Abstract
Purpose
To study the effect of orbital tumors on visual functions and highlight the factors predictive of visual outcome after surgery.
Methods
A prospective interventional study compared visual function parameters and fundus changes, before and after surgery, in eyes having well-defined orbital tumors with the normal fellow eye. These included visual acuity (VA), refractive error, keratometry changes, color vision, Goldmann visual field (GVF), and visual evoked response (VER).
Results
In total 28 cases (age range 7–56 years), of which the majority of tumors were vascular (46%) and lacrimal (18%) in origin, had a mean VA of 0.54±0.33 in the affected eye, which improved postoperatively to 0.66±0.31 (P=0.002). The affected eye had a median refractive error of +0.00 DS (−2.00 to 5.13), which was significantly more hyperopic than the normal eye (median +0.00 DS; range −1.25 to +1.63 DS) and normalized postoperatively. Keratometry showed higher astigmatism in the involved eye (P=0.004). The fundus showed disc pallor, edema, and/or choroidal folds, of which disc edema resolved in all cases after surgery. In all, 40% of the affected eyes had a deficient color vision and this partially improved postoperatively (P=0.25). GVF had abnormalities in 10 cases, half of which normalized postoperatively (P=0.04). The VER of affected eyes had a mean amplitude of 8.91±4.59 μv and latency of 116.3±14.7 ms, with improvement after surgery (P=0.005 and 0.001, respectively).
Conclusion
Orbital tumors adversely affected visual functions. The presenting acuity depended on disc changes, color vision abnormalities, and prolonged VER latency. The postoperative VA depended on VA at presentation, amount of proptosis, degree of hyperopia, and clinically significant VER abnormalities.
Similar content being viewed by others
Introduction
Orbital tumors account for about 11–36% of all the benign and malignant neoplasias of the eye and adnexa in India.1, 2 Owing to their varied ocular impact and post-surgical course, it is often difficult to give the patient a definitive visual prognosis. There have been a few sporadic studies involving small numbers addressing visual acuity (VA), refractive error, fundus, or visual-field changes in specific orbital tumors, but the literature lacks a comprehensive larger study of all the visual-function parameters and their interrelations.3, 4, 5, 6, 7 This study aims to evaluate the effect of an orbital tumor on the visual-function parameters, with emphasis on the factors predictive of visual outcome after surgery.
Materials and methods
A prospective interventional study was conducted at a tertiary-care eye hospital after approval from the ethics committee. All patients admitted for surgery with a well-defined unilateral orbital tumor within a 2-year period commencing June 2008 were included. Exclusion criteria included those patients with best-corrected VA in either eye worse than 20/200, those aged below 5 years, patients who were uncooperative or unwilling for evaluation or follow-up, and those who had another associated ocular disease affecting visual-function parameters in either eye. All patients underwent a complete ocular and systemic evaluation, including a cycloplegic refraction with post mydriatic testing and a subjective acceptance (to define the best-corrected VA), Hertel's exophthalmometry, color vision testing using Ishihara charts, manual keratometry (Baush and Lomb keratometer; Bausch and Lomb, Rochester, NY, USA), Goldmann visual field (GVF) testing, and a pattern visual evoked response (VER) test (Nicolet Ganzfeld stimulator, Nicolet Inc., Madison, WI, USA). Appropriate imaging was done to determine the type, extent, and location of tumor mass. Surgical removal of the orbital tumor was done. The refraction and investigations were repeated at the 2-week, 1-month, and 3-month follow-up visits. The data was analyzed in two sets, one comparing the visual-function parameters in the eye with orbital tumor vis-a-vis the fellow eye, while the other compared the pre- and postoperative visual parameters in the involved eye. Associations between the visual function and clinical parameters were also examined.
Refractive error was compared as the spherical equivalent for analysis. In keratometry, the difference between the two meridian readings was analyzed as corneal astigmatism. On the Ishihara plates, a difference of four plates between the two eyes was defined as color deficiency. A difference of at least 10° between two visual fields was the criterion for defining expansion, constriction, or improvement of the GVFs. In the pattern VER, the amplitude of the waveform and p100 latency were compared. A difference of >2.5 μv and 10 ms in amplitude and latency, respectively, was considered to be clinically significant for analysis.8
Analysis was done using SPSS version 11.5 (SPSS Inc., Chicago, IL, USA) and Stata 8.0 (StataCorp LP, College Station, TX, USA) using appropriate parametric and non-parametric tests.
