Abstract
OBJECTIVE: To test the sensitivity of waist circumference (central adiposity) as an index of disease risk in postmenopausal women.
DESIGN: Retrospective analysis of postmenopausal women tested at Washington University School of Medicine.
SUSBJECTS: A total of 323 healthy postmenopausal (66±5 y; mean±s.d.) women not using any hormone replacement.
MEASUREMENTS: Body composition, hyperinsulinemia (insulin area), triglycerides and HDL-cholesterol.
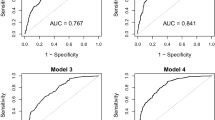
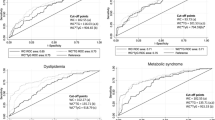
RESULTS: Excess waist size had a stronger association with hyperinsulinemia and hypertriglyceridemia than body mass index (BMI; kg/m2) in otherwise healthy, postmenopausal women. After adjusting for BMI, a strong relation existed between waist circumference and insulin area, HDL-cholesterol and triglycerides (P<0.01). Conversely, after adjusting for waist circumference, no relation was apparent between BMI and the dependent variables of interest. The strength of the association between waist circumference and disease risk became most apparent when analyses were restricted to normal-weight women (BMI 24–28 kg/m2). When BMI was held constant, hyperinsulinemia and triglyceridemia increased dose-dependently with changes in waist size.
CONCLUSION: Waist circumference, an easily obtained index of central adiposity, is a more sensitive measure of relative disease risk than is BMI in middle-aged and older women, particularly in normal-weight individuals.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Manson J, Willet W, Mier J et al. Body weight and mortality among women New Engl J Med 1995 333: 677–685.
Stevens J, Cai J, Pamuk ER, Williamson DF, Thun MJ, Wood JL . The effect of age on the association between body-mass index and mortality New Engl J Med 1998 338: 1–7.
Ohlson L-O, Larsson B, Sva¨rdsudd K et al. The influence of body fat distribution on the incidence of diabetes mellitus: 13.5 years of follow-up of the participants in the study of men born in 1913 Diabetes 1985 34: 1055–1058.
Seidell J, Han T, Feskens E, Lean M . Narrow hips and broad waist circumferences independently contribute to increased risk of non-insulin-dependent diabetes mellitus J Intern Med 1997 242: 401–406.
Rexrode K, Carey V, Hennekens C et al. Abdominal adiposity and coronary heart disease in women JAMA 1998 280: 1843–1848.
Folsom A, Kaye S, Sellers T et al. Body fat distribution and 5-year risk of death in older women JAMA 1993 269: 483–487.
Bjo¨rntorp P . Body fat distribution, insulin resistance, and metabolic diseases Nutrition 1997 13: 795–803.
Despres J-P . The insulin resistance-dyslipidemic syndrome of visceral obesity: effect on patient's risk Obes Res 1998 6: S8–S17.
Ley CJ, Lees B, Stevenson JC . Sex- and menopause-associated changes in body-fat distribution Am J Clin Nutr 1992 55 950–954.
Kannel WB, Wilson PW . Risk factors that attenuate the female coronary disease advantage Arch Intern Med 1995 155: 57–61.
Poehlman ET, Toth MJ, Gardner AW . Changes in energy balance and body composition at menopause: a controlled longitudinal study Ann Intern Med l995 123: 673–675.
Wing R, Matthews K, Kuller L, Meilahn E, Plantinga P . Weight gain at the time of menopause Arch Intern Med 1991 151: 97–102.
Poiliot MC, Despres J-P, Lemieux S et al. Waist circumference and abdominal sagittal diameter: best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women Am J Cardiol 1994 73: 460–468.
Lean ME, Han TS, Seidell JC . Impairment of health and quality of life in people with large waist circumference Lancet 1998 351: 853–856.
American Diabetes Association . Report of the expert committee on the diagnosis and classification of diabetes mellitus Diabetes Care 1998 21: S5–S19.
