Abstract
OBJECTIVE: The frequently observed U-shaped relationship between body mass index (BMI; kg/m2) and mortality rate may be due to the opposing effects of fat mass (FM) and fat-free mass (FFM) components of BMI on mortality rate. The purpose is to test the hypothesis stated above.
DESIGN: Longitudinal prospective cohort studies. The mortality follow-up of the first and second National Health and Nutrition Examination Surveys (NHANES I and NHANES II).
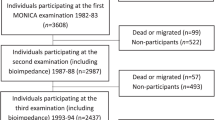
SUBJECTS: A total of 10 169 male subjects aged 25–75 who participated in NHANES I and II were selected for analyses. Follow-up continued until 1992. The mean follow-up time was 14.6 y for NHANES I and 12.9 y for NHANES II. Ninety-eight percent of the participants were successfully followed representing a total of 3722 deaths.
MEASUREMENTS: Subscapular and triceps skinfolds thickness were used as FM indicators, whereas upper arm circumference was used as a FFM indicator. The Cox proportional hazards model tested the relationships of BMI, FM and FFM with all-cause mortality adjusting for age, smoking status, race and education levels.
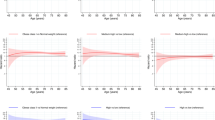
RESULTS: BMI had a U-shaped relationship with mortality, with a nadir of approximately 27 kg/m2. However, when indicators of FM and FFM were added to the model, the relationship between BMI and mortality became more nearly monotonic increasing. Moreover, the relationship between FM indicator and mortality was monotonic increasing and the relationship between FFM indicator and mortality was monotonic decreasing.
CONCLUSION: These results support the hypothesis that the apparently deleterious effects of marked thinness may be due to low FFM and that, over the observed range of the data, marked leanness (as opposed to thinness) has beneficial effects.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Troiano RP, Frongillo EA Jr, Sobal J, Levitsky DA . The relationship of body weight and mortality: a quantitative analysis of combined information from existing studies Int J Obes Relat Metab Disord 1996 20: 63–75.
Allison DB, Saunders SE . Obesity in North America: an overview Med Clin N Am 2000 84: 305–332.
Manson JE, Stampfer MJ, Hennekens CH, Willett WC . Body weight and longevity: a reassessment JAMA 1987 257: 353–358.
Manson JE, Willett WC, Stampfer MJ, Colditz GA, Hunter DJ, Hankinson SE, Hennekens CH, Speizer FE . Body weight and mortality among women New Engl J Med 1995 333: 677–685.
Stevens J, Cai J, Pamuk ER, Williamson DF, Thun MJ, Wood JL . The effect of age on the association between body-mass index and mortality New Engl J Med 1998 338: 1–7.
The BMI in Diverse Populations Collaborative Group . Effect of smoking on the body mass index-mortality relation: empirical evidence from 15 studies Am J Epidemiol 1999 150: 1297–1308.
Goldstein DJ . Beneficial effects of modest weight loss Int J Obes Relat Metab Disord 1992 16: 397–415.
McCarter RJ . Role of caloric restriction in the prolongation of life Clin Geriatr Med 1995 11: 553–565.
Allison DB, Faith MS, Heo M, Kotler DP . Hypothesis concerning the U-shaped relation between body mass index and mortality Am J Epidemiol 1997 146: 339–349.
Comstock GW, Kendrick MA, Livesay VT . Subcutaneous fatness and mortality Am J Epidemiol 1966 83: 548–563.
Keys A, Taylor HL, Blackburn H, Brozek J, Anderson T, Simonson E . Mortality and coronary heart disease among men studied for 23 y Arch Intern Med 1971 128: 201–214.
Menotti A, Descovich GC, Lanti M, Spagnolo A, Dormi A, Seccareccia F . Indexes of obesity and all-causes mortality in Italian epidemiological data Prev Med 1993 22: 293–303.
Blair SN, Brodney S . Effects of physical inactivity and obesity on morbidity and mortality: current evidence and research issues Med Sci Sports Exerc 1999 31(Suppl): 646–662.
Kalmijn S, Curb JD, Rodriguez BL, Yano K, Abbott RD . The association of body weight and anthropometry with mortality in elderly men: the Honolulu Heart Program Int J Obes Relat Metab Disord 1999 23: 395–402.
Heitmann BL, Erikson H, Ellsinger BM, Mikkelsen KL, Larsson B . Mortality associated with body fat, fat-free mass and body mass index among 60-year-old Swedish men—a 22-year follow-up. The study of men born in 1913 Int J Obes Relat Metab Disord 2000 24: 33–37.
Lee CD, Blair SN, Jackson AS . Cardiorespiratory fitness, body composition, and all-cause and cardiovascular disease mortality in men Am J Clin Nutr 1999 69: 373–380.
Goran MI, Allison DB, Poehlman ET . Issues relating to normalization of body fat content in men and women Int J Obes Relat Metab Disord 1995 19: 638–643.