Statement of ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
Results
During the study period, 72 patients had presented with orbital tumors, of which 28 met the study criteria. Those who did not qualify included 19 patients with VA worse than 20/200, 18 patients with other confounding factors, 2 patients with age <5 years or uncooperative, 2 patients who did not undergo surgery, 2 patients who were lost to follow-up, and 1 patient who did not consent to repeated investigations. The clinical profile and tumor diagnosis are depicted in Table 1. Proptosis was noted in 93% of the cases. Tumors were equally divided between the intraconal and extraconal locations.
The mean VA in the eye with orbital tumor was significantly worse than that in the normal fellow eye (Table 2). In all, 60% (17/28) of the affected eyes had a Snellen VA of 20/40 or better, in contrast to 97% (27/28) of the fellow eyes (P<0.001, χ2-test). The acuity improved significantly after surgery, and finally at 3 months follow-up about 80% (22/28) of the cases had a VA of 20/40 or better in the operated eye (P=0.02, χ2-test). A total of 15 patients who had a VA of 20/30 or better improved or maintained their acuity, while 6 cases with preoperative VA worse than 20/120 did not show any improvement after surgery. Seven cases showed a transient decline in vision immediately after surgery, six of which improved on subsequent follow-up visits. The preoperative VA showed a significant correlation with a prolonged VER latency (r=−0.48, P=0.01). The final postoperative VA showed correlation with the amount of proptosis at presentation (r=−0.562, P=0.002) and degree of hyperopia induced (r=−0.534, P=0.004). It also strongly correlated with the VA at presentation (r=0.87, P<0.001). Both the acuity at presentation and the final acuity were significantly worse in those patients who also had color vision impairment. (P=0.01 and 0.001 respectively, t-test). The mean pre- or postoperative VA was not affected by the location of the tumor.
On cycloplegic refraction, it was noted that the spherical equivalent of the refractive error in eyes with orbital tumor was skewed towards hyperopia (median of +0.00 DS; range –2.00 to +5.13 DS), whereas the normal eyes were significantly less hyperopic (median +0.00 DS; range –1.25 to +1.63 DS) in comparison (P=0.036, Wilcoxon's signed rank test). After surgery, this hyperopia significantly decreased to a median value of −0.25 DS (range −1.25 DS to 4.38 DS) (P=0.002, Wilcoxon's signed rank test), which showed an insignificant difference compared with the normal eye (P=0.627, Wilcoxon's signed rank test) (Table 2). The degree of hyperopia was significantly correlated with the amount of proptosis (r=0.604, P=0.001, Spearman's correlation coefficient). Intraconal tumors showed more hyperopia than extraconal tumors, with a median of +0.75 DS (range −0.75 to +5.13 DS) against +0.00 DS (range −2.00 to +3.25 DS), though this difference was not statistically significant (P=0.061, Mann–Whitney U-test) (Table 3). The trend in change of refractive error showed a significant change within 2 weeks of surgery and most of the change occurred by the 1-month follow-up visit (Table 3).
Keratometry revealed a significantly higher corneal astigmatism in the eyes with orbital tumor (median 0.88 D; range 0.00–5.50 D) in comparison with the fellow eye (median 0.50 D; range 0.00–5.75 D) (P=0.004, Mann–Whitney U-test) (Table 2). This difference was significantly more in the extraconal (median 1.50 D; range 0.50–3.75 D) than in the intraconal tumors (median 0.50 D; range 0.00–5.50 D) (P=0.002, Mann–Whitney U-test). Postoperatively at 3 months, there was no significant change in the keratometry values. Keratometry changes were not associated with the amount of proptosis, duration of illness, VA, or fundus changes.
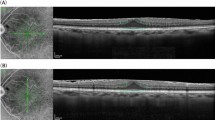
The fundus of 19 cases showed an abnormality in the proptosed eye, which significantly reduced to 14 cases after surgery at 3 months of follow-up (P<0.05, χ2-test). The frequent pre- and postoperative findings are depicted in Table 4. Those patients with optic disc changes at presentation had a significantly worse mean pre- and postoperative VA (P=0.02, t-test; P=0.01, t-test, respectively). Eyes with tumor having an abnormal fundus were significantly more hyperopic (+0.75 DS; −1.00 to 5.13 DS) in comparison with eyes with a normal fundus (−0.19 DS; −2.00 to +0.00 DS) (P=0.008, Mann–Whitney U-test). A similar association exists in the postoperative period. Fundus changes were not found to be associated with the amount of proptosis, duration of illness, or keratometry changes.
