Abstract
Purpose
To evaluate the changes in the best-corrected visual acuity (BCVA) after 1 year and after ≥5 years after macular translocation for age-related macular degeneration (AMD) or myopic choroidal neovascularisation (mCNV).
Methods
The medical records of 61 consecutive patients who underwent macular translocation with 360° retinotomy for AMD (35 eyes) or mCNV (26 eyes) were reviewed. Overall, 40 patients, 17 mCNV and 23 AMD, were followed for at least 5 years. BCVA and area of the Goldmann visual field (VF) measured before, 12 months after surgery, and at the final visit.
Results
In the 23 AMD eyes followed for ≥5 years, the mean preoperative BCVA was 1.149±0.105 logMAR units, which significantly improved to 0.69±0.06 logMAR units at 1 year (P<0.001). This BCVA was maintained at 0.633±0.083 logMAR units on their final examination. In the 17 eyes with mCNV followed for ≥5 years, the mean preoperative BCVA was 1.083±0.119 logMAR units, which was significantly improved to 0.689±0.121 logMAR units at 1 year (P=0.001). This BCVA was maintained at 0.678±0.142 logMAR units on their final examination. The area of the VF was significantly decreased at 12 months and did not change significantly thereafter.
Conclusions
Our results show that macular translocation surgery significantly improves the BCVA and significantly decreases the VF area of eyes with mCNV or AMD after first 1 year. The BCVA and VF area do not change significantly from the values at 1 year for at least 5 years.
Similar content being viewed by others
Introduction
Age-related macular degeneration (AMD) is the leading cause of legal blindness in the elderly of industrialised countries.1 There are two types of AMD; the dry type and the wet type. The wet type is associated with subretinal choroidal neovascularisation (CNV). High myopia can also lead to visual reductions and development of a CNV (myopic CNV (mCNV)).2
At present, an intravitreal injection of anti-vascular endothelial growth factor is generally used to treat CNVs. However, if the retinal pigment epithelium (RPE) underlying the fovea is damaged, the effectiveness of this therapy on the visual acuity (VA) is limited. To overcome this problem, new therapies such as RPE cell transplantation and transplantation of stem cells are being tried.3,4
Macular translocation surgery has also been used to treat AMD. In this surgery, the macular area is moved from the underlying damaged RPE to an area of healthier RPE.5,6,7 This technique involves the detachment of the entire retina from the RPE by a subretinal infusion of fluid followed by an axial rotation of the macula.8,9,10,11,12 Although this surgery improves the VA after 1 to 2 years,8,9,11,13,14,15 it is rarely performed now because of the difficult surgical procedures and the production of severe strabismus. However, the long-term results of this surgery have provided important information on whether an impaired sensory retina moved onto healthy RPE can recover and maintain good visual function for long periods.
The outcome of macular translocation surgery for AMD is still controversial. Most studies have reported favourable outcomes but for follow-up periods of ≤2 years after the surgery.9,11,12,15,16,17,18,19,20 On the other hand, there are two reports on the visual outcome of macular translocation surgery with follow-up periods of ≥3 years,21,22 and the visual outcomes were reported to be poor in both. However, in these two reports, the visual improvement was not attained even in the first year. In the other study, 32 patients were studied retrospectively, but one-third of the patients were not included in the analyses because they were not followed for more than 5 years.21 Thus, this study may have excluded patients that may have good vision if followed longer. For eyes with a mCNV, the findings ≥5 years after macular translocation surgery were presented but the results of only five cases were reported.22
We have recorded focal electroretinograms from the translocated macular area and found it was significantly better than that before operation at 22 months postoperatively.18,20 However, the results after longer follow-up periods have not been reported.
Thus, the purpose of this study was to determine the visual outcomes ≥5 years after macular translocation surgery with 360° retinotomy in eyes with mCNV or AMD.
We analysed all 61 patients 1 year after macular translocation surgery, and separately analysed 40 of these patients who were followed for ≥5 years.
Patients and methods
This research was conducted in accordance with the Institutional Guidelines of Nagoya University and conformed to the tenets of the World Medical Association Declaration of Helsinki.
