Abstract
Purpose
This retrospective comparative case series aims to determine whether patient ethnicity (White versus South Asian versus Black) is related to the outcome of surgical treatment for traction complications of severe proliferative diabetic retinopathy (PDR).
Setting
Moorfields Eye Hospital London, UK.
Methods
All patients who underwent vitrectomy with, delamination and/or segmentation for PDR over a 5-year period (2009–2014) were reviewed retrospectively. Patients were divided into White, South Asian or Black groups, and their age, gender, HbA1C and type of diabetes were recorded. A total of 484 patients (253 White, 117 South Asian, 114 Black) were included. Twenty-one patients were excluded due to inadequate documentation.
Outcomes
LogMAR Visual acuity (converted from Snellen) (VA), was recorded pre-operatively and ~6 months post surgery (range 5–8 months). Surgical outcome was classified according to the type and duration of tamponade required post-operatively.
Results
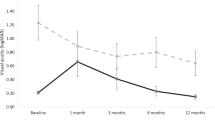
Pre-operative VA and HbA1C values were similar across all three ethnic groups (P=0.64 and 0.569, respectively). Change in VA (mean±SD) was 0.41±0.78, 0.14±0.76 and −0.26±0.57 in White, South Asian and Black patient groups respectively (P<0.001). Multiple regression analysis showed that post-op VA was significantly related to race and pre-op VA only (both P<0.001). The Black patient group were more likely to require silicone oil tamponade (P<0.001) and long-term retention of silicone oil (P<0.001) than the White and South Asian patient groups.
Conclusions
This study demonstrates that Black patients on average lose vision following delamination surgery for traction complications of PDR while White and South Asian patients gain vision. The same group is also at higher risk of retaining silicone more than 6 months after surgery. This difference remains even when corrected for glycaemic control. The higher risk of visual loss and long-term retention of silicone oil in black patients requires further investigation. If these results are confirmed, surgeons should consider their patients’ ethnicity before proceeding with surgical treatment of diabetic tractional detachment.
Similar content being viewed by others
Introduction
Vision loss is one of the most feared complications amongst the diabetic population. Although the risk of retinopathy can be reduced with good glycaemic and blood pressure (BP) control1, 2, 3, 4 and, ocular complications may be treatable with laser,5 surgery6 and pharmacologically,7 visual loss from diabetic retinopathy (DR) remains prevalent. Severe proliferative diabetic retinopathy (PDR) poses the most serious threat to sight. Complications of PDR such as intraocular haemorrhage, fibrous proliferation, traction retinal detachment or traction retinoschisis8, 9 can lead to profound vision loss.10 The prevalence of PDR is estimated at between 13 and 50% after 15–20 years of diabetes duration in patients needing insulin11, 12 with a risk of becoming legally blind after 5–10 years if left untreated.13
Vitreo-retinal surgery, including vitrectomy, with or without delamination and segmentation, is recognised as the principal treatment for late complications of PDR such as intraocular haemorrhage, traction retinal detachment (involving or threatening the macula) and, uncontrolled progressive fibro-vascular proliferation.6, 14 The main aims of surgery are to clear the media opacities (usually blood) and divide or remove as many as possible of the adhesions causing retinal traction. Although several studies have evaluated the outcomes, complications and benefits of surgery for the complications of PDR,6, 14, 15, 16 differences in outcome relative to ethnic origin have not been investigated.17 This study sets out to explore the impact of the ethnicity of patients—White versus Black versus South Asian, on the treatment outcomes of the subgroup of patients who undergo vitrectomy with delamination and/or segmentation surgery for the traction complications of severe PDR.
Methods
Patient selection and inclusion
This work describes a retrospective (2009–2014) comparative case series from a tertiary referral centre in the United Kingdom. A search of all surgical bookings on the electronic patient record database using the keywords ‘diabetes’ and/or ‘vitrectomy’ and/or ‘delamination’ and/or ‘segmentation’ was performed to identify all of the diabetic patients who underwent vitrectomy surgery (including ‘with delamination and segmentation’) during this period. Manual checking of each patient’s case note was performed to confirm the actual diagnoses and surgical procedures performed. Where delamination and/or segmentation were specifically recorded as part of the operation, the subject was included in our study. Cases of vitreous haemorrhage that only required vitrectomy and laser were excluded. The study received prospective internal review board approval (Research and Development, Moorfields Eye Hospital NHS Foundation Trust. Reference number: ROAD 14/038).
