals. This effect seems independent of platelet 12-LOX or COX, a conclusion based on the fact that co-incubation of platelets with activated neutrophils led to a significant decrease of 12-LOX– and COX-derived metabolites (12-HETE and HHT, respectively) and that platelets preincubated with 12-LOX and COX inhibitors (eg, ETYA and aspirin, respectively) exhibited a similar inhibitory effect on neutrophil 5-LOX activity. Moreover, this effect remains present after the addition of exogenous AA indicating an inhibition downstream to neutrophil PLA2 and that this platelet inhibitory effect has been related to adenosine in fMLP-stimulated neutrophils but was adenosine-independent in MSUM-activated neutrophils, suggesting another inhibitory product issued from platelets. This mediator has to be determined.
Platelets can convert neutrophil LTA4 into peptido-LTs (Maclouf et al, 1989) and lipoxins (Serhan and Sheppard, 1990). Platelet 12-HETE can be transformed by the neutrophil 5-LOX (Marcus et al, 1984), and neutrophil 5-HETE can be metabolized by platelets through the action of 12-LOX (Goppelt-Struebe et al, 1986), both pathways leading to 5S,12S-diHETE. However, diversion of substrate from neutrophils to platelets seems unlikely to be responsible for the inhibitory effect of platelets on neutrophil generation of 5-LOX metabolites because 5S,12S-diHETE were undetectable when neutrophils were stimulated with fMLP or MSUM and addition of exogenous AA did not modify the inhibitory effect of platelets.
Modulation of AA metabolism during interactions between platelets and neutrophils has been studied extensively using various experimental conditions sometimes leading to apparent discrepant observations. For instance, the 12-LOX of human platelet activates the production of LTB4 by autologous neutrophils through the formation of 12-HPETE using addition of exogenous AA (Maclouf et al, 1982) or 10 μm fMLP and 60 μm AA (Kanaji et al, 1986). Thrombin-activated platelets are also able to increase LTB4 synthesis by human blood neutrophils stimulated with fMLP, PAF, or C5a through a mechanism independent of platelet 12-LOX and COX, possibly through platelet-derived AA (Palmantier and Borgeat, 1991), or to increase LTB4 synthesis by rabbit blood neutrophils stimulated with fMLP through AA originating from platelets (Evangelista et al, 1999). However, human platelets added to neutrophils in the presence of ionophore A23187 can slightly increase LTB4 accumulation while decreasing that of 5-HETE (McCulloch et al, 1992) or can decrease LTB4 synthesis (Maderna et al, 1993), an effect not observed in allergic patients (Hosni et al, 1991). These controversial data prompted us to study the effect of human platelets on blood neutrophils to verify whether the platelet inhibitory effect on LTB4 formation could be demonstrated in conditions using pathophysiologic agonists such as fMLP and MSUM. Size and surface area of crystals may influence their phlogogenic activity (Dieppe et al, 1983; Schumacher et al, 1975). For instance, small urate crystals (≤10 μm) were shown to induce a higher percentage of neutrophil lysis than did larger crystals (Burt et al, 1989). However, urate crystals from 3.9 to 30.6 μm were equally phagocytosed by human leukocytes in vitro and had a similar phlogogenic potential in rabbits (Fam et al, 1992). These discrepancies may be related to differences in the preparations of synthetic crystals (Fam et al, 1992). We used MSUM crystals of size and morphology close to those found in gout as previously characterized (Gaudry et al, 1993). Moreover, they were shown to activate various neutrophil functions such as intracellular calcium mobilization, superoxide anion production, phospholipase D activity, and tyrosine phosphorylation of proteins (Gaudry et al, 1993; Naccache et al, 1991, 1993). Controls in the report by Palmantier and Borgeat (1991), such as fMLP-stimulated neutrophils with unactivated platelets (ratio: 25/1), were not contradictory with our data because they observed a slight decrease of LTB4 accumulation. The major difference in their experimental conditions was the presence of thrombin leading to a drastic increase in LTB4 generation when neutrophils were co-incubated with platelets. It is important to stress that thrombin activates not only platelets but also endothelial cells, leukocytes, and mesenchymal cells (Grand et al, 1996). Thrombin alone was reported to stimulate slightly the synthesis of LTB4 in GM-CSF–primed neutrophils (Palmantier and Borgeat, 1991). Taken together with the fact that active thrombin is not spontaneously present at the onset of an inflammatory reaction, the present study focused on the exact role of platelets on the synthesis of LTB4 upstream to functional thrombin in two different conditions in which platelets can be directly activated by MSUM to release their granule constituents (Ginsberg et al, 1977) and AA (Serhan et al, 1984) or indirectly stimulated through products from fMLP-activated neutrophils (Evangelista et al, 1991; Serhan et al, 1982). Therefore, in our experimental conditions, platelets can strongly inhibit the accumulation of LTB4 synthesized by activated neutrophils (Figs. 1 and 2) despite that more endogenous AA was available through thimerosal (Fig. 1) or GM-CSF (Fig. 2) pretreatment of neutrophils or through MSUM activation of platelets as previously reported (Serhan et al, 1984).