Patients
Macular translocation surgery was performed on one eye of 62 patients with a subfoveal CNV at the Nagoya University Hospital from February 2000 to July 2004. An informed consent was obtained from each patient for the surgery after they were provided information on other treatment options including photocoagulation, removal only, and observation only. Because one patient developed dementia and could not return to our hospital after discharge, the results from 61 eyes from 61 patients were analysed. There were 35 patients with AMD (26 men and 9 women) and 26 patients with mCNV (5 men and 21 women). The mean age at operation was 73.0±6.5 years with a range of 62–87 years in the eyes with AMD and 62.6±9.7 years with a range of 40–77 years in eyes with a mCNV (Tables 1 and 2). The mean size of the lesion was 3890±1164 μm with a range of 1060–6947 μm in the eyes with AMD and 2511±832 μm with a range of 1248–4190 μm in the eyes with a mCNV. All patients were Japanese, and they were followed for a mean of 67.5±25.9 months with a range of 15–105 months. Three patients were followed for 15, 18, and 18 months, and all others were followed for at least 24 months.
Overall, 23 AMD patients and 17 mCNV patients were followed for ≥5 years. The type of AMD was predominantly classic in 16 eyes, minimally classic in 5 eyes, and occult with no classic signs in 14 eyes.
The patients’ medical records were reviewed, and the best-corrected VA (BCVA) and the area of the visual field (VF) before, 12 months after surgery, and at the final examination were analysed. The BCVA was measured with a standard Japanese VA chart in decimal units and converted to the logarithm of the minimal angle of resolution (logMAR) units for statistical analyses. The BCVAs expressed in logMAR units are shown in Table 1. When the change of the BCVA was ±>2 logMAR units, the change was taken to be significant.
The VFs were determined by Goldmann perimetry (with V-4), and the area of the VF in degrees2 was measured with the SCION Image software (NIH, Bethesda, MD, USA). When the VF area changed by ±>30%, it was taken to be a significant decrease.
Surgical techniques
Initially, a pars plana posterior lensectomy was performed followed by pars plana vitrectomy. After the vitrectomy, four separate dome-shaped retinal detachments (RDs) were created by subretinal injections of saline solutions. This was followed by fluid–air exchange of the vitreous to induce a total RD. After a 360° retinotomy at the ora serrata, the CNV was removed and heavy perfluorocarbon liquid was injected into the vitreous. Then, the entire detached retina was rotated around the optic disc axis. The holes made for the 360° retinotomy were sealed by endophotocoagulation, and the perfluorocarbon liquid was replaced by silicone oil. The silicone oil was removed after several months, and an intraocular lens was implanted in patients who requested the implantation.18,19,20
The data are presented as the means±SEMs. Wilcoxon signed-rank t-tests with the Bonferonni correction were used to compare the BCVA and area of the visual VF before, 12 months after surgery, and at the final examination. P-values <0.017 were taken to be statistically significant.
To identify the factors that might influence the final BCVA, multiple regression analyses were performed with the final BCVA as the dependent variable. The independent variables were the gender, age, type of AMD, the preoperative BCVA and at 1 year, >5 years, CNV size at surgery, postoperative complications, and duration of follow-up. Regression analyses were also performed with the improvement of BCVA as the dependent variable.
All statistical analyses were performed using the SPSS software version 19 (SAS Institute, Cary, NC, USA).
Results
Surgical results and complications
The macula was successfully translocated in all eyes. The postoperative complications included rhegmatogenous RD in one AMD and three mCNV cases, and a macular hole (MH) in three mCNV eyes with two complicated by a RD. The macula on the new RPE cells was detached in all eyes. Vitrectomy was performed on these patients to reattach the retina. Aseptic endophthalmitis developed in one mCNV eye and was treated with antibiotics and cyclosporine, and secondary glaucoma developed in one mCNV eye that required trabeculectomy. A CNV recurred in five AMD eyes and one mCNV eye at the previously affected foveal area, and these were treated with radiation, CNV removal surgery, photocoagulation, or photodynamic therapy. Proliferative vitreoretinopathy did not occur in any eye.
A RD and a MH developed significantly more frequently in mCNV eyes than in AMD eyes (P=0.014; χ2-test), but the rate of recurrence of CNV was not significantly different in the two types of eyes (P=0.175: χ2-test).
