Abstract
Purpose
To compare the topographic features of eyes treated with photorefractive keratectomy (PRK) for myopia using two different excimer lasers.
Methods
A total of 65 eyes in 39 patients treated with PRK (6.0-mm optical zone) using Technolas 217C and VISX S4 excimer lasers were evaluated retrospectively to determine the size of the topographic ablation zone.
Results
The zones ablated using the VISX S4 had shorter diameters in both axes (−0.89±0.73, −1.59±0.49 mm; both P=0.00), whereas those ablated using the Technolas 217C had a longer diameter in the major axis (0.96±0.63 mm; P=0.00) and a shorter diameter in the minor axis (−0.39±0.59 mm; P=0.00). The theoretical ablated zone was a circle with a diameter of 6.0 mm. The Technolas 217C group tended to have oval cuts in comparison with the VISX S4 group, and the difference between the programmed (6.0 mm) and topographic diameters was significant in both groups.
Conclusions
There was a difference between the programmed and postoperative topographic diameters of the ablation zone. The postoperative ablation zone differed in shape and size according to the type of excimer laser.
Similar content being viewed by others
Introduction
Photorefractive keratectomy (PRK) and laser in situ keratomileusis (LASIK) can correct myopia and myopic astigmatism.1, 2, 3, 4 Despite the high success rate, decreased vision, such as glares or halos, in a dark environment can occur in patients undergoing excimer laser refractive surgery. Many studies have explained this phenomenon using the disparity between the scotopic pupil size and the optical zone,5, 6, 7 although some studies have found no correlation between the scotopic pupil size and night vision complaints.8, 9 As the expanding transition zone may decrease night vision complaints,8 in addition to the programmed optical zone and preoperative scotopic pupil size, the size of the transition peripheral zone should be considered previously to identify the cause of night vision problems.
The ablation zone tends to be smaller than the programmed ablation zone after refractive surgery. Recent reports suggest that the difference between the programmed and actual diameters of the optical zone also depends on the type of excimer laser system.10, 11 This difference prevents one from obtaining the best postoperative result, despite selecting an appropriate optical zone. This study evaluated the characteristics and differences of the topographic ablation zones produced using two different excimer laser systems and assessed the difference between the programmed and postoperative topographic diameters with each system.
Patients and methods
A retrospective analysis was made of 65 eyes in 39 patients who were diagnosed with myopia or myopic astigmatism and underwent PRK. The operations were performed using a Technolas 217C excimer laser in 34 eyes in 20 patients at Ajou University Hospital (by J Ahn) and using a VISX STAR S4 laser with an EK fixation device12 in 31 eyes in 19 patients at Severance Hospital (by EK Kim). Eyes with previous ocular surgery, underlying ocular or systemic disease, a programmed optical zone other than 6.0 mm, significant postoperative corneal haze, or a postoperative uncorrected visual acuity (UCVA) of less than 20/25 were excluded from this study.
The programmed ablation zone was 6.0 mm. We defined the programmed ablation zone as the ablation zone diameter determined by the operator, not the ablation zone calculated by the excimer laser machines. Therefore, the programmed ablation zone was fixed at a 6.0 mm diameter, excluding the transition or blending zones.
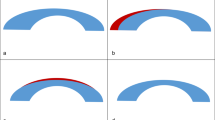
All eyes underwent corneal topography using an Orbscan II (Bausch and Lomb) at the preoperative evaluation and at 3 months postoperatively, and a difference map between the pre- and postoperative anterior tangential maps was obtained using a program in Orbscan II (Bausch and Lomb). According to several studies that determined ablation centration based on the corneal topography,13, 14, 15 the ablation zone on corneal topography was defined as the area including the blue central circle surrounded by the green area (Figure 1). Using the method described by Coorpender et al,16 a transparent grid was placed on the difference map. Then, the lengths of the topographic ablation zone were measured at the zone of lowest curvature on the difference map (confluent blue zone). We defined the longest and shortest diameters as the major and minor axes, respectively.
We compared the two axes of the topographic ablation zone with the programmed ablation zone diameter (6.0 mm) in the Technolas 217C and VISX STAR S4 laser groups (Figure 2). In addition, we compared the two axes of the postoperative topographic ablation zone between the two different laser systems.