The addition of exogenous AA to our neutrophil-platelet suspensions, although associated with an increase of the output of LTB4, did not reverse the inhibition observed in neutrophil-platelet interactions without AA (Fig. 3). This lends support to an inhibitory effect of platelets on the formation of 5-LOX compounds downstream of PLA2. A possible candidate to the inhibitory effect of platelets on the LTB4 synthesis by neutrophils was adenosine because platelets contain large amounts of adenosine nucleotides (D’Souza and Glueck, 1977) that can be converted to adenosine and this compound suppresses the LTB4 synthesized by neutrophils activated by ligands such as fMLP and PAF (Krump et al, 1996, 1997). The addition of ADA to the platelet-neutrophil suspensions reversed the inhibitory effects of platelets in fMLP-treated cells, confirming that adenosine was the inhibitory product of LTB4 synthesis in these experimental conditions. Adenosine could act through an inhibitory phosphorylation of cPLA2 as reported in smooth muscle cells (Murthy and Makhlouf, 1998), but this mechanism seems unlikely in the present data insofar as addition of exogenous AA did not reverse the platelet inhibition of LTB4 synthesis (Fig. 3). The mechanism of action of adenosine in the present inhibitory effect of platelets on fMLP-stimulated LTB4 synthesis by human neutrophils could be a down-regulation of the translocation of the 5-LO through an elevation of cAMP as recently described (Flamand et al, 2002). In contrast, the addition of ADA had no effect on platelet inhibition of LTB4 synthesis by neutrophils in the presence of MSUM, a solid agonist that, however, has been shown to interact opportunistically with CD16 initially and to transduce signals through CD11b further (Barabe et al, 1998). This persistent inhibition of neutrophil LTB4 synthesis by platelets in the presence of MSUM indicates that adenosine was not responsible for the inhibitory effect and suggests that another platelet product is involved in such an effect. This pattern is reminiscent of (a) a significant inhibition by platelets of the LTB4 synthesis from A23187-stimulated neutrophils (Hosni et al, 1991), of (b) the absence of effect of adenosine on LTB4 synthesis by neutrophils activated by ionophore A23187 as previously reported (Krump et al, 1997), and of (c) the absence of inhibition by adenosine of phospholipase D stimulated by MSUM in human neutrophils (Thibault et al, 2000).
In conclusion, platelets could naturally inhibit the LTB4 synthesis by neutrophils through their spontaneous interactions with these cells. The inhibitory factor can be adenosine as identified in ligand-operated interactions of platelets with neutrophils, but the platelet-derived product responsible for down-regulation of neutrophil lipid mediator release and generation remains to be identified. This could have a significant impact on the homeostatic process of inflammation. In the case of gouty arthritis and/or other crystal-associated diseases, platelet-derived mediators and/or substances that could counter leukocyte activation could be important in the endogenous regulation of continuing bouts of inflammation that distinguish crystal-associated diseases.