GVFs were significantly abnormal in 10 cases with respect to the fellow eye and five eyes showed improvement by 3 months after surgery (P=0.048, χ2-test). The notable field changes included an expansion of the temporal or nasal quadrant, constriction of the field, or centrocaecal scotomas (Table 4). Alterations in the visual field were found to have a significant association with fundus changes (P=0.01, McNemar), but were not related to the amount of proptosis, duration of illness, color vision abnormalities, or VER changes.
A defective color vision was present in 40% (11/28) of the cases, with no significant improvement after surgery (P=0.25, McNemar). Color vision deficit was associated with fundus changes (P<0.01, McNemar) and the amount of proptosis (P<0.01, Mann–Whitney U-test). Color vision changes were not significantly related to change in VA, duration of illness, or VER changes.
A pattern VER showed a decrease in mean amplitude and a significantly delayed latency preoperatively, both of which significantly improved 3 months after surgery (Table 2). For further analysis, a change >2.5 μv and 10 ms in amplitude and latency, respectively, was considered to be clinically significant (for inter- and intraocular analysis).8 On the basis of these criteria, 10 (35.7%) and 9 (32.1%) eyes showed a preoperative abnormality in VER amplitude and latency, respectively. One (3.6%) eye showed a clinically significant improvement in amplitude, while latency improved in 3 (10.7%) eyes after surgery, such that at the final follow-up visit amplitude was abnormal in 7 (25%) and latency prolonged in 5 (17.4%) eyes. VER latency showed a clinically significant improvement after surgery (P=0.04, Wilcoxon's signed rank test), whereas the amplitude did not (P=0.08, Wilcoxon's signed rank test). There were significant associations between VER amplitude abnormalities with presenting VA (Mann–Whitney U-test, P=0.008) and duration of illness (Mann–Whitney U-test, P=0.04), but not with location of tumor or fundus changes. The VER latency at presentation did not show a significant association with preoperative VA, but was related to changes in the fundus (Fisher's exact test, P=0.01). After surgery, final VA showed a significant association with persistent postoperative VER amplitude abnormalities, but not with VER latency changes (P=0.22, Mann–Whitney U-test). The amount of proptosis, color vision, and visual field changes did not hold significant associations with VER changes.
Discussion
The demographic profile of our cases is similar to that reported in the literature.2, 5, 9 The frequency and distribution of tumor diagnosis and their association with age is in accordance with past studies that too have demonstrated a relatively higher frequency of vascular and lacrimal gland tumors among operable orbital neoplasms.3, 5, 9, 10, 11, 12, 13 Proptosis is the commonest presentation reported in orbital tumors, and in our series the mean proptosis is quite similar to previous data.3, 14, 15 In effect, our series is a universally representative sample of orbital tumors.
VA is significantly affected in eyes with orbital tumors.4, 5 The presenting acuity, as noted in our series, is dependent on the optic nerve compromise by its association with VER and color vision deficits. It is found to be unrelated to the duration of illness or amount of proptosis. In our study, the trend of change of VA after surgery supports current literature.3, 5 We too noted a transient or permanent postoperative decline in VA.16, 17 It is evident from the above studies that those cases that involved a large posterior tumor or excessive surgical manipulation of the optic nerve were the ones more likely to suffer a permanent deterioration in VA. The case that showed a permanent decline of acuity in our series was a large meningioma with a 10-mm axial proptosis and a presenting VA of 20/30. We noted that in a majority of cases a transient decline in VA maximally improved during a 3-month follow up. Further, patients with a presenting acuity of 20/120 or worse did not improve significantly after surgery, unlike those with a mild decline in vision. We ascribe this to the fact that those with a good preoperative VA had tumors, which were unlikely to impinge on the optic nerve or orbital apex. The approach for surgery (either anterior or lateral orbitotomy) did not affect the VA outcome.
We illustrated a significant difference between the refractive error of the proptosed eye and the fellow eye, with the tumor eye showing more hyperopia and a significant postoperative improvement. In contrast to our findings, Friberg et al.3 found that extraconal tumors actually caused a myopic shift in refraction that decreased after surgery, which they attributed to the compression of the globe from the side and consequential elongation. Intraconal lesions showed a sudden and larger change in refractive error after surgery than extraconal tumors and, we believe, this is a direct result of the loss of posterior pole indentation. The maximal refractive error change took place within the first month after surgery.
