Abstract
INTRODUCTION:
Traditional cardiovascular risk factors such as central obesity, high blood pressure and insulin resistance, all constituents of metabolic syndrome, have been associated with increased levels of C-reactive protein (CRP). Therefore, this marker of low-grade inflammation may play a major role in the pathogenesis of cardiovascular diseases. In this study, data from a representative sample of urban adults was used to evaluate the association between CRP and metabolic syndrome, accounting for the type and number of its constituents.
METHODS:
Using random digit dialing, 1022 participants, aged 18–92 y, were selected. All participants completed a structured questionnaire comprising of information on social, demographic, behavioral and clinical aspects. Anthropometrics and blood pressure were recorded and a fasting blood sample collected. Metabolic syndrome was defined, according to the Third Report of the Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults, as the presence of three or more of the following characteristics: waist circumference greater than 102 cm in men and 88 cm in women; triglyceride levels ≥150 mg/dl; high-density lipoprotein cholesterol levels <40 mg/dl in men and <50 mg/dl in women; blood pressure ≥130/85 mm Hg; and serum glucose ≥110 mg/dl. High-sensitivity CRP was assessed by immunonephelometric assay. After excluding 65 participants with CRP ≥10 mg/l, 957 subjects (599 women and 358 men) remained for analysis. Geometric means were compared after adjustment for age, sex, alcohol consumption and smoking.
RESULTS:
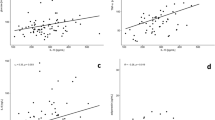
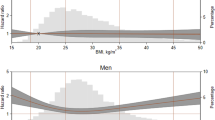
Higher mean levels of CRP (2.34 vs 1.36, P<0.001) were observed when metabolic syndrome was present. Also, mean CRP levels were significantly higher in the presence of central obesity (2.45 vs 1.24, P<0.001), high blood pressure (1.76 vs 1.12, P<0.001), hypertriglyceridemia (2.17 vs 1.32, P<0.001) and high fasting glucose (1.96 vs 1.46, P=0.032). We found a significant increasing trend (P<0.001) in mean levels of CRP as the number of features of metabolic syndrome increased. The major contributing features for high CRP levels were central obesity and high blood pressure.
CONCLUSIONS:
Present data show that increasing severity of metabolic syndrome is associated with increasing CRP. Additionally, we found that central obesity and high blood pressure are the most important determinants of the low-grade chronic inflammation present in metabolic syndrome.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Alberti K, Zimmet P . Definition, diagnosis and classification of diabetes mellitus and its complications. Part I: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabetes Med 1998; 15: 539–553.
Festa A, D'Agostino R, Howard G, Mykkänen L, Tracy R, Haffner S . Chronic subclinical inflammation as part of the insulin resistance syndrome. The Insulin Resistance Atherosclerosis Study (IRAS). Circulation 2000; 102: 42–47.
Ford E . The metabolic syndrome and C-reactive protein, fibrinogen, and leucocyte count: findings from the Third National Health and Nutrition Examination Survey. Atherosclerosis 2003; 168: 351–358.
Marques-Vidal P, Mazoyer E, Bongard V, Gourdy P, Ruidavets J, Drouet L, Ferrières J . Prevalence of insulin resistance syndrome in southwestern France and its relationship with inflammatory and hemostatic markers. Diabetes Care 2002; 25: 1371–1377.
Sattar N, Gaw A, Scherbakova O, Ford I, O'Reilly D, Haffner S, Isles C, Macfarlane PW, Packard CJ, Cobbe SM, Shepherd J . Metabolic syndrome with and without C-reactive protein as a predictor of coronary heart disease and diabetes in the West of Scotland Coronary Prevention Study. Circulation 2003; 108: 414–419.
Han T, Sattar N, Williams K, Gonzalez-Villalpando C, Lean M, Haffner S . Prospective study of C-reactive protein in relation to the development of diabetes and metabolic syndrome in the Mexico City Diabetes Study. Diabetes Care 2002; 25: 2016–2021.
Ridker P, Buring J, Cook N, Rifai N . C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events. An 8-year follow-up of 14 719 initially healthy American women. Circulation 2003; 107: 391–397.