Materials and Methods
Reagents
FMLP, rhGM-CSF, and thimerosal were from Sigma Chemical Company (La Verpillière, France). ADA (EC 3.5.4.4., calf intestinal type VIII) was from Sigma Chemical Company (St. Louis, Missouri). ADA was dialyzed against NaCl 0.9% before use. ADA at 0.1 U/ml decreased efficiently the concentration of adenosine within seconds, an effect that persists for up to 30 minutes (Krump et al, 1997). Triclinic crystals MSUM were prepared under sterile pyrogen-free conditions according to the method of McCarty (1965), and the mean sizes of MSUM, as determined by scanning electron microscopy, were 10 × 1.25 μm with a specific area of 6.7 m2/g as previously described (Gaudry et al, 1993). Aspirin, ETYA, and standards used in HPLC were from Cayman (Ann Arbor, Michigan).
Cell Preparation and Incubation
Venous blood from healthy volunteers was collected on citric acid-trisodium citrate-glucose. Platelets were isolated from platelet-rich plasma (Lagarde et al, 1980) and resuspended in Tyrode-HEPES buffer at 550 × 106 cells/ml. Neutrophils were obtained after Dextran sedimentation followed by Ficoll-Paque centrifugation and hypotonic lysis of contaminating erythrocytes. After two washes, neutrophils were resuspended into Tyrode-HEPES buffer at 55 × 106 cells/ml. Platelets remaining in neutrophil suspensions were evaluated by the rosette formation method (Jungi et al, 1986), scored under phase-contrast microscopy after cell fixation in Unopett (Becton and Dickinson), and found at 0.2 to 0.5 platelets/neutrophil. Platelet suspension was placed in 3.5 ml of polypropylene tubes, and neutrophil suspension was added to obtain a platelet/neutrophil ratio of 30/1. Platelet-neutrophil suspensions were preincubated for 5 minutes at 37° C with 1.5 mm CaCl2 and 0.4 mm MgCl2 before stimulation by 1 μm fMLP, or 1 mg/ml MSUM for 5 minutes (fMLP) or 15 minutes (MSUM) at 37° C. Neutrophils stimulated by fMLP were preincubated with 40 μm thimerosal for 30 minutes at room temperature, to increase the availability of AA for 5-LOX by diminishing AA reacylation into phospholipids (Haurand and Flohe, 1989). Neutrophils activated by MSUM were previously primed with 500 μm GM-CSF for 60 minutes at room temperature, to enhance AA release and FLAP expression (DiPersio et al, 1988; Pouliot et al, 1994). For further investigating the mechanism(s) involved in the effect of platelets on 5-LOX activity in neutrophils, platelets were preincubated with ETYA (12-LOX inhibitor) (Salari et al, 1984) and aspirin (COX inhibitor) used at 2 and 200 μm, respectively, for 5 minutes at room temperature. ETYA at 2 μm showed no inhibitory activity on the 5-LOX in neutrophils (data not shown). Graded concentrations of AA were added to incubation media. Finally, in experiments devoted to the possible implication of adenosine in the inhibitory effect of platelets on LTB4 synthesis by neutrophils, 0.1 U/ml ADA was simultaneously added with platelets to neutrophil suspensions.
Incubations were terminated by the addition of methanol (MeOH)-acetonitrile (ACN; 1:1, vol/vol) containing 100 pmol of PGB2 and 15S-hydroxy-8,11-trans-13-cis-eicosatrienoic acid (15-HETrE) as internal standards for RP-HPLC analysis of dihydroxy and monohydroxy derivatives, respectively.