Demographics
Ethnicity was classified according to the hospital record of self-reported ethnicity at registration for each patient. Patients were placed into three main groups: White, Black, or South Asian. The subgroups pooled into each main group were White (White British, White Irish, White any other background), South Asian (Indian, Pakistani, Afghan, Bangladeshi, Nepalese, Bhutanese, Maldivian) and Black (African, Caribbean, Black any other background). Cases where the ethnicity was not accurately recorded or not declared were excluded from the study. Mixed race or Filipino/Oriental racial groups were also excluded from the study but were minimal in number.
Other details collected were age, gender and type of diabetes. All Black patients were tested for the presence of Haemoglobin S and those that were positive were excluded from the study as their retinal pathology was treated as non-diabetic (6 patients were excluded for this reason).
Functional outcome
Visual acuity (VA), using the patients’ habitual best correction, was measured in Snellen and converted to logMAR. The VA was recorded pre-operatively and at the follow-up visit closest to 6 months post-operatively in both eyes (range 5–8 months), this will be referred to as the 6 months visit. The sub-form acuity measures namely ‘counting fingers’ (CF), ‘hand motion’ (HM), ‘light perception’ (LP) and ‘no light perception’ (NLP) received the following logMAR values: CF=1.6, HM=2.0, LP=2.5, NLP=3.0.18
Surgical outcome
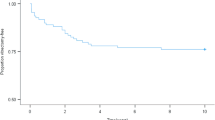
The surgical outcome for each patient was recorded according to the type and duration of retinal tamponade required post-operatively. These were classified into three groups being (1) gas only or no tamponade (2) Silicone Oil (SO) tamponade used but removed <6 months post-operatively, and (3) SO used and retained ≥6 months.
Glycaemic control
HbA1c was recorded for each patient within 1 month of surgery.
Bilateral disease
In patients with bilateral traction pathology, where both eyes required vitrectomy and delamination surgery one eye was randomly chosen (http://www.randomizer.org/) for inclusion in the study in order to maintain sample independence.
Statistical analysis
All statistical analyses were performed using SPSS 23 for Mac (SPSS, Chicago, IL, USA). Descriptive statistics were presented as mean±SD. Histograms were plotted for each of the three variables—age, VA, and HbA1c levels to assess the normality of their sample distributions. After consultation with an independent statistician and, as normality of the sample distribution could not be established for the above three variables, non-parametric tests were chosen for the analysis. The level of statistical significance is set as P<0.05. A multiple regression analysis was performed to predict the post-operative VA from age, pre-operative VA, HbA1c level, diabetes type (1 or 2), and ethnicity.
Results
The electronic search identified 1376 diabetic patients who underwent vitrectomy over the study period. Of these, 502 patients (668 eyes) were identified as having delamination or segmentation surgery as described above. Eighteen patients (27 eyes, 3.5%) were excluded because of inadequate documentation in the electronic database and case notes, or because they did not fit clearly into the three main racial groups we were analysing. Data from only one eye of the remaining 484 patients were analysed.
Demographics
Of the 484 patients, 253 were White, 117 were South Asian, and 114 were Black. Overall, 157 (32%) patients had bilateral surgery. As a proportion of the total number of patients within each racial group the number of patients having bilateral surgeries were 93/253 (37%) White, 33/117 (28%) South Asian and 31/114 (27%) Black.
The mean age (years)±standard deviation (SD) for all patients was 51.9±14.4. This was 48.9±15.6, 54.5±11.7, and 56.1±12.7 in the White, South Asian and Black groups respectively. The White group was significantly younger than South Asian and Black groups (P=0.001 and P<0.001 respectively, Mann–Whitney U-test). There were 213 females (44.0%) and 271 males (56.0%) in total. Gender was not associated with racial group (% male by racial group was: 54.9% for White, 57.3% for South Asian, and 57.0% for Black; P-value from χ2-test=0.887).
