Abstract
Purpose
To explore a modified technique for silicone intubation for the repair of canalicular lacerations.
Methods
The surgery was performed on 35 eyes in 35 adult patients from October 2007 to September 2009. Using a modified soft probe, silicone tubes were inserted through the lacrimal punctum and left in the bicanaliculi for 3–10 months.
Results
The surgery was performed successfully in all cases. The tubes were removed after 3–10 months (mean 5.3±1.8 months). The mean follow-up time after tube removal was 13.8 months (range, 6–22 months). Lower punctum splitting occurred in one case (2.86%) after the surgery. No other complications associated with the silicone tubes occurred. All the tubes were removed successfully without any difficulty. No iatrogenic injuries occurred during tube removal.
Conclusions
The modified bicanalicular intubation procedure described here is an effective and atraumatic procedure for the management of canalicular lacerations in adults, and it is associated with fewer complications than the traditional sutures of canalicular lacerations.
Similar content being viewed by others
Introduction
Canalicular lacerations are a common injury of the canalicular system. The key step during surgery for the treatment of canalicular laceration is to identify the site of trauma to the canaliculi. On the basis of the canalicular anatomy and microscopic magnification, locating the damaged end of the canaliculi has become simpler.1 To ensure the normal function of the injured canaliculi after healing, the placement of a silicone tube in the canalicular system has been recommended as a surgical stent during the healing process.2 The temporary stent intubation could prevent canalicular obstruction during recovery. The advantage of silicone intubation is that it can restore a normal anatomical pathway rather than creating a bypass.3 Different surgical procedures, such as the pigtail probe, have been introduced to intubate the silicone tube into the canalicular system to repair canalicular lacerations.4, 5 However, these procedures are regarded as having some limitations and disadvantages. Accordingly, more effective and less invasive methods of silicone tube insertion for the treatment of canalicular lacerations are needed. Herein, based on our previous studies,3, 6 we describe a modified bicanalicular intubation (MBCI) technique for the treatment of canalicular laceration.
Materials and methods
Patients
A total of 35 eyes from 35 patients (28 males and 7 females) underwent canalicular intubation from October 2007 to September 2009 in the Zhongshan Ophthalmic Center, Sun Yat-sen University. The age ranged from 18 to 59 years (mean age 31.86 years). The duration from the time of canalicular injury to the surgery ranged from 2 h to 7 days. The diagnosis of canalicular laceration was based on an ophthalmological examination, which is illustrated in Figure 1. Among the 35 eyes, 29 (82.9%) had lower canalicular lacerations, 4 (11.4%) had upper canalicular lacerations and 2 (5.7%) had bicanalicular lacerations. The study and data collection were carried out with the approval of the Ethics Committee and institutional review board of the Zhongshan Ophthalmic Center of Sun Yat-Sen University. A consent form was obtained from each patient before the surgery.
Surgical procedures
Based on the procedures described in our previously published studies,3, 6 a modified soft probe (Figure 2) consisting of a segmental epidural catheter with a blind tip and a stainless steel acupuncture needle (the needle point was cutoff and the tip was burnished) was inserted into the lumen of the proximal part of the catheter to increase its rigidity before inserting the soft probe.
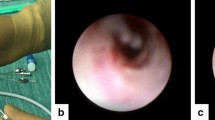
The procedure was performed under local infiltration anesthesia with 2% lidocaine hydrochloride. The inferior nasal meatus was treated twice with a pledget soaked in 0.5% proparacaine hydrochloride eye drops (Alcon Laboratories Inc., Fort Worth, TX, USA) and 1% ephedrine hydrochloride solution. Two soft probes were prepared for bicanalicular intubation (BCI), and a silicone tube (the tip had a 0.30-mm inner diameter, and the middle had a 0.60-mm outer diameter; therefore, the tip was smaller than middle part) was used as a lacrimal stent. After locating the cut end of the laceration, two catheters were inserted into the inferior and superior lacrimal system (the punctum, canaliculus, lacrimal sac, and nasolacrimal duct). Additionally, blind tip of the epidural catheter was put through the lacrimal punctum and the proximal of the canalicular laceration >15 cm, whereas the distance between the lacrimal punctum and the cut end of the laceration was <5 mm. Then, the acupuncture needle through the side hole was placed to form ‘soft lacrimal probe’. Then inserted into the lacrimal sac and nasolacrimal duct (Figure 3a). A snare device made of an epidural tube was inserted into the inferior meatus of the nasolacrimal duct, and the catheters were inserted into the snare device. Then, the snare device was pulled smoothly, and the catheters were retrieved. The catheters could be more easily retrieved using a