Vague J . Les Obesities Etude Biometrique Biol Med 1947 36: 1.
Tuljapurkar S, Li N, Boe C . A universal pattern of mortality decline in the G7 countries Nature 2000 405: 789–792.
Cornoni-Huntley J, Harris T, Everett D, Albanes D, Micozzi MS, Miles TP, Feldman JJ . An overview of body weight of older persons, including the impact on mortality. The National Health and Nutrition Examination Survey I—Epidemiologic Follow-up Study J Clin Epidemiol 1991 44: 743–753.
Freedman D, Williamson D, Croft J, Byers T . Relation of body fat distribution to ischemic heart disease. The NHANES I Epidemiologic Follow-up Study Am J Epidemiol 1995 142: 53–63.
Department of Health and Human Services NCHS . Plan and operation of the second National Health and Nutrition Examination Survey 1976–1980. Vital and Health Statistics Series 1, Vol 15 DHHS Publication No. (PHS) 81-1317 US Government Printing Office: Washington, DC 1981.
Department of Health and Human Services NCHS . Plan and operation of the NHANES I Epidemiologic Followup Study, 1987. Vital and Health Statistics Series 1, Vol 27, DHHS publication no. (PHS) 92–1303 National Center for Health Statistics, 1992.
Allison DB, Heo M, Flanders DW, Faith MS, Williamson DF . Examination of ‘early mortality exclusion’ as an approach to control for confounding by occult disease in epidemiologic studies of mortality risk factors Am J Epidemiol 1997 146: 672–680.
Allison DB, Faith MS, Heo M, Townsend-Butterworth D, Wiliamson DF . Meta-analysis of the effect of excluding early deaths on the estimated relationship between body mass index and mortality Obes Res 1999 7: 342–354.
Allison DB, Heo M, Flanders DW, Faith MS, Carpenter KM, Williamson DF . Simulation study of the effects of excluding early deaths on risk factor–mortality analyses in the presence of confounding due to occult disease: the example of body mass index Ann Epidemiol 1999 9: 132–142.
Allison DB, Zannolli R, Faith MS, Heo M, Pietrobelli A, Vanltallie TB, Pi-Sunyer FX, Heymsfield SB . Weight loss increases and fat loss decreases all-cause mortality rate: results from two independent cohort studies Int J Obes Relat Metab Disord 1999 23: 603–611.
National Heart Lung and Blood Institute . Clinical guidelines for the identification, evaluation, and treatment of overweight and obesity in adults. The evidence report Obes Res 1998 6(Suppl 2): 51–209.
Heymsfield SB, Wang ZM, Baumgartner RN, Ross R . Human body composition: advances in models and methods A Rev Nutr 1997 17: 527–558.
Heymsfield SB, Allison DB, Heshka S, Pierson RN Jr . Assessment of human body composition. In: Allison DB (ed). Handbook of assessment methods for eating behaviors and weight-related behaviors Sage: Thousand Oaks, CA 1995 515–560.
Norton K . Anthropometric estimation of body fat. In: Norton K, Olds T (eds.) Anthropometrica Sydney: UNSW Press 1996 172–198.
Couillard C, Gagnon J, Bergeron J, Leon AS, Rao DC, Skinner JS, Wilmore JH, Despres JP, Bouchard C . Contribution of body fatness and adipose tissue distribution to the age variation in plasma steroid hormone concentrations in men: the Heritage Family Study J Clin Endocrinol Metab 2000 85: 1026–1031.
Pi-Sunyer FX . Medical hazards of obesity Ann Intern Med 1993 119: 655–660.
Mitsiopoulos N, Baumgartner RN, Heymsfield SB, Lyons W, Gallagher D, Ross R . Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography J Appl Physiol 1998 85: 115–122.
Acknowledgements
We are grateful to David F Williamson for his helpful comments. This research was supported in part by NIH grants AG17166, DK51716 and DK26687, and unrestricted grants from Merck Pharmaceuticals, Tanita Incorporated Mead-Johnson and the Sugar Association.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Allison, D., Zhu, S., Plankey, M. et al. Differential associations of body mass index and adiposity with all-cause mortality among men in the first and second National Health and Nutrition Examination Surveys (NHANES I and NHANES II) follow-up studies. Int J Obes 26, 410–416 (2002). https://doi.org/10.1038/sj.ijo.0801925
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0801925
Keywords
This article is cited by
-
Hypertension modifies the associations of body mass index and waist circumference with all-cause mortality among older Chinese: a retrospective cohort study
BMC Geriatrics (2022)
-
Interpretable machine learning prediction of all-cause mortality
Communications Medicine (2022)
-
Calf Circumference and All-Cause Mortality: A Systematic Review and Meta-Analysis Based on Trend Estimation Approaches
The Journal of nutrition, health and aging (2022)
-
Levels and changes in body mass index decomposed into fat and fat-free mass index: relation to long-term all-cause mortality in the general population
International Journal of Obesity (2020)
-
The association between body composition and quality of life among elderly Italians
Endocrine (2020)