RP-HPLC for AA Metabolites
Supernatants of incubates added with stop solution were directly analyzed without fractionation. AA-derived metabolites were purified and assayed by RP-HPLC as described (Hosni et al, 1991). Briefly, the LiChrospher 100 RP-18 column was isocratically eluted with MeOH/ACN/water/acetic acid (250:300:400:4) at a flow rate of 0.8 ml/min to separate the dihydroxy derivatives (LTB4, Δ6-trans-LTB4, 12-epi-Δ6-trans-LTB4, 20-OH-LTB4, and 5S,12S-diHETE) monitored at 270 nm. Elution times of LTB4 and 5S,12S-diHETE were 26.1 and 27.5 minutes, respectively. Monohydroxy derivatives (5-HETE, 12-HETE) were separated using MeOH/ACN/water/acetic acid (300:450:200:4) at a flow rate of 0.6 ml/min and monitored at 235 nm. Mobile phases had a pH adjusted to 5.6 with 28% (wt/vol) aqueous NH4OH. Quantitation of metabolites was done according to specific densities of each compound with corrections based on internal standards.
Statistical Analysis
Results are expressed in picomoles as mean ± sem of n experiments performed with cells from different donors. Significant differences were statistically evaluated by using the nonparametric Wilcoxon’s paired rank-sum test.
References
Barabe F, Gilbert C, Liao N, Bourgoin SG, and Naccache PH (1998). Crystal-induced neutrophil activation VI. Involvement of FcγRIIIB (CD16) and CD11b in response to inflammatory microcrystals. FASEB J 12: 209–220.
Borgeat P and Samuelsson B (1979). Metabolism of arachidonic acid in polymorphonuclear leukocytes. Structural analysis of novel hydroxylated compounds. J Biol Chem 254: 7865–7869.
Burt HM, Jackson JK, and Rowell J (1989). Calcium pyrophosphate and monosodium urate crystal interactions with neutrophils: Effect of crystal size and lipoprotein binding to crystals. J Rheumatol 16: 809–817.
Carulli G, Barsotti G, Cupisti A, Minnucci S, Gianfaldoni ML, Agostini B, and Ambrogi F (1995). Platelet-neutrophil interactions in uremic patients: Effects on neutrophil superoxide anion production and chemiluminescence. Nephron 69: 248–252.
Chabannes B, Moliere P, Pacheco Y, and Lagarde M (1994). Decreased arachidonic acid metabolism in human platelets by autologous neutrophils: Possible role of cell adhesion. Biochem J 300: 685–691.
Chabannes B, Perraut C, El Habib R, Moliere P, Pacheco Y, and Lagarde M (1997). Correlation between arachidonic acid oxygenation and luminol-induced chemiluminescence in neutrophils: Inhibition by diethyldithiocarbamate. Biochem Pharmacol 53: 927–935.
Colli S, Eligini S, Lalli M, and Tremoli E (1996). Platelet-neutrophil interaction and superoxide anion generation: Involvement of purine nucleotides. Free Radic Biol Med 20: 271–278.
Cronstein BN (1994). Adenosine, an endogenous anti-inflammatory agent. J Appl Physiol 76: 5–13.
Dieppe P, Hornby J, Swan A, Hutton C, and Preece A (1983). Laboratory handling of crystals. Ann Rheum Dis 42 (Suppl 1): 60–63.
DiPersio JF, Billing P, Williams R, and Gasson JC (1988). Human granulocyte-macrophage colony-stimulating factor and other cytokines prime human neutrophils for enhanced arachidonic acid release and leukotriene B4 synthesis. J Immunol 140: 4315–4322.
D’Souza L and Glueck HI (1977). Measurement of nucleotide pools in platelets using high pressure liquid chromatography. Thromb Haemost 38: 990–1001.
Evangelista V, Celardo A, Dell’Elba G, Manarini S, Mironov A, de Gaetano G, and Cerletti C (1999). Platelet contribution to leukotriene production in inflammation: In vivo evidence in the rabbit. Thromb Haemost 81: 442–448.
Evangelista V, Rajtar G, de Gaetano G, White JG, and Cerletti C (1991). Platelet activation by fMLP-stimulated polymorphonuclear leukocytes: The activity of cathepsin G is not prevented by antiproteinases. Blood 77: 2379–2388.
Fam AG, Schumacher HR Jr, Clayburne G, Sieck M, Mandel NS, Cheng PT, and Pritzker KP (1992). A comparison of five preparations of synthetic monosodium urate monohydrate crystals. J Rheumatol 19: 780–787.