nasal endoscope (Figures 3b, c and 4a). After retrieval of the catheters, the two ends of the silicone tube were securely tied (end to end) to the catheters with 5-0 silk sutures. The silicon tube outside the nostril formed a U-shape. Then, a 1-0 silk suture (20 cm long) was coiled around the U-shaped silicone tube outside the nostril (Figure 4b). A small amount of ophthalmic ointment (tobramycin 0.3%, Zhongshan Ophthalmic center, Sun Yat-sen University, China) was applied to facilitate the tube pulling. Then, the catheters were pulled upward through the nasolacrimal duct, the lacrimal sac, the canalicular laceration and out from the inferior/superior punctum until the silicone tube was completely located in the canalicular system (Figure 4c). The catheters were cutoff of the silicone tube near the site of the connection (Figure 4d). Then, the BCI was established, two or three 5-0 polyglactin sutures were passed through the pericanalicular tissue in a horizontal mattress fashion, and the skin wound was closed with interrupted 7-0 polyglactin sutures. The two ends of the silicone tube were cut short ∼2 mm out of the lacrimal punctum and tied securely, end to end, with 5-0 silk sutures. Then, the joint of the silicone tube was rotated into the superior punctum using a blunt forceps, and the suture was pulled through the nostril (Figure 4e). The length of the tube between the upper and lower punctum was adjusted to ensure that no tension was present in the medial canthus, and the suture was removed through the nostril (Figure 4f). All patients were prescribed topical TobraDex eye drops (Alcon Laboratories Inc.) four times per day and antibiotics for 1 week. The skin sutures were removed 1 week after the surgery (Figure 5).
A diagram depicting the insertion of the tubes into the inferior meatus of the nasolacrimal duct. (a) The blind tip of the epidural catheter was put through the lacrimal punctum and the proximal of the canalicular laceration >15 cm, whereas the distance between the lacrimal punctum and the cut end of the laceration was <5 mm. Then, the acupuncture needle was placed through side hole to form ‘soft lacrimal probe’. (b) A snare device made from an epidural tube was inserted into the inferior meatus of the nasolacrimal duct. Next, the catheters were inserted into the snare device. (c) Then, the snare device was pulled smoothly, and the catheters were retrieved easily with the aid of a nasal endoscope.
The procedure of the MBCI technique for the treatment of canalicular lacerations. (a) Two catheters are inserted into the lacrimal system. (b) The silicon tube outside the opening of the nostril is formed into a U-shape. Then, a 1-0 silk suture (20 cm long) is coiled around the U-shaped silicon tube outside the nostril. (c) The catheters are pulled upward through the nasolacrimal duct, the lacrimal sac, the canaliculus and out from the inferior/superior punctum until the silicon tube is completely located in the canalicular system. (d) The two ends of the silicone tube are cut short, ∼2 mm out of the punctum, and tied securely with two pieces of 5-0 silk suture (end to end). (e) The length of the tube between the upper and lower punctum is adjusted to ensure that no tension is present in the medial canthus. (f) The location of the silicone tube after MBCI.
Removal of the silicon tube
The silicone tube was removed 3–10 months after MBCI, when the patients had experienced relief from tearing and irrigation through the free passage. A drop of topical ophthalmic anesthetic (0.5% proparacaine hydrochloride eye drops, Zhongshan Ophthalmic Center, Sun Yat-sen University, China) was instilled into the conjunctival sac. The tube loop (at the medial canthus) was rotated with small, blunt forceps until the joint of the tube was observed from the superior punctum. The loop between the superior punctum and joint was cut and pulled out from the medial canthus. Irrigation (with an antibiotic solution) was administered to the patients immediately after tube removal to clear the discharge in the lacrimal passage.
Results
MBCI was performed successfully in all eyes without any intraoperative complications during the procedure. The tubes were left in place for 3–10 months (mean 5.3±1.8 months) after the surgery. All the tubes were removed successfully in the outpatient department. The follow-up after tube removal ranged from 6 to 22 months (mean 10.7±4.1 months).
Irrigation of the lacrimal passages in all 34 eyes showed that they were free from obstruction. In total, 31 eyes (91.18%) achieved complete success (complete disappearance of epiphora after tube removal), and 3 eyes (8.82%) achieved partial success (some residual symptoms under irritating conditions, such as wind or winter weather). Postoperative tearing was found in three eyes, among which, two eyes had lower canalicular laceration and one eye had bicanalicular lacerations before surgery. Lower punctum splitting occurred in one case (2.86%) 1 month after the surgery, and the tubes in this patient were removed prematurely. This patient had recurrent epiphora 1 month after the tube removal. There were no other complications observed in this study.