The astigmatism induced by orbital tumors has only been studied in capillary hemangiomas in children.4, 18 The corneal curvature changes observed in our cases are secondary to either the pressure effect of the tumor or effect of the lid and prolonged exposure due to proptosis. In a study it was found that despite the removal of a long-standing cavernous hemangioma there was a persistent flattening of the posterior pole, which was attributed to scleral remodeling.19 It is possible that a similar mechanism may have a role in the corneal tissue. Also in support are studies that found no difference in the pre- and postoperative keratometry after orbital decompression for thyroid eye disease.20, 21 The amount of astigmatism induced is dependent on the location of the tumor, but not on the amount of proptosis or duration of illness.
The most common fundus findings described are choroidal folds, disc pallor, disc edema, and vascular tortuousity.5, 7, 22 The presenting VA is significantly affected by the presence of disc changes on fundus whereas choroidal folds did not hamper it. The postoperative visual outcome also followed suit. In our group of patients, we found a significant relation between the presence of fundus changes and the refractive error of the patient. Hyperopia in the pre- and postoperative period in proptosed eyes with fundus changes may be explained by the presence of a larger tumor, which is more likely to indent the globe. In our study, there is only partial reversal of choroidal folds after surgery and scleral remodeling may elucidate this.19
Color vision changes are known to precede VA changes in disc edema. Color vision in our study was found to be significantly associated with fundus changes and a poorer presenting VA. An orbital space-occupying lesion causes a compression effect on the optic nerve, even if not directly impinging on the nerve, resulting in a neuropathy presenting with poor VA, color vision deficits, and disc changes. The non-reversibility of color vision observed points toward a permanent neuronal damage, and hence a color vision deficit at presentation is a marker for poorer prognosis. Current literature lacks substantial prospective data on color vision changes in orbital tumors.
The commonest change on GVF testing was an expansion of the field as a consequence of the eye being proptosed beyond the confines of the orbital rim. A constriction of field noted in some eyes could be due to either a mechanical ptosis or a non-axial proptosis. Central or centrocaecal scotomas marked optic nerve involvement. Visual fields had been previously studied in orbital tumors using automated perimetry by Wei et al6 in 22 patients with field alterations varying from arcuate to inferior altitudinal, centrocaecal scotomas to temporal hemianopsia or a diffuse defect. The unique finding of an expanded visual field has not been reported in the study as it used standard automated perimetry protocols. Postoperatively, there was a loss of the panoramic field though it did not possess a functional significance.
Our study demonstrated significant VER changes. VER has been shown to mirror optic nerve compromise in orbital tumors.7, 23 The relief of orbital compression after surgery caused an improvement in both amplitude and latency, resulting in the improvement of linked parameters, namely fundus changes and VA. VER amplitude abnormalities did not show a clinically significant reversal after surgery; therefore, any clinically relevant change noted preoperatively was predictive of a poorer visual outcome and prognosis. VER latency changes demonstrated a moderately strong correlation with presenting VA, but failed to show a similar correlation in the postoperative period, thereby rendering it as a weak predictor of final visual outcome.
This study involves a heterogeneous group of orbital tumors. To analyze visual function changes and prognostic factors for specific tumors would be inappropriate because of the small individual numbers involved. The paper discusses the effect that an orbital space-occupying lesion would cause on visual parameters and visual outcome. Though not noted in our cases, postoperative chemotherapy and radiotherapy may have a confounding effect during longer follow-up.
To conclude, we found significant affliction of various visual function parameters due to orbital tumors. These parameters are an interrelated web and changes in one of these got reflected onto another factor. Changes observed in color vision, keratometry, and VER amplitude did not show a significant improvement after surgery. The visual outcome depends on the preoperative VA, amount of proptosis at presentation, degree of hyperopia induced, and presence of clinically significant VER changes. The presenting VA in turn depends on the presence of color vision abnormalities, disc changes on ophthalmoscopy, and a prolonged VER latency.
We recommend a comprehensive preoperative evaluation, including keratometry, color vision testing, visual fields, and a VER to help prognosticate the visual outcome. A longer follow-up study needs to be undertaken to ascertain definitely the behavior and reversibility of visual function changes.

References
Sunderraj P . Malignant tumours of the eye and adnexa. Indian J Ophthalmol 1991; 39: 6–8.
Gogi R, Nath K, Ahuja L, Shukla M . Ocular and adnexal tumours. Indian J Ophthalmol 1979; 27: 25–28.
Friberg TR, Grove AS . Choroidal folds and refractive errors associated with orbital tumors. Arch Ophthalmol 1983; 101: 589–603.