BCVA in eyes with AMD
The BCVAs of the 35 eyes of patients with AMD before surgery, 12 months after surgery, and at the last follow-up examination (15 months to >5 years) are plotted in Figures 1a and b. The BCVA at 12 months of 19 of 35 eyes (54.3%) was significantly improved and that of the other 16 eyes were not changed significantly from the baseline BCVA. At the last examination (15–105 months), the BCVA had improved significantly in 5 eyes (14.3%), worsened significantly in 1 eye (2.8%), and did not change significantly in 29 eyes (82.9%) from the BCVA at 1 year.
Effect of macular translocation surgery on the BCVA in the AMD eyes. Overall, 23 eyes were followed for ≥5 years (filled circle) and 12 eyes were followed for <5 years (open circle). Scatter plots of the BCVA before and 12 months after surgery (a) and at the final examination (b) are shown. The BCVA is plotted in logMAR units. The mean BCVA of the 35 eyes examined (open circle) and that of the 23 eyes followed for ≥5 years months (filled circle) are shown (c). The BCVA improved significantly at 12 months and did not decrease significantly thereafter. The error bars represent the SEMs. *P=0.01, **P<0.001 by Wilcoxon's signed-rank test.
Before surgery, the mean BCVA was 1.128±0.075 logMAR units in the 35 AMD eyes and 1.149±0.105 logMAR units in 23 eyes followed for ≥5 years. At 12 months, the mean BCVA was 0.724±0.049 logMAR units in the 35 eyes and 0.690±0.064 logMAR units in the 23 eyes followed for ≥5 years. At the last examination, the mean BCVA was 0.657±0.060 logMAR units in the 35 AMD eyes and 0.633±0.083 logMAR units in the 23 eyes followed for ≥5 years (Figure 1c).
The improvement in the BCVA at 12 months was significant for the 35 eyes (P<0.001) and also for the 23 eyes followed for ≥5 years. The BCVA did not decrease significantly after 1 year (P=0.010 for the 35 AMD eyes; Figure 1c).
The last BCVA was significantly associated with the BCVA at 12 months but not significantly associated with the gender, age, type of AMD, preoperative BCVA, CNV size at surgery, postoperative complications, and duration of follow-up. Spearman's rank correlation coefficient showed that the BCVA at the last examination was significantly correlated with the BCVA at 12 months (r=0.791; P<0.001) but not with that before surgery.
The improvement of the BCVA at the 12 months was significantly associated with the preoperative BCVA, but not significantly associated with the gender, age, CNV size at surgery, postoperative complication, or duration of follow-up. Spearman's rank correlation coefficient also showed that the improvement of BCVA at the 12 months was significantly correlated with the BCVA before surgery (r=−0.598; P<0.001).
BCVA in myopic eyes with choroidal neovascularisation
The BCVAs of the 26 eyes with a mCNV before surgery, 12 months after surgery, and at the last follow-up examination are plotted in Figures 2a and b. At 12 months, the BCVA of 19 of 26 eyes (73.1%) had a significant improvement of the BCVA, 2 eyes (7.7%) had a worsening, and 5 eyes (19.2%) remained unchanged. At the last examination (15 months to >5 years), the BCVA had improved significantly in 4 eyes (15.4%), worsened in 2 eyes (7.7%), and remained stable in 20 eyes (76.9%) compared with that at 1 year.
Effect of macular translocation surgery on the BCVA in myopic eyes with a CNV. Overall, 17 eyes were followed for ≥5 years (filled circle) and 9 eyes were followed for <60 months (open circle). Scatter plots of the BCVA before and 12 months after surgery (a) and at the final examination (b) are shown. The BCVAs are plotted in logMAR units. The mean BCVA of the 26 eyes (open circle) and that of 17 eyes followed for ≥5 years (filled circle) are shown (c). The BCVA significantly improved at 12 months and was stable thereafter. The error bars represent the SEMs. *P=0.001, **P<0.001 by Wilcoxon's signed-rank test.