Type 1 diabetes was present in 159 (33%) patients, while 325 patients (67%) had type 2 diabetes. Type 1 diabetes was more common in the White patient group (% type 1 by racial group was: 45.9% for White, 17.1% for South Asian, 20.2% for Black; P-value from χ2-test<0.001). Within the type 2 group, the mean age (years)±SD was: 60.2±10.0, 57.7±9.0, and 60.4±9.0 for White, South Asian, and Black groups, respectively. There were no statistically significant differences in the age distribution of the type 2 diabetic patients across the three ethnic groups (P=0.89, Kruskal–Wallis test).
As type 1 diabetes typically present in much younger patients, giving rise to the younger mean age of in the White group of patients, we performed subgroup comparisons of only the type 2 diabetic patients across the three ethnic groups.
Glycaemic control
HbA1c values were available in 91% of the patients. The mean and standard deviation for each racial group are listed in Table 1. There were no significant differences in the distribution of HbA1c across the three groups (P=0.569, Kruskal–Wallis test). Pearson’s correlation analysis indicated that there was no significant association between peri-operative HbA1c level and the final VA at 6 months post-operatively (Pearson’s correlation=0.097).
Functional outcomes
Visual acuity was available for all patients pre-operatively and at 6 months post-operatively (as defined) in both eyes. The median pre-operative VA with interquartile range (logMAR), median post-operative VA with interquartile range (logMAR) and the mean change in VA±SD after surgery for patients in each ethnic group is recorded in Table 1. The same parameters for type 2 diabetic patients are also recorded for each ethnic group in Table 1.
The percentages of patients from each racial group with sub-form vision (including combined CF, HM, PL, and NPL), both pre and post-operative are documented in Table 1.
Multiple regression analysis
A multiple regression was performed to predict the post-op BCVA from age, pre-operative BCVA, per-operative HbA1c level, Diabetes type (1 or 2), and ethnicity. Collectively these variables significantly predicted post-op BCVA (F(5, 436)=39.1, P<0.001, R2=0.31). Of these, only two variables showed statistically significant predictive value for the outcome of post-op BCVA. They are pre-op VA and ethnicity (P<0.001 for both).
Outcomes of patients without long-term silicone oil tamponade
Subgroup analysis looking at the VA outcome in patients who did not require long-term silicone oil tamponade showed that the median pre and post-operative VA (InterQuartile Range) was 1 (0.18–2.50) and 0.48 (−0.8 to 3) for the White group (n=235, 93% of White patients), 1 (0.18–2.50) and 0.6 (0–3) for the South Asian group (n=107, 91% of South Asian patients), and 0.78 (0.18–1.83) and 1 (0–3) for Black group (n=80, 70% of Black patients). No further statistical analysis was performed as this subgroup represented an inherently biased cohort selected for better outcome. However, the trend indicates that more White and South Asian patients are likely to be tamponade free in the long term, with better VA than Black patients.
Surgical outcome
The proportions of patients requiring SO tamponade at the end of surgery and those with SO retained after the 6 month’s visit are recorded in Table 1.
Discussion
Vision loss secondary to DR remains a major public health issue for most countries. Ethnic differences in the incidence, prevalence, severity and response to treatment in DR, as well as other ophthalmic conditions such as glaucoma and cataract have been demonstrated.19, 20, 21, 22, 23 In this study, we have shown that Black patients on average lose vision while White and South Asian patients gain vision following surgical delamination or segmentation for tractional retinal detachment or tractional schisis secondary to PDR. We have also observed that ethnicity affects the anatomical outcomes following surgery in that silicone oil is used in surgery and retained after 6 months more frequently in Black patients, than South Asian or White patients.
