Abstract
Introduction:
As survival and long-term morbidity of very preterm infants have improved over the past decade, the limits of infant viability, the level of maturity below which survival and/or acceptable neurodevelopmental outcome are extremely unlikely, have also decreased.
Study Design:
In an effort to define the current limits of infant viability, the data in the literature on survival and long-term neurodevelopmental outcome in very preterm neonates have been reviewed.
Result:
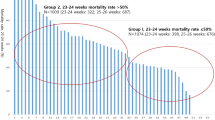
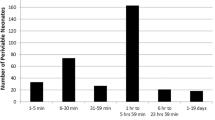
The gestational age and birth weight below which infants are too immature to survive, and thus provision of intensive care is unreasonable, appears to be at <23 weeks and <500 g, respectively. Infants born at ⩾25 weeks' gestation and with a birth weight of ⩾600 g are mature enough to warrant initiation of intensive care, as the majority of these patients survive, and at least 50% do so without severe long-term disabilities. Finally, for infants born between 230/7 and 246/7 weeks' gestation and with a birth weight of 500 to 599 g, survival and outcome are extremely uncertain. For these infants born in the so-called ‘gray zone’ of infant viability, the line between patient autonomy and medical futility is blurred, and medical decision-making becomes even more complex and needs to embrace careful consideration of several factors. These factors include appraisal of prenatal data and the information obtained during consultations with the parents before delivery; evaluation of the patient's gestational age, birth weight and clinical condition upon delivery; ongoing reassessment of the patient's response to resuscitation and intensive care and continued involvement of the parents in the decision-making process after delivery.
Conclusion:
Based on these findings an algorithm is offered for consideration for neonatologists managing infants born in the ‘gray zone’ of infant viability. However, caution must be exercised when one considers incorporating this guideline into clinical practice because the algorithm is based on the analysis of the findings in the literature and the authors' experience rather than direct evidence.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
The Victorian Infant Collaborative Study Group. Outcome at 2 years of children 23–27 weeks' gestation born in Victoria in 1991–1992. J Paediatr Child Health 1997; 33: 161–165.
Batton DG, De Witte DB, Espinosa R, Swails TL . The impact of fetal compromise on outcome at the border of viability. Am J Obstet Gynecol 1998; 178: 909–915.
Draper ES, Manktelow B, Field DJ, James D . Prediction of survival for preterm births by weight and gestational age: retrospective population based study. BMJ 1999; 319: 1093–1097.
Lorenz JM . Survival of the extremely preterm infant in North America in the 1990s. Clin Perinatol 2000; 27: 255–262.
El-Metwally D, Vohr B, Tucker R . Survival and neonatal morbidity at the limits of viability in the mid 1990s: 22–25 weeks. J Pediatr 2000; 137: 616–622.
Wood NS, Marlow N, Costeloe K, Gibson AT, Wilkinson AR . Neurologic and developmental disability after extremely preterm birth. EPICure Study Group. N Engl J Med 2000; 343: 378–384.
Lorenz JM . The outcome of extreme prematurity. Semin Perinatol 2001; 25: 25348–25359.
Doyle LW, the Victorian Infant Collaborative Study Group. Neonatal intensive care at borderline viability—is it worth it? E Hum Develop 2004; 80: 103–113.
Kaiser JR, Tilford JM, Simpson PM, Salhab WA, Rosenfeld CR . Hospital survival of very-low-birth-weight neonates from 1977 to 2000. J Perinatol 2004; 24: 343–350.
Marlow N, Wolke D, Bracewell MA, Samara M, the EPICure Study Group. Neurologic and developmental disability at six years of age after extremely preterm birth. N Engl J Med 2005; 352: 71–72.
Chervenak FA, McCullough LB, Levene MI . An ethically justified, clinically comprehensive approach to peri-viability: gynecological, obstetric, perinatal and neonatal dimensions. J Obstet Gynaecol 2007; 27: 3–7.
Singh J, Fanaroff J, Andrews B, Caldarelli L, Lagatta J, Plesha-Troyke S et al. Resuscitation in the gray zone of viability: determining physician preferences and predicting infant outcomes. Pediatrics 2007; 120: 519–526.
Lantos JD, Meadow WL . Neonatal Bioethics: The Moral Challenges of Medical Innovation. Johns Hopkins University Press: Baltimore, MD, 2006.
Vohr BR, Wright LL, Dusick AM, Mele L, Verter J, Steichen JJ et al. Neurodevelopmental and functional outcomes of extremely low birth weight infants in the National Institute of Child Health and Human Development Research Network 1993–1994. Pediatrics 2000; 105: 1216–1226.
Hack M, Fanaroff AA . Outcomes of children of extremely low-birth weight premature infants in the 1990s. Early Hum Dev 1999; 53: 195–218.
Mestan KK, Marks JD, Hecox K, Huo D, Schreiber MD . Neurodevelopmental outcomes of premature infants treated with inhaled nitric oxide. N Engl J Med 2005; 353: 23–32.
Schreiber MD, Gin-Mestan K, Marks JD, Huo D, Lee G, Srisuparp P . Inhaled nitric oxide in premature infants with the respiratory distress syndrome. N Engl J Med 2003; 349: 2099–2107.
Allen MC, Donohue PK, Dusman AE . The limit of viability—neonatal outcome of infants born at 22–25 weeks' gestation. N Engl J Med 1993; 329: 1597–1601.
Markestad T, Kaaresen PI, Rønnestad A, Reigstad H, Lossius K, Medbø S et al. Early death, morbidity and need of treatment among extremely premature infants. Pediatrics 2005; 115: 1289–1298.
Walther FJ . Withholding treatment, withdrawing treatment, and palliative care in the neonatal intensive care unit. Early Hum Dev 2005; 81: 965–972.
Lucey JF, Rowan CA, Shiono P, Wilkinson AR, Kilpatrick S, Payne NR et al. Fetal infants: the fate of 4172 infants with birth weights of 401–500 grams—the Vermont Oxford Network experience (1996–2000). Pediatrics 2004; 113: 1559–1566.
Serenella-Pignotti M, Donzelli G . Perinatal care at the threshold of viability: an international comparison of practical guidelines for the treatment of extremely preterm births. Pediatrics 2008; 121: e193–e198.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure
This paper was supported by a grant from Dey, L.P. Dr. Seri is on the scientific advisory board for Dey, L.P. Dr. Evans has received consulting fees from Discovery Labs and lecture fees from NO Therapeutics.
Rights and permissions
About this article
Cite this article
Seri, I., Evans, J. Limits of viability: definition of the gray zone. J Perinatol 28 (Suppl 1), S4–S8 (2008). https://doi.org/10.1038/jp.2008.42
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2008.42
Keywords
This article is cited by
-
Adverse Pregnancy Outcomes Following the Assassination of John F. Kennedy in 1963
Maternal and Child Health Journal (2021)
-
Joint periviability counseling between neonatology and obstetrics is a rare occurrence
Journal of Perinatology (2020)
-
Challenging the gestational age for the limit of viability: proactive care
Journal of Perinatology (2019)
-
Placental abruption and hemorrhage—review of imaging appearance
Emergency Radiology (2019)
-
Prospective study of early and late outcomes of extremely low birthweight in Central Saudi Arabia
BMC Pediatrics (2018)