Flamand N, Surette ME, Picard S, Bourgoin S, and Borgeat P (2002). Cyclic AMP-mediated inhibition of 5-lipoxygenase translocation and leukotriene biosynthesis in human neutrophils. Mol Pharmacol 62: 250–256.
Ford-Hutchinson AW (1990). Leukotriene B4 in inflammation. Crit Rev Immunol 10: 1–12.
Gaudry M, Roberge CJ, de Medicis R, Lussier A, Poubelle PE, and Naccache PH (1993). Crystal-induced neutrophil activation. III. Inflammatory microcrystals induce a distinct pattern of tyrosine phosphorylation in human neutrophils. J Clin Invest 91: 1649–1655.
Ginsberg MH, Kozin F, O’Malley M, and McCarty DJ (1977). Release of platelet constituents by monosodium urate crystals. J Clin Invest 60: 999–1007.
Ginsburg I and Quie PG (1980). Modulation of human polymorphonuclear leukocyte chemotaxis by leukocyte extracts, bacterial products, inflammatory exudates, and polyelectrolytes. Inflammation 4: 301–311.
Goppelt-Struebe M, Koerner CF, Hausmann G, Gemsa D, and Resch K (1986). Control of prostanoid synthesis: Role of reincorporation of released precursor fatty acids. Prostaglandins 32: 373–385.
Grand RJ, Turnell AS, and Grabham PW (1996). Cellular consequences of thrombin-receptor activation. Biochem J 313 (Pt 2):353–368.
Haurand M and Flohe L (1989). Leukotriene formation by human polymorphonuclear leukocytes from endogenous arachidonate. Physiological triggers and modulation by prostanoids. Biochem Pharmacol 38: 2129–2137.
Henderson WR Jr (1994). The role of leukotrienes in inflammation. Ann Intern Med 121: 684–697.
Hoover RL, Karnovsky MJ, Austen KF, Corey EJ, and Lewis RA (1984). Leukotriene B4 action on endothelium mediates augmented neutrophil/endothelial adhesion. Proc Natl Acad Sci USA 81: 2191–2193.
Hosni R, Chabannes B, Pacheco Y, Moliere P, Grosclaude M, Perrin Fayolle M, and Lagarde M (1991). Leukotriene B4 levels from stimulated neutrophils from healthy and allergic subjects: Effect of platelets and exogenous arachidonic acid. Eur J Clin Invest 21: 631–637.
Issekutz AC, Ripley M, and Jackson JR (1983). Role of neutrophils in the deposition of platelets during acute inflammation. Lab Invest 49: 716–724.
Jungi TW, Spycher MO, Nydegger UE, and Barandun S (1986). Platelet-leukocyte interaction: Selective binding of thrombin-stimulated platelets to human monocytes, polymorphonuclear leukocytes, and related cell lines. Blood 67: 629–636.
Kanaji K, Okuma M, and Uchino H (1986). Deficient induction of leukotriene synthesis in human neutrophils by lipoxygenase-deficient platelets. Blood 67: 903–908.
Kjeldsberg CR and Swanson J (1974). Platelet satellitism. Blood 43: 831–836.
Krump E, Lemay G, and Borgeat P (1996). Adenosine A2 receptor-induced inhibition of leukotriene B4 synthesis in whole blood ex vivo. Br J Pharmacol 117: 1639–1644.
Krump E, Picard S, Mancini J, and Borgeat P (1997). Suppression of leukotriene B4 biosynthesis by endogenous adenosine in ligand-activated human neutrophils. J Exp Med 186: 1401–1406.
Lagarde M, Bryon PA, Guichardant M, and Dechavanne M (1980). A simple and efficient method for platelet isolation from their plasma. Thromb Res 17: 581–588.
Larsen E, Celi A, Gilbert GE, Furie BC, Erban JK, Bonfanti R, Wagner DD, and Furie B (1989). PADGEM protein: A receptor that mediates the interaction of activated platelets with neutrophils and monocytes. Cell 59: 305–312.