In terms of PDR we have observed within our study, that the proportion of White, South Asian and Black patients were 52.3, 24.2, and 23.5% while the respective proportion of these groups in the London population are 59.7, 16.9, and 11.2%.24 This indicates that a higher proportion of South Asian and Black patients had severe PDR requiring surgery, which compounds the finding that the Black patient group has a much poorer visual and surgical outcomes after surgery. The proportions may also reflect the higher representation of type 2 diabetes in these two ethnic groups.25
The mean age of the patients in our series was lower in the White group, though this likely reflects the higher prevalence of type 1 diabetes in White patients compared to South Asian (up to 3 times) and Black (up to 6 times) patients.26 When only type 2 diabetic patients were analysed, the age distribution was comparable for the three groups, but the Black group still had a significantly worse visual outcome. Importantly, a multiple regression analysis showed that mean age, type of diabetes and HbA1c alone across the three ethnic groups were insufficient to explain the differences in their visual outcome. It also confirmed that race and pre-operative VA was significantly predictive of final VA.
HbA1c level was not predictive of outcome independently of race and this is consistent with data from diabetic screening. Retinal screening has demonstrated a reduction in sight threatening DR in London,27 with non-attendance to screening not influenced by ethnicity despite the disparity in socio-economic status.28 In our cohort of patients there was also no significant difference in HbA1c levels between the different ethnic groups. The poorer visual outcomes observed in the South Asian and Black patients, therefore, could not be explained by differences in the systemic control of diabetes alone.
In many surgical treatments, the operative outcome is partly determined by the technical difficulty of the procedure. For diabetic delamination surgery, we have used the type and duration of tamponade required as a defacto indicator of the degree of difficulty and anatomical outcome of surgery. Silicone oil tamponade is mainly used in technically difficult cases in which retinal re-attachment is threatened by residual retinal traction.29 In a previous study, Yorston et al17 showed that the use of long-acting tamponades, that is, silicone oil, was more likely in eyes with extensive areas of retinal adhesions. They noted this surgical feature more frequently in Black patients than in patients of other ethnicities. In our study, Black patients showed a markedly higher rate of SO tamponade and retention of SO long term (≥ 6 months) than in the other groups. It is possible that Black patients have stronger vitreo-retinal adhesions thereby rendering surgical delamination of their eyes technically more difficult. In keeping with the worse surgical outcomes, the post-operative visual acuity was also significantly worse in Black patients relative to the other two groups. In a subgroup analysis of visual acuity outcomes in patients who did not have silicone oil at 6 months there was a trend for black and South Asian patients to do worse. We did not examine this statistically as there was a sampling bias in the choice of good outcome but it suggests black patients may do worse after surgery independent of silicone.
In our study, a potential confounding factor in terms of visual outcome is the extent and timing of previous retinal laser treatment. Unfortunately, we could not get reliable information about timing and extent of laser in this cohort of patients to analyse its effect. Furthermore, the extent of fibrovascular tissue could also be more extensive in black patients and therefore influence the visual and anatomical outcomes of surgery. Unfortunately, the source data in this retrospective study did not have the quality and consistency to allow us to make these assessments, which leave potential confounding variables unaddressed and we acknowledge identifies a limitation to the study.
Another limitation of our study is the retrospective design, which may represent a selection bias. Also, not all patients had peri-operative HbA1c measurements, though this data was available for 91% of the patients and was equally distributed between the three ethnic groups. We were not able to control for all major risk factors for the progression of diabetes and micro-vascular diseases, such as the presence of systemic hypertension and renal disease. Nevertheless, we feel that these factors may be less important, as we are evaluating a group of patients who already manifest a late complication of diabetes.
This study aimed to identify whether the outcome of surgical delamination or segmentation for traction complications of PDR was affected by the patients’ ethnicity. Whilst black ethnicity may provide a protective influence on diabetes-associated macro-vascular disease,30 our data strongly suggests that Black diabetic patients have significantly worse surgical and visual outcomes following diabetic delamination and segmentation surgery than White and South Asian patients. As poor surgical and subsequent functional outcomes lead to profound visual loss, we feel this ethnic difference needs to be highlighted so that further research can be performed in this area. Guthrie et al31 describe diabetic vitrectomy in E. Africa, and noted the beneficial effect of pre-treatment with Bevacizumab in a predominantly black population. It may be that use of a similar technique in the UK might lead to better results in Black patients. Currently, treatment and consenting discussions for severe PDR do not differentiate between different racial groups but given the potentially worse visual and surgical outcomes with long-term retention of silicone oil in black patients this distinction should be made.