Discussion
The canaliculi in the lids have little connective tissue compared with the medial and lateral tissues, making them particularly vulnerable to avulsion.7 Therefore, the canaliculi in the lids are susceptible to blunt trauma and sharp damage, which can cause local deformity and epiphora. It is necessary to repair the cut edges of the canaliculus as soon as possible. With the development of microsurgery, it has become easier to identify the cut end of the damaged canaliculus and suture the canalicular laceration. However, in cases of prolonged injury or severe damage of the canalicular tissue, it is difficult for surgeons to identify the cut ends. In our previous study (unpublished data), we developed a modified method to identify the cut end of the canaliculus more quickly and easily than the traditional method by using a modified soft probe system. The system consisted of a segmental epidural catheter with a blind tip (with a self-made side aperture 2.0 cm from the tail end), a stainless steel acupuncture needle (the needle point was cutoff and the tip was burnished) that was inserted into the lumen of the proximal part to increase the rigidity of the catheter before inserting the soft probe, and a syringe used to inject 0.3% Tobramycin Eye Ointment (Zhongshan Ophthalmic center, Sun Yat-sen University, China). In this study, all surgeries were performed by one surgeon who utilized a modified soft probe (5 cm long) (Figure 6a) to locate the lacerated medial cut end. The modified soft probe consisted of a segmental epidural catheter with the blind tip (with a self-made side aperture 1 cm from the tail end) and a stainless steel acupuncture needle that was inserted into the lumen of the proximal part to increase the rigidity of the catheter before inserting the soft probe. When the laceration occurred medially, identifying the medial end of the canaliculus was difficult, and a modified soft probe was inserted through the dilated ipsilateral intact punctum (for isolated lower canalicular lacerations, the uninjured upper punctum was used, and vice versa). The probe was passed from the uninjured punctum and canaliculus to the proximal end of the nasolacrimal duct through the common canaliculus and the lacrimal sac (Figure 6b). Then, the acupuncture needle was removed, and eye ointment was injected simultaneously so that it would be emitted from the injured canalicular distal end immediately after it filled the lacrimal sac (Figure 6c). Demonstrating the lumen of the cut end, a silicone tube was intubated through the exposed cut medial end. When the BCI was established, two or three 5-0 polyglactin sutures were passed through the pericanalicular tissue in a horizontal mattress fashion, and then the skin wound was closed with interrupted 7-0 polyglactin sutures.
The modified method to identify the cut end of the canaliculus. (a) A soft probe (5 cm long) is used to locate the lacerated medial cut end. (b) The probe is passed from the uninjured punctum and the canaliculus to the proximal end of the nasolacrimal duct through the common canaliculus and the lacrimal sac. (c) The acupuncture needle is removed, and oculentum is injected simultaneously until it is emitted from the injured canalicular distal end (once the lacrimal sac is full).
The injured canaliculus requires stenting of the holdfast to prevent canalicular obstruction. Silicone is the most widely used tubing material, and numerous surgical techniques have described how to insert a silicone tube to treat canalicular lacerations. These methods can be divided into monocanalicular intubation and BCI techniques. Monocanalicular intubation with Monoka tubes offers an alternative method for the treatment of monocanalicular lacerations.8 Recently, it has been reported that Mini-Monoka stent extrusions occur within 1 month and with an 11.1% extrusion rate, especially in upper canalicular lacerations, resulting in damage to the ocular surface. Therefore, this technique is not suitable for use in patients with combined upper and lower canalicular lacerations.9 BCI, which was developed by Crawford10 and Guibor11, involves the passage of the tube through the inferior and superior puncta and through the nasolacrimal drainage system into the nose, leaving a loop of tubing extending between the inferior and superior puncta. The approach has been widely adopted by many ophthalmologists owing to its simplicity, safety, efficacy, and minimal invasiveness. It can alleviate the tension on sutured tissues, can be used at the site of wound healing, and it is especially suitable for upper and lower canalicular lacerations. However, the traditional bicanalicular stent has some disadvantages, including the potential for damage to the normal nasolacrimal duct and the Hasner valve. To avoid the drawbacks mentioned above, a number of therapeutic developments have been reported recently, such as the use of a pigtail probe in this setting,8, 9, 12 but this technique is so difficult that its use has been discouraged because of possible damage to the common or uninjured canaliculus, leading to bypass formation, especially to the bicanalicular lacerations. To overcome the disadvantages of conventional BCI, improvements based on the use of silicone tubes have become increasingly important. In our previous study, we introduced a method of lacrimal system intubation and achieved a good result without iatrogenic injury.3, 6 However, the disadvantage still exist, for example, when the silicone tube entangle the blind tip of epidural catheter, retrograde traction is often caused by damage of the lacrimal. Second, the potential risks of the normal lacrimal punctum split and canalicular tear when soft lacrimal probe directly through the lacrimal punctum and traumatic canalicular, then enter the lacrimal sac vertically. In this study, we developed a modified method to insert the silicone tube for the treatment of canalicular lacerations.