The mean preoperative BCVA was 1.074±0.085 logMAR units in the 26 mCNV eyes and 1.083±0.119 logMAR units in the 17 eyes followed for ≥5 years. At 12 months, the mean BCVA was 0.733±0.099 logMAR units in the 26 eyes and 0.689±0.121 logMAR units in the 17 eyes followed for ≥5 years. At the last examination (15 months to 5 years), the BCVA was 0.689±0.105 logMAR units in the 26 mCNV eyes and 0.678±0.142 logMAR units in the 17 eyes followed for ≥5 years (Figure 2c).
The improvement of the BCVA at 12 months was significant for the 26 eyes (P<0.001) and also for the 17 eyes followed ≥5 years (P=0.001), and this was maintained thereafter (P=0.206 and P=0.721, respectively; Figure 2c).
The last BCVA was significantly associated with the BCVA at 12 months (P<0.001). However, it was not significantly associated with the gender, age, CNV size at surgery, postoperative complications, BCVA before surgery, or duration of follow-up. Spearman's rank correlation coefficient showed that last BCVA was significantly correlated with the BCVA before surgery (P=0.003, r=0.561), and the improvement of BCVA at 1 year was significantly correlated with the BCVA before surgery (P=0.033, r=−0.420).
Changes in area of VF
We measured the VFs of the 35 AMD eyes and the 26 eyes with a mCNV. The mean VF area of eyes with AMD and with mCNV before surgery, 12 months after surgery, and at the final examination are shown in Figure 3. Before surgery, the mean VF area was 11110±218 μm2 in the AMD patients and 9833±412 μm2 in the mCNV patients. At 12 months after surgery, it was 8948±332 μm2 in the AMD patients and 7076±423 μm2 in the mCNV patients. At the last examination, the mean VF area was 8358±417 μm2 in the AMD patients and 6930±532 μm2 in the mCNV patients.
The area of the VF was significantly smaller at 12 months in both the AMD (P<0.001) and mCNV (P<0.001) eyes. The area of the VF did not change significantly in both types of patients thereafter (P=0.726 and P=0.280, respectively). Eight mCNV eyes (20.8%) and 13 AMD eyes (37.1%) showed a significant decrease in the VF area, and the other 40 eyes did not change significantly.
Discussion
Our findings showed that the BCVAs of eyes with AMD or mCNV were significantly improved by macular translocation surgery after 12 months. The improved BCVA was maintained even after ≥5 years. From 12 months after surgery to the final examination, only two mCNV eyes and one AMD eye had a decrease of >2 logMAR lines in the BCVA. The other eyes improved significantly (four myopic and five AMD) or did not change significantly during this period.
For mCNV, Fujii et al23 reported that 4 of 11 eyes showed a significant improvement of ≥2 Snellen lines and 4 eyes remained unchanged 9.8 months after macular translocation surgery. Fujikado et al24 reported that 8 of 11 eyes had an improvement of greater than 0.2 logMAR units, and only 1 eye had a decrease of 0.2 logMAR units 6.2 months after translocation surgery. Our results at 12 months are consistent with these findings. Yamada et al22 reported that the mean BCVA before operation was maintained until the final follow-up in five of five myopic cases after a mean follow-up time of 6.5 years.
For AMD patients, Mruthyunjaya et al15 reported that better preoperative BCVA was significantly associated with better postoperative BCVA at 12 months. Our results are also consistent with theirs, that is, there was a significant association between the preoperative BCVA and improvement of the BCVA in eyes with AMD.
There are more than 10 studies on the visual outcome of macular translocation surgery for eyes with AMD with follow-up periods of <2 years, and most of these showed a significant improvement or unchanged BCVA.9,11,12,15,16,17,18,19,20 Our findings are consistent with these reports, and our results for the 35 AMD eyes showed that the mean BCVA improved from 1.128±0.075 to 0.724±0.049 logMAR units at 12 months and did not worsen at the final examination even after follow-up periods of ≥5 years.
For AMD patients, there are two reports with a follow-up of >5 years. In one study, Yamada et al22 reported that the BCVA was not significantly changed at 1 year and significantly worsened after >5 years. These differences from our findings could be because the preoperative BCVA was worse in their patients than ours. In addition, five of their patients developed postoperative proliferative vitreoretinopathy. However, they stated that the retinopathy was treated successfully, and there was no difference in the BCVA between the eyes with complications from those without complications. Our multiple regression analyses showed that the final BCVA was not significantly associated with the kind of complications.