References
Klein R, Klein BE, Moss SE, Cruickshanks KJ . The Wisconsin Epidemiologic Study of Diabetic Retinopathy: XVII. The 14-year incidence and progression of diabetic retinopathy and associated risk factors in type 1 diabetes. Ophthalmology 1998; 105 (10): 1801–1815.
Turner R, Holman R, Stratton I, Cull C, Frighi V, Manley S et al. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ 1998; 317 (7160): 703–713.
Stratton IM, Kohner EM, Aldington SJ, Turner RC, Holman RR, Manley SE et al. UKPDS 50: risk factors for incidence and progression of retinopathy in Type II diabetes over 6 years from diagnosis. Diabetologia 2001; 44 (2): 156–163.
Yau JW, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care 2012; 35 (3): 556–564.
Vander JF, Duker JS, Benson WE, Brown GC, McNamara JA, Rosenstein RB . Long-term stability and visual outcome after favorable initial response of proliferative diabetic retinopathy to panretinal photocoagulation. Ophthalmology 1991; 98 (10): 1575–1579.
Scanlon PH . Why do patients still require surgery for the late complications of Proliferative Diabetic Retinopathy? Eye (Lond) 2010; 24 (3): 435–440.
Montero JA, Ruiz-Moreno JM, Correa ME . Intravitreal anti-VEGF drugs as adjuvant therapy in diabetic retinopathy surgery. Curr Diabetes Rev 2011; 7 (3): 176–184.
Lincoff H, Serag Y, Chang S, Silverman R, Bondok B, el-Aswad M . Tractional elevations of the retina in patients with diabetes. Am J Ophthalmol 1992; 113 (3): 235–242.
Imai M, Iijima H, Hanada N . Optical coherence tomography of tractional macular elevations in eyes with proliferative diabetic retinopathy. Am J Ophthalmol 2001; 132 (3): 458–461.
Nelson RG, Wolfe JA, Horton MB, Pettitt DJ, Bennett PH, Knowler WC . Proliferative retinopathy in NIDDM. Incidence and risk factors in Pima Indians. Diabetes 1989; 38 (4): 435–440.
Klein R . The epidemiology of diabetic retinopathy: findings from the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Int Ophthalmol Clin 1987; 27 (4): 230–238.
Rossing K, Jacobsen P, Rossing P, Lauritzen E, Lund-Andersen H, Parving HH . Improved visual function in IDDM patients with unchanged cumulative incidence of sight-threatening diabetic retinopathy. Diabetes Care 1998; 21 (11): 2007–2015.
Deckert T, Simonsen SE, Poulsen JE . Prognosis of proliferative retinopathy in juvenile diabetics. Diabetes 1967; 16 (10): 728–733.
Helbig H . Surgery for diabetic retinopathy. Ophthalmologica 2007; 221 (2): 103–111.
Helbig H, Sutter FK . Surgical treatment of diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol 2004; 242 (8): 704–709.
Jackson TL, Donachie PH, Sallam A, Sparrow JM, Johnston RL . United Kingdom National Ophthalmology Database study of vitreoretinal surgery: report 3, retinal detachment. Ophthalmology 2014; 121 (3): 643–648.
Yorston D, Wickham L, Benson S, Bunce C, Sheard R, Charteris D . Predictive clinical features and outcomes of vitrectomy for proliferative diabetic retinopathy. Br J Ophthalmol 2008; 92 (3): 365–368.
Arroyo JG, Postel EA, Stone T, McCuen BW, Egan. KM . A matched study of primary scleral buckle placement during repair of posterior segment open globe injuries. Br J Ophthalmol 2003; 87: 75–78.
Arfken CL, Reno PL, Santiago JV, Klein R . Development of proliferative diabetic retinopathy in African-Americans and whites with type 1 diabetes. Diabetes Care 1998; 21 (5): 792–795.