We, for the first time, applied this technique in the treatment of canalicular lacerations in a total of 35 patients with canalicular lacerations, MBCI was found to be an effective technique with an anatomic success rate of 97.14%. Our findings demonstrated that the MBCI was a highly successful approach, providing complete epiphora relief in 31 eyes (88.57%), partial relief in 3 eyes (8.57%), and failure in 1 eye (2.86%). The MBCI was an effective procedure for treating canalicular lacerations with few complications.
Compared with the previous study, the MBCI achieved a relatively high success rate. This may be due to several factors. First, as shown in the Figure 3a, this method will not lead to tearing by generating tension for normal lacrimal punctum and the proximal canaliculus when soft lacrimal probe directly through the lacrimal punctum and traumatic canalicular, then enter the lacrimal sac vertically. Therefore, this technique could ensure clinical success and the integrity of the lacrimal punctum and proximal canaliculus. Second, restenosis of the canaliculus is the most common reason for failure. To reduce the risk of damage to the canalicular and puncta, in the connection of silicone tube and epidural catheter, the tip of silicone tube was smaller than the lumen of the epidural catheter. Thus, there was not iatrogenic injury occurred when the epidural was pulled up to drive the silicone tube through the lacrimal canaliculus retrogradely (Figure 4), ensuring that the silicone tube would proceed smoothly, avoiding iatrogenic injury and improving the success rate. Third, the silicone tube was only used with a soft probe, which minimized trauma to the healthy canalicular system rather than bypassing the lacrimal drainage passage. These features account for the minimal invasiveness of the technique and the lower rate of complications. Finally, in the MBCI, the silicone tube was placed to reconstruct the canalicular lacerations and was isolated from the lacrimal canaliculus intubation without disturbing the normal nasolacrimal duct and the Hasner valve. This ensured the normal function of the lacrimal duct and nasal cavity. Therefore, The MBCI could reduce the potential for discharge reflux from the nasal cavity along the tube.
In summary, MBCI is a novel, potentially effective approach for the treatment of canalicular lacerations. It can effectively recanalize the lacerations and restore the normal anatomical structure and physiological function of the canalicular system.
MBCI has a satisfactory success rate, it is minimally invasive, and it is associated with fewer complications. Therefore, it is a promising option for treating canalicular lacerations.

References
Cho SH, Hyun DW, Kang HJ, Ha MS . A simple new method for identifying the proximal cut end in lower canalicular laceration. Korean J Ophthalmol 2008; 22 (2): 73–76.
Forbes BJ, Katowitz WR, Binenbaum G . Pediatric canalicular tear repairs--revisiting the pigtail probe. J AAPOS 2008; 12 (5): 518–520.
Wang L, Chen D, Wang Z . New technique for lacrimal system intubation. Am J Ophthalmol 2006; 142 (2): 252–258.
Jordan DR, Nerad JA, Tse DT . The pigtail probe, revisited. Ophthalmology 1990; 97 (4): 512–519.
Saunders DH, Shannon GM, Flanagan JC . The effectiveness of the pigtail probe method of repairing canalicular lacerations. Ophthalmic Surg 1978; 9 (3): 33–40.
Chen D, Li N, Wan P, Xiao J, Liu Y, Wang X et al. A novel procedure for treating canalicular obstruction by re-canaliculisation and bicanalicular intubation. Br J Ophthalmol 2012; 96 (3): 366–369.
Wulc AE, Arterberry JF . The pathogenesis of canalicular laceration. Ophthalmology 1991; 98 (8): 1243–1249.
Lee H, Chi M, Park M, Baek S . Effectiveness of canalicular laceration repair using monocanalicular intubation with Monoka tubes. Acta Ophthalmol 2009; 87 (7): 793–796.
Reifler DM . Management of canalicular laceration. Surv Ophthalmol 1991; 36 (2): 113–132.
Crawford JS . Intubation of obstructions in the lacrimal system. Can J Ophthalmol 1977; 12 (4): 289–292.
Guibor P . Canaliculus intubation set. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol 1975; 79 (2): OP419–OP420.
Pecora JL . Pediatric nasolacrimal pigtail probes. Ophthalmic Surg 1980; 11 (4): 249.
Acknowledgements
This study was supported by the Projects of Science and Technology Research of Guangdong Province, China (no. 2011B080701033, LXW) and the China Postdoctoral Science Foundation (no. 20110490962, LNY).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Liang, X., Lin, Y., Wang, Z. et al. A modified bicanalicular intubation procedure to repair canalicular lacerations using silicone tubes. Eye 26, 1542–1547 (2012). https://doi.org/10.1038/eye.2012.212
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2012.212