Yudkin J, Stehouwer C, Emeis J, Coppack S . C-reactive protein in healthy subjects: associations with obesity, insulin resistance, and endothelial dysfunction. A potential role for cytokines originating from adipose tissue? Arterioscler Thromb Vasc Biol 1999; 19: 972–978.
Hak A, Stehouer C, Bots M, Polderman K, Schalkwijk C, Westendorp I, Hofman A, Witteman JCM . Associations of C-reactive protein with measures of obesity, insulin resistance, and subclinical atherosclerosis in healthy, middle-aged women. Arterioscler Thromb Vasc Biol 1999; 19: 1986–1991.
Fröhlich M, Imhof A, Berg G, Hutchinson W, Pepys M, Boeing H, Muche R, Brenner H, Koenig W . Association between C-reactive protein and features of the metabolic syndrome. A population-based study. Diabetes Care 2000; 23: 1835–1839.
Shen B, Todaro J, Niaura R, McCaffery J, Zhang J, Spiro III A, Ward KD . Are metabolic risk factors one unified syndrome? Modeling the structure of the metabolic syndrome X. Am J Epidemiol 2003; 157: 701–711.
Meigs J . Insulin Resistance Syndrome? Multiple Metabolic Syndrome? A Syndrome at all? Factor analysis reveals patterns in the fabric of correlated metabolic risk factors. Am J Epidemiol 2000; 152: 908–911.
Sesso H, Buring J, Rifai N, Blake G, Gaziano J, Ridker P . C-reactive protein and the risk of developing hypertension. JAMA 2003; 290: 2945–2951.
Pearson T, Mensah G, Alexander R, Anderson J, Cannon III R, Criqui M, Fadl YY, Fortmann SP, Hong Y, Myers GL, Rifai N, Smith SC, Taubert K, Tracy RP, Vinicor F . Markers of inflammation and cardiovascular disease. Application to clinical and public health practice. A statement for health care professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 2003; 107: 499–511.
Ridker P . Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation 2003; 107: 363–369.
Yeh E, Willerson J . Coming of age C-reactive protein. Using inflammation markers in cardiology. Circulation 2003; 107: 370–372.
Ridker P, Cushman M, Stampfer M, Tracy R, Hennekens C . Inflammation, aspirin, and risk of cardiovascular disease in apparently healthy men. N Engl J Med 1997; 336: 973–979.
Koenig W, Sund M, Frohlich M, Fischer HG, Lowel H, Doring A, Hutchinson WL, Pepys MB . C-reactive protein, a sensitive marker of inflammation, predicts future risk of coronary heart disease in initially healthy middle-aged men: results from the MONICA (Monitoring Trends and Determinants in Cardiovascular Disease) Augsburg Cohort Study, 1984–1992. Circulation 1999; 99: 237–242.
Witherell H, Smith K, Friedman G, Ley C, Thom D, Orentreich N, Vogelman JH, Parsonnet J . C-reactive protein, Helicobacter pylori, Chlamydia pneumoniae, cytomegalovirus and risk for myocardial infarction. Ann Epidemiol 2003; 13: 170–177.
Ridker P, Glynn R, Hennekens C . C-reactive protein adds to the predictive value of total and HDL cholesterol in determining risk of first myocardial infarction. Circulation 1998; 97: 2007–2011.
Ridker P, Hennekens C, Buring J, Rifai N . C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med 2000; 342: 836–843.
Ridker P, Rifai N, Pfeffer M, Sacks F, Moye L, Goldman S, Flaker GC, Braunwald E, Cholesterol and Recurrent Events (CARE) Investigators. Inflammation, pravastatin, and the risk of coronary events after myocardial infarction in patients with average cholesterol levels. Circulation 1998; 98: 839–844.
Lopes C . Diet and Myocardial Infarction: A Community-Based Case–Control Study. [PhD]. University of Porto: Porto; 2000.
Ramos E, Lopes C, Barros H . Investigating the effect of nonparticipation using a population-based case–control study on myocardial infarction. Ann Epidemiol 2004; 14: 437–441.
Folstein M, Folstein S, Mchush P . Mini mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiat Res 1975; 12: 189–198.