Levine JD, Lau W, Kwiat G, and Goetzl EJ (1984). Leukotriene B4 produces hyperalgesia that is dependent on polymorphonuclear leukocytes. Science 225: 743–745.
Maclouf J, de Laclos BF, and Borgeat P (1982). Stimulation of leukotriene biosynthesis in human blood leukocytes by platelet-derived 12-hydroperoxy-icosatetraenoic acid. Proc Natl Acad Sci USA 79: 6042–6046.
Maclouf J, Fitzpatrick FA, and Murphy RC (1989). Transcellular biosynthesis of eicosanoids. Pharmacol Res 21: 1–7.
Maderna P, Colli S, Caruso D, Eligini S, Toia A, Galli G, and Tremoli E (1993). Quantitative changes of hydroxyacid formation during platelet-neutrophil interaction. J Lab Clin Med 121: 406–414.
Marcus AJ, Broekman MJ, Safier LB, Ullman HL, Islam N, Sherhan CN, Rutherford LE, Korchak HM, and Weissmann G (1982). Formation of leukotrienes and other hydroxy acids during platelet-neutrophil interactions in vitro. Biochem Biophys Res Commun 109: 130–137.
Marcus AJ, Broekman MJ, Safier LB, Ullman HL, Islam N, Serhan CN, and Weissmann G (1984). Production of arachidonic acid lipoxygenase products during platelet-neutrophil interactions. Clin Physiol Biochem 2: 78–83.
McCarty DJ Jr (1965). The inflammatory reaction to microcrystalline sodium urate. Arthritis Rheum 8: 726–735.
McCulloch RK, Croft KD, and Vandongen R (1992). Enhancement of platelet 12-HETE production in the presence of polymorphonuclear leukocytes during calcium ionophore stimulation. Biochim Biophys Acta 1133: 142–146.
McGarrity ST, Hyers TM, and Webster RO (1988). Inhibition of neutrophil functions by platelets and platelet-derived products: Description of multiple inhibitory properties. J Leukoc Biol 44: 93–100.
Murthy KS and Makhlouf GM (1998). Differential regulation of phospholipase A2 (PLA2)-dependent Ca2+ signaling in smooth muscle by cAMP- and cGMP-dependent protein kinases. Inhibitory phosphorylation of PLA2 by cyclic nucleotide-dependent protein kinases. J Biol Chem 273: 34519–34526.
Naccache PH, Bourgoin S, Plante E, Roberge CJ, de Medicis R, Lussier A, and Poubelle PE (1993). Crystal-induced neutrophil activation. II. Evidence for the activation of a phosphatidylcholine-specific phospholipase D. Arthritis Rheum 36: 117–125.
Naccache PH, Grimard M, Roberge CJ, Gilbert C, Lussier A, de Medicis R, and Poubelle PE (1991). Crystal-induced neutrophil activation. I. Initiation and modulation of calcium mobilization and superoxide production by microcrystals. Arthritis Rheum 34: 333–342.
Palmantier R and Borgeat P (1991). Thrombin-activated platelets promote leukotriene B4 synthesis in polymorphonuclear leucocytes stimulated by physiological agonists. Br J Pharmacol 103: 1909–1916.
Peters MJ, Heyderman RS, Hatch DJ, and Klein NJ (1997). Investigation of platelet-neutrophil interactions in whole blood by flow cytometry. J Immunol Methods 209: 125–135.
Poubelle PE and Borgeat P (2002). Platelet interactions with other cells related to inflammatory diseases. In: Gresele P, Page CP, Fuster V, Vermylen J, editors. Platelets in thrombotic and non-thrombotic disorders: Pathophysiology, pharmacology and therapeutics. Cambridge, UK: Cambridge University Press, 869–884.
Poubelle PE, Bourgoin S, Naccache PH, and Borgeat P (1989). Granulocyte-macrophage colony-stimulating factor (GM-CSF) and opsonization synergistically enhance leukotriene B4 (LTB4) synthesis induced by phagocytosis in human neutrophils. Agents Actions 27: 388–390.