The fact that Yamada et al22 analysed only two-thirds of the patients (n=32 analysed) operated on can be another reason for the differences. Because the other third were not followed for >5 years, they were not included in the analyses. It is possible that patients with good BCVA stopped coming to the hospital and were not followed for a long period. To exclude this possibility, we analysed the results of all the patients who had undergone macular translocation surgery and separately for the 40 patients who were followed for ≥5 years. However, the results of these two analyses were similar; both showed an improvement of the BCVA at 12 months and no significant changes thereafter. Thus, a decrease in the BCVA was not found in our cases at 12 months. Although the reason for the differences in visual outcome at the earlier times are not known, our results suggest that if the outcome is good at 12 months, the final BCVA will be good at 5 years.
The mean follow-up period after macular translocation surgery was 38.2 months in the study by Aisenbrey et al,21 and 52 of their patients (57.8%) were followed for ≥3 years and 25 patients (27.8%) were followed for ≥5 years. At 36 months, 75% of their patients had stable or significantly improved BCVA. These findings are not different from our results at 12 months in our patients. They also stated that the patients who were followed for a short period did not show better outcome, and those who were followed for a long period did not show worse outcome. These findings are consistent with our multiple regression results that the follow-up period was not significantly associated with the final BCVA.
Because macular translocation surgery damages the retina, for example, artificial RD and rotation of the retina, it was expected that the area of the VF would be reduced. However, the VF was not significantly decreased after 12 months, suggesting that the surgical procedures may not be harmful to the retina.
In conclusion, the changes in the visual function of eyes with mCNV and AMD after macular translocation surgery with 360 retinotomy were analysed. Although there are some limitations in this study, related to its retrospective nature, we have found that this surgery can improve the BCVA in the first 12 months, and the BCVA is maintained for ≥5 years. The survival of retinal function on the new RPE for long period is important for future treatments of CNVs, such as RPE cell transplantation.

References
Klein R, Klein BE, Linton KL . Prevalence of age-related maculopathy. The Beaver Dam Eye Study. Ophthalmology 1992; 99: 933–943.
Chan WM, Ohji M, Lai TY, Liu DT, Tano Y, Lam DS . Choroidal neovascularisation in pathological myopia: an update in management. Br J Ophthalmol 2005; 89: 1522–1528.
Du H, Lim SL, Grob S, Zhang K . Induced pluripotent stem cell therapies for geographic atrophy of age-related macular degeneration. Semin Ophthalmol 2011; 26: 216–224.
Falkner-Radler CI, Krebs I, Glittenberg C, Povazay B, Drexler W, Graf A et al. Human retinal pigment epithelium (RPE) transplantation: outcome after autologous RPE-choroid sheet and RPE cell-suspension in a randomised clinical study. Br J Ophthalmol 2011; 95 (3): 370–375.
Machemer R, Steinhorst UH . Retinal separation, retinotomy, and macular relocation: II. A surgical approach for age-related macular degeneration? Graefes Arch Clin Exp Ophthalmol 1993; 231: 635–641.
Machemer R, Steinhorst UH . Retinal separation, retinotomy, and macular relocation: I. Experimental studies in the rabbit eye. Graefes Arch Clin Exp Ophthalmol 1993; 231: 629–634.
Anonymous. American Academy of Ophthalmology. Macular translocation. Ophthalmology 2000; 107: 1015–1018.
Eckardt C, Eckardt U, Conrad HG . Macular rotation with and without counter-rotation of the globe in patients with age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 1999; 237: 313–325.
Aisenbrey S, Lafaut BA, Szurman P, Grisanti S, Lüke C, Krott R et al. Macular translocation with 360 degree retinotomy for exudative age-related macular degeneration. Arch Ophthalmol 2002; 120: 451–459.
Ohji M, Fujikado T, Kusaka S, Hayashi A, Hosohata J, Ikuno Y et al. Comparison of three techniques of foveal translocation in patients with subfoveal choroidal neovascularization resulting from age-related macular degeneration. Am J Ophthalmol 2001; 132: 888–896.