Perloff D, Grim C, Flack J, Frohlich ED, Hill M, McDonald M, Morgenstern BZ . Human blood pressure determination by sphygmomanometry. Circulation 1993; 88: 2460–2470.
Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001; 285: 2486–2497.
Lagrand W, Visser C, Hermens W, Niessen H, Verheugt F, Wolbink G, Hack CE . C-reactive protein as a cardiovascular risk factor. More than an epiphenomenon? Circulation 1999; 100: 96–102.
Burke A, Tracy R, Kolodgie F, Malcom G, Zieske A, Kutys R, Pestaner J, Smialek J, Virmani R . Elevated C-reactive protein values and atherosclerosis in sudden coronary death. Association with different pathologies. Circulation 2002; 105: 2019–2023.
Blake G, Ridker P . C-reactive protein, subclinical atherosclerosis, and risk of cardiovascular events. Arterioscler Thromb Vasc Biol 2002; 22: 1512–1513.
Yasojima K, Schwab C, McGeer EG, McGeer PL . Generation of C-reactive protein and complement components in atherosclerotic plaques. Am J Pathol 2001; 158: 1039–1051.
Ridker PM, Rifai N, Pfeffer MA, Sacks F, Braunwald E . Long-term effects of pravastatin on plasma concentration of C-reactive protein. The Cholesterol and Recurrent Events (CARE) Investigators. Circulation 1999; 100: 230–235.
Danesh J, Collins R, Appleby P, Peto R . Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease. Meta -analyses of prospective studies. JAMA 1998; 279: 1477–1482.
Das U . Is obesity an inflammatory condition? Nutrition 2001; 17: 953–966.
Santos A, Lopes C, Barros H . Prevalence of metabolic syndrome in the city of Porto. Rev Port Cardiol 2004; 23: 45–52.
McLaughlin T, Abbasi F, Lamendola C, Liang L, Reaven G, Schaaf P, Reaven P . Differentiation between obesity and insulin resistance in the association with C-reactive protein. Circulation 2002; 106: 2908–2912.
Daniels SR . Cardiovascular disease risk factors and atherosclerosis in children and adolescents. Curr Atheroscler Rep 2001; 3: 479–485.
Imhof A, Fröhlich M, Brenner H, Boeing H, Pepys M, Koenig W . Effect of alcohol consumption on systemic markers of inflammation. Lancet 2001; 357: 763–767.
Albert M, Glynn R, Ridker P . Alcohol consumption and plasma concentration of C-reactive protein. Circulation 2003; 107: 443–447.
Grundy S, Hansen B, Smith S, Cleeman J, Kahn R . Clinical management of metabolic syndrome. Report of the American Heart Association/National Heart, Lung, and Blood Institute/American Diabetes Association Conference on Scientific Issues Related to Management. Circulation 2004; 109: 551–556.
Acknowledgements
This study was funded by the Fundação para a Ciência e Tecnologia, Praxis 2/2.1/SAU/1332/95, POCTI/ESP/35767/99 and POCTI/ESP/42361/2001.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Santos, AC., Lopes, C., Guimarães, J. et al. Central obesity as a major determinant of increased high-sensitivity C-reactive protein in metabolic syndrome. Int J Obes 29, 1452–1456 (2005). https://doi.org/10.1038/sj.ijo.0803035
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0803035
Keywords
This article is cited by
-
Serum levels of vitamin D, retinol, zinc, and CRP in relation to obesity among children and adolescents
European Journal of Medical Research (2022)
-
Clinical and biological risk factors associated with inflammation in patients with type 2 diabetes mellitus
BMC Endocrine Disorders (2022)
-
Pericardial fat, thoracic peri-aortic adipose tissue, and systemic inflammatory marker in nonalcoholic fatty liver and abdominal obesity phenotype
Scientific Reports (2022)
-
Obesity and cardiovascular disease in women
International Journal of Obesity (2020)
-
Impact of a Formulation Containing Unusual Polyunsaturated Fatty Acids, Trace Elements, Polyphenols and Plant Sterols on Insulin Resistance and Associated Disturbances
Diabetes Therapy (2020)