Sivaprasad S, Gupta B, Crosby-Nwaobi R, Evans J . Prevalence of diabetic retinopathy in various ethnic groups: a worldwide perspective. Surv Ophthalmol 2012; 57 (4): 347–370.
West SK, Munoz B, Schein OD, Duncan DD, Rubin GS . Racial differences in lens opacities: the Salisbury Eye Evaluation (SEE) project. Am J Epidemiol 1998; 148 (11): 1033–1039.
Quigley HA, Broman AT . The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 2006; 90 (3): 262–267.
Cheng JW, Zong Y, Zeng YY, Wei RL . The prevalence of primary angle closure glaucoma in adult Asians: a systematic review and meta-analysis. PLoS One 2014; 9 (7): e103222.
2011. UK Census. Available at: http://www.ons.gov.uk/ons/guide-method/census/2011/uk-census/index.html and http://webarchive.nationalarchives.gov.uk/20160105160709/http://www.ons.gov.uk/ons/rel/mro/news-release/census-2-1——london/census-gives-insights-into-characteristics-of-london-s-population.html.
Winkley K, Thomas SM, Sivaprasad S, Chamley M, Stahl D, Ismail K et al. The clinical characteristics at diagnosis of type 2 diabetes in a multi-ethnic population: the South London Diabetes cohort (SOUL-D). Diabetologia 2013; 56 (6): 1272–1281.
JY N . The Health of Britain’s Ethnic Minorities: Findings From a National Survey. Policy Studies Institute: London, UK, 1997.
Forster AS, Forbes A, Dodhia H, Connor C, Du Chemin A, Sivaprasad S et al. Changes in detection of retinopathy in type 2 diabetes in the first 4 years of a population-based diabetic eye screening program: retrospective cohort study. Diabetes Care 2013; 36 (9): 2663–2669.
Forster AS, Forbes A, Dodhia H, Connor C, Du Chemin A, Sivaprasad S et al. Non-attendance at diabetic eye screening and risk of sight-threatening diabetic retinopathy: a population-based cohort study. Diabetologia 2013; 56 (10): 2187–2193.
Castellarin A, Grigorian R, Bhagat N, Del Priore L, Zarbin MA . Vitrectomy with silicone oil infusion in severe diabetic retinopathy. Br J Ophthalmol 2003; 87 (3): 318–321.
Davis TM, Coleman RL, Holman RR . Ethnicity and long-term vascular outcomes in Type 2 diabetes: a prospective observational study (UKPDS 83). Diabet Med 2014; 31 (2): 200–207.
Guthrie G, Hall AB, Dhalla K, Davies RM, Steel DH . Bevacizumab as an adjunct to vitreoretinal surgery for diabetic retinopathy in East Africa. Eye (Lond) 2013; 27 (11): 1263–1268.
Acknowledgements
LdC previously received a government support from the Medical Research Council and National Institute of Health Research and from the Industry consultancy Reneuron and Alimera (not current or ongoing), Second Sight Medical Instruments, Inc. CE previously received grant awards and advisory board support from Novartis Pharmaceuticals for research in diabetic retinopathy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Mastropasqua, R., Luo, YL., Cheah, Y. et al. Black patients sustain vision loss while White and South Asian patients gain vision following delamination or segmentation surgery for tractional complications associated with proliferative diabetic retinopathy. Eye 31, 1468–1474 (2017). https://doi.org/10.1038/eye.2017.95
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2017.95
This article is cited by
-
The effect of ethnicity on anatomic success following macular hole surgery: a multicentre cohort study
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
The UK National Artificial Eye Questionnaire study: predictors of artificial eye wearers’ experience part 1—comfort and satisfaction
Eye (2021)
-
Surgical outcomes of vitrectomy surgery for proliferative diabetic retinopathy in patients with abnormal renal function
Graefe's Archive for Clinical and Experimental Ophthalmology (2020)
-
Beneficial visual outcome of vitrectomy and delamination surgery for tractional complications of diabetic retinopathy in a cohort of black patients
Eye (2019)