Pertile G, Claes C . Macular translocation with 360 degree retinotomy for management of age-related macular degeneration with subfoveal choroidal neovascularization. Am J Ophthalmol 2002; 134: 560–565.
Lai JC, Lapolice DJ, Stinnett SS, Meyer CH, Arieu LM, Keller MA et al. Visual outcomes following macular translocation with 360-degree peripheral retinectomy. Arch Ophthalmol 2002; 120: 1317–1324.
Toth CA, Freedman SF . Macular translocation with 360-degree peripheral retinectomy impact of technique and surgical experience on visual outcomes. Retina 2001; 21: 293–303.
Abdel-Meguid A, Lappas A, Hartmann K, Auer F, Schrage N, Thumann G et al. One year follow up of macular translocation with 360 degree retinotomy in patients with age related macular degeneration. Br J Ophthalmol 2003; 87: 615–621.
Mruthyunjaya P, Stinnett SS, Toth CA . Change in visual function after macular translocation with 360 degrees retinectomy for neovascular age-related macular degeneration. Ophthalmology 2004; 111: 1715–1724.
Fujikado T, Asonuma S, Ohji M, Kusaka S, Hayashi A, Ikuno Y et al. Reading ability after macular translocation surgery with 360-degree retinotomy. Am J Ophthalmol 2002; 134: 849–856.
Toth CA, Lapolice DJ, Banks AD, Stinnett SS . Improvement in near visual function after macular translocation surgery with 360-degree peripheral retinectomy. Graefes Arch Clin Exp Ophthalmol 2004; 242: 541–548.
Terasaki H, Miyake Y, Suzuki T, Niwa T, Piao CH, Suzuki S et al. Change in full-field ERGs after macular translocation surgery with 360° retinotomy. Invest Ophthalmol Vis Sci 2002; 43: 452–457.
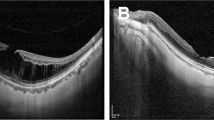
Terasaki H, Ishikawa K, Suzuki T, Nakamura M, Miyake K, Miyake Y . Morphologic and angiographic assessment of the macula after macular translocation surgery with 360° retinotomy. Ophthalmology 2003; 110: 2403–2408.
Terasaki H, Ishikawa K, Niwa Y, Piao CH, Niwa T, Kondo M et al. Changes in focal macular ERGs after macular translocation surgery with 360 degrees retinotomy. Invest Ophthalmol Vis Sci 2004; 45: 567–573.
Aisenbrey S, Bartz-Schmidt KU, Walter P, Hilgers RD, Ayertey H, Szurman P et al. Long-term follow-up of macular translocation with 360° retinotomy for exudative age-related macular degeneration. Arch Ophthalmol 2007; 125: 1367–1372.
Yamada Y, Miyamura N, Suzuma K, Kitaoka T . Long-term follow-up of full macular translocation for choroidal neovascularization. Am J Ophthalmol 2010; 149: 453–457.
Fujii GY, Humayun MS, Pieramici DJ, Schachat AP, Au Eong KG, de Juan Jr E . Initial experience of inferior limited macular translocation for subfoveal choroidal neovascularization resulting from causes other than age-related macular degeneration. Am J Ophthalmol 2001; 131: 90–100.
Fujikado T, Ohji M, Kusaka S, Hayashi A, Kamei M, Okada AA et al. Visual function after foveal translocation with 360-degree retinotomy and simultaneous torsional muscle surgery in patients with myopic neovascular maculopathy. Am J Ophthlmol 2001; 131: 101–110.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Takeuchi, K., Kachi, S., Iwata, E. et al. Visual function 5 years or more after macular translocation surgery for myopic choroidal neovascularisation and age-related macular degeneration. Eye 26, 51–60 (2012). https://doi.org/10.1038/eye.2011.302
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.302
Keywords
This article is cited by
-
The role of indocyanine green angiography imaging in further differential diagnosis of patients with nAMD who are morphologically poor responders to ranibizumab in a real-life setting
Eye (2016)
-
Prospects for clinical use of reprogrammed cells for autologous treatment of macular degeneration
Fibrogenesis & Tissue Repair (2015)
-
Displacement of foveal area toward optic disc after macular hole surgery with internal limiting membrane peeling
Eye (2013)