Dubois J, Milot J, Jaeger BI, McCuaig C, Rousseau E, Powell J . Orbital and eyelid hemangiomas: is there a relationship between location and ocular problems? J Am Acad Dermatol 2006; 55: 614.
Sharma V, Betharia SM . Prospective evaluation of fundus changes in patients with orbital mass lesions. Retina 2006; 26: 415–421.
Wei R, L Y, Zhou Y . Automated perimetry analysis of optic nerve compression caused by orbital tumors and tumor-like lesions. 1997; 33: 33–35.
Brecelj J, Stirn-Kranjc B, Skrbec M . Visual electrophysiology in children with tumours affecting the visual pathway: Case reports. Doc Ophthalmol 2000; 101: 125–154.
Oken BS, Chiappa KH, Gill E . Normal temporal variability of the P100. Electroencephalogr Clin Neurophysiol 1987; 68: 153–156.
Nath K, Gogi R . Primary orbital tumours. Indian J Ophthalmol 1977; 25: 10–16.
Ohtsuka K, Hashimoto M, Suzuki Y . Review of 244 orbital tumors in Japanese patients during a 21 year period: origin and locations. Jpn J Ophthalmol 2005; 49: 49–55.
Shields JA, Shields CL, Scartozzi R . Survey of 1264 patients with orbital tumors and simulating lesions: The 2002 Montgomery Lecture, part 1. Ophthalmology 2004; 111: 997–1008.
Bajaj MS, Pushker N, Chaturvedi A, Betharia SM, Kashyap S, Balasubramanya R et al. Orbital space-occupying lesions in Indian children. J Pediatr Ophthalmol Strabismus 2007; 44: 106–111.
Viswanathan S, George S, Ramadwar M, Shet T, Arora B, Laskar S et al. Extraconal orbital tumors in children—A spectrum. Virchows Arch 2009; 454: 703–713.
Masud MZ, Babar TF, Iqbal A, Khan MT, Zaffar ul Islam, Khan MD . Proptosis: etiology and demographic patterns. J Coll Physicians Surg Park 2006; 16: 38–41.
Ben Simon GJ, Yoon MK, Atul J, Nakra T, McCann JD, Goldberg RA . Clinical manifestations of orbital mass lesions at the Jules Stein Eye Institute. 1999–2003. Ophthalmic Surg Lasers Imaging 2006; 37: 25–32.
Sulimma F, Lieb WE . Orbital surgery: perioperative problems and results problems and results. Ophthalmologe 1999; 96: 724–727.
Park HJ, Yang SH, Kim IS, Sung JH, Son BC, Lee SW . Surgical treatment of orbital tumors at a single institution. J Korean Neurosurg Soc 2008; 44: 146–150.
Robb RM . Refractive errors associated with hemangiomas of the eyelids and orbit in infancy. Am J Ophthalmol 1977; 83: 52–58.
Wu J, Lai TF, Leibovitch I, Selva D . Persistent posterior globe flattening after orbital cavernous haemangioma excision. Clin Experiment Ophthalmol 2005; 33: 424–425.
Chandrasekaran S, Petsoglou C, Billson FA, Selva D, Ghabrial R . Refractive change in thyroid eye disease (a neglected clinical sign). Br J Ophthalmol 2006; 90: 307–309.
Sagili S, DeSousa JL, Malhotra R . Intraocular pressure and refractive changes following orbital decompression with intraconal fat excision. Open Ophthalmol J 2008; 2: 73–76.
Cockerham KP, Cockerham GC, Stutzman R, Hidayat AA, Depper MH, Turbin RE et al. The clinical spectrum of schwannomas presenting with visual dysfunction: a clinicopathologic study of three cases. Surv Ophthalmol 1999; 44: 226–234.
Janáky M, Benedek G . Visual evoked potentials during the early phase of optic nerve compression in the orbital cavity. Doc Ophthalmol 1992; 81: 197–208.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Singh, D., Pushker, N., Bajaj, M. et al. Visual function alterations in orbital tumors and factors predicting visual outcome after surgery. Eye 26, 448–453 (2012). https://doi.org/10.1038/eye.2011.308
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.308
Keywords
This article is cited by
-
Stereotactic radiosurgery for orbital cavernous venous malformation: a single center’s experience for 15 years
Acta Neurochirurgica (2021)
-
Post-operative optical coherence tomography angiography features of chorioretinal folds resulting from pleomorphic adenoma of the lacrimal gland (PALG) of orbit- a case report
BMC Ophthalmology (2020)
-
Biometric and refractive changes after orbital decompression in Korean patients with thyroid-associated orbitopathy
Eye (2016)