Poubelle PE, Stankova J, Grassi J, and Rola-Pleszczynski M (1991). Leukotriene B4 up-regulates IL-6 rather than IL-1 synthesis in human monocytes. Agents Actions 34: 42–45.
Pouliot M, McDonald PP, Borgeat P, and McColl SR (1994). Granulocyte/macrophage colony-stimulating factor stimulates the expression of the 5-lipoxygenase-activating protein (FLAP) in human neutrophils. J Exp Med 179: 1225–1232.
Radmark O, Shimizu T, Jornvall H, and Samuelsson B (1984). Leukotriene A4 hydrolase in human leukocytes. Purification and properties. J Biol Chem 259: 12339–12345.
Rinder HM, Bonan JL, Rinder CS, Ault KA, and Smith BR (1991). Dynamics of leukocyte-platelet adhesion in whole blood. Blood 78: 1730–1737.
Rouzer CA, Shimizu T, and Samuelsson B (1985). On the nature of the 5-lipoxygenase reaction in human leukocytes: Characterization of a membrane-associated stimulatory factor. Proc Natl Acad Sci USA 82: 7505–7509.
Salari H, Braquet P, and Borgeat P (1984). Comparative effects of indomethacin, acetylenic acids, 15-HETE, nordihydroguaiaretic acid and BW755C on the metabolism of arachidonic acid in human leukocytes and platelets. Prostaglandins Leukot Med 13: 53–60.
Schumacher HR, Fishbein P, Phelps P, Tse R, and Krauser R (1975). Comparison of sodium urate and calcium pyrophosphate crystal phagocytosis by polymorphonuclear leukocytes. Effects of crystal size and other factors. Arthritis Rheum 18: 783–792.
Serhan CN, Broekman MJ, Korchak HM, Marcus AJ, and Weissmann G (1982). Endogenous phospholipid metabolism in stimulated neutrophils differential activation by FMLP and PMA. Biochem Biophys Res Commun 107: 951–958.
Serhan CN, Lundberg U, Weissmann G, and Samuelsson B (1984). Formation of leukotrienes and hydroxy acids by human neutrophils and platelets exposed to monosodium urate. Prostaglandins 27: 563–581.
Serhan CN and Sheppard KA (1990). Lipoxin formation during human neutrophil-platelet interactions. Evidence for the transformation of leukotriene A4 by platelet 12-lipoxygenase in vitro. J Clin Invest 85: 772–780.
Sha’afi RI, Naccache PH, Molski TF, Borgeat P, and Goetzl EJ (1981). Cellular regulatory role of leukotriene B4: Its effects on cation homeostasis in rabbit neutrophils. J Cell Physiol 108: 401–408.
Spangenberg P, Redlich H, Bergmann I, Losche W, Gotzrath M, and Kehrel B (1993). The platelet glycoprotein IIb/IIIa complex is involved in the adhesion of activated platelets to leukocytes. Thromb Haemost 70: 514–521.
Thibault N, Harbour D, Borgeat P, Naccache PH, and Bourgoin SG (2000). Adenosine receptor occupancy suppresses chemoattractant-induced phospholipase D activity by diminishing membrane recruitment of small GTPases. Blood 95: 519–527.
Weksler BB (1983). Platelets and the inflammatory response. Clin Lab Med 3: 667–676.
Acknowledgements
This work was supported by INSERM (France), the Région Rhône-Alpes, the FRSQ (Québec, Canada) via a Programme de Coopération (no 980971) and the Université Laval (sabbatical year to PEP).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chabannes, B., Poubelle, P., Molière, P. et al. Platelets Abrogate Leukotriene B4 Generation by Human Blood Neutrophils Stimulated with Monosodium Urate Monohydrate or f-Met-Leu-Phe In Vitro. Lab Invest 83, 491–499 (2003). https://doi.org/10.1097/01.LAB.0000062855.90029.D8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1097/01.LAB.0000062855.90029.D8