Kohrt WM, Malley MT, Dalsky GP, Holloszy JO . Body composition of healthy sedentary and trained, young and older men and women Med Sci Sports Exerc 1992 24: 832–837.
Brozek J, Grande F, Anderson JT, Keys A . Densitometric analysis of body composition: revision of some quantitative assumptions Ann NY Acad Sci 1963 110: 113–140.
Warnick GR, Benderson J, Albers JJ . Dextran sulfate-Mg2+ precipitation procedure for quantification of high-density lipoprotein cholesterol Clin Chem 1982 28: 1379–1388.
Friedewald W, Levy R, Fredrickson D . Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without the use of the preparative ultracentrifuge Clin Chem 1972 18: 499–502.
Morgan DR, Lazarow A . Immunoassay of insulin: two antibody system Diabetes 1963 12: 115–126.
Bjorkelund C, Lissner L, Andresson S, Lapidus L, Bengtsson C . Reproductive history in relation to relative weight and fat distribution Int J Obes Relat Metab Discord 1996 20: 213–219.
Espeland MA, Stefanick ML, Kritz-Silverstein D et al. Effect of postmenopausal hormone therapy on body weight and waist and hip girths J Clin Endocrinol Metab l997 82: 1549–1556.
Gambacciani M, Ciaponi M, Cappagli B et al. Body weight, body fat distribution, and hormonal replacement therapy in early postmenopausal women J Clin Endocrinol Metab 1997 82: 414–417.
The Writing Group for the PEPI Trial . Effects of hormone replacement therapy on endometrial histology in postmenopausal women. The Postmenopausal Estrogen/Progestin Inverventions (PEPI) Trial JAMA 1996 275: 370–375.
Samaras K, Hayward C, Sullivan D, Kelly R, Campbell L . Effects of postmenopausal hormone replacement therapy on central abdominal fat, glycemic control, lipid metabolism, and vascular factors in type 2 diabetes: a prospective study Diabetes Care 1999 22: 1401–1407.
Van Pelt R, Davy K, Stevenson E et al. Smaller differences in total and regional adiposity with age in regularly exercising compared with sedentary women Am J Physiol (Endocrin Metab) 1998 275 E626–E634.
Kohrt WM, Obert KA, Holloszy JO . Exercise training improves fat distribution patterns in 60- to 70-yr-old men and women J Gerontol 1992 47: M99–M105.
Kohrt WM, Ehsani AA, Birge SJ . HRT preserves increases in bone mineral density and reductions in body fat after a supervised exercise program J Appl Physiol 1998 84: 1506–1512.
Acknowledgements
This research was supported by the following awards from the National Institutes of Health: Claude Pepper Older Americans Independence Center, AG13629; Research Career Development, AG00663 (Kohrt); General Clinical Research Center, RR00036; and Diabetes Research and Training Center, DK20579.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Van Pelt, R., Evans, E., Schechtman, K. et al. Waist circumference vs body mass index for prediction of disease risk in postmenopausal women. Int J Obes 25, 1183–1188 (2001). https://doi.org/10.1038/sj.ijo.0801640
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0801640
Keywords
This article is cited by
-
Abdominal obesity and digestive system cancer: a systematic review and meta-analysis of prospective studies
BMC Public Health (2023)
-
Effects of diet and exercise on weight-related outcomes for breast cancer survivors and their adult daughters: an analysis of the DAMES trial
Supportive Care in Cancer (2017)
-
Impact of body fat changes in mediating the effects of antiretroviral therapy on blood pressure in HIV-infected persons in a sub-Saharan African setting
Infectious Diseases of Poverty (2016)
-
Objectively measured physical activity and sedentary time of breast cancer survivors, and associations with adiposity: findings from NHANES (2003–2006)
Cancer Causes & Control (2010)
-
Left ventricular mass, abdominal circumference and age: The Fels Longitudinal Study
The Journal of nutrition, health and aging (2009)