Difference maps for the Technolas 217C (left) and VISX STAR S4 (right) laser systems, created using Orbscan II corneal topography (1 D colour steps). The ablation zone was defined as the central confluent blue zone surrounded by the green area. In the Technolas 217C difference map (left), the long axis length was 6.4 mm, and the short axis length was 5.1 mm. In the VISX STAR S4 difference map (right), the long axis length was 4.4 mm, and the short axis length was 3.9 mm.
Statistical analysis was performed using SPSS 12.0, and P<0.05 was considered statistically significant. An independent sample t-test was used to compare the programmed and topographic ablation zones in each group and between groups. The Pearson's correlation test was used to evaluate the relationship between the spherical equivalent and the topographic ablation zone diameter.
Results
The mean age of the patients was 28.6±4.78 years (mean±SD) in the Technolas group and 27.9±6.45 years in the VISX S4 group. The mean preoperative spherical equivalents were −4.47±0.69 (−5.88 to −3.00) and −4.49±1.31 (−6.50 to −1.25) dioptres (D) in the Technolas and VISX S4 groups, respectively. The mean postoperative UCVA values were 0.98±0.07 and 0.98±0.06, respectively. The mean age, mean preoperative spherical equivalent, and postoperative UCVA did not differ between the two groups (Table 1).
There was a significant difference in the size of the ablation zone programmed preoperatively vs that measured postoperatively at the 3-month follow-up between the excimer laser systems. The major and minor diameters of the postoperative ablation zone were both shorter than the programmed ablation zone diameter in the VISX Star S4 group (−0.89±0.73 and −1.59±0.49 mm), whereas the major axis was longer (0.96±0.63 mm) and the minor axis was shorter (−0.39±0.59 mm) than those of the programmed ablation zone in the Technolas 217C group (Table 2). The major diameter of the postoperative ablation zone was longer in the Technolas 217C group than that in the VISX Star S4 group (6.96±0.63 vs 5.11±0.73 mm, P<0.001). In addition, the minor diameter of the postoperative ablation zone was longer in the Technolas 217C group than that in the VISX Star S4 group (5.61±0.59 vs 4.41±0.49 mm, P<0.001).
The difference between the lengths of the major and minor axes showed that the cut tended to be oval with the Technolas 217C (1.34±0.47 mm) and VISX S4 (0.81±0.44 mm). The effect was significantly greater in the Technolas 217C group (P<0.001).
We considered the preoperative spherical equivalent to be a factor affecting the difference between the programmed ablation zone and topographic optical zone. Statistical analysis using the Pearson's correlation test revealed no significant correlation between the groups (P>0.05).
Conclusion
We evaluated the difference between the programmed ablation zone and the postoperative topographic ablation zone resulting from the use of two different excimer lasers in PRK patients.
In a study of LASIK using VISX S2, Partal et al11 stated that the postoperative topographic optical zone (6.0±0.2 mm, 5.5±0.5 mm) was smaller than the programmed ablation zone (6.5 mm) and that this reduction seemed to be independent of the degree of myopia. Similar to Partal et al, we found that both the major and minor axes diameters of the postoperative topographic ablation zone were shorter than the programmed ablation zone diameter in the VISX S4 group. In the Technolas 217C group, the major axis diameter of the postoperative topographic ablation zone was longer than the programmed ablation zone diameter, whereas the minor axis diameter was shorter.
Canals et al10 found large differences in the superficial dimensions and contours of the ablations produced by different excimer lasers using a polymethylmethacrylate plate covered with thin aluminium foil and a 6.0-mm programmed ablation zone. The Technolas 217C had an oval central area (5.96 × 8.73 mm), and the VISX S4 had slightly smaller, round central area (5.52 × 5.84 mm). Our postoperative values are similar to those of Canals et al, but the zone diameters are smaller, suggesting that wound remodelling occurred at 3 months in our human study.
The postoperative topographic ablation zone was defined as the area including the blue central circle surrounded by green area. However, this has topographic meaning only, and no clinical or real corneal meaning. Many authors have defined the optical zone using various methods.17, 18, 19 Although it is likely that the topographic ablation zone adopted in our study is proportional to the size of the real optical zone, the effective optical zone (the zone with the attempted correction) may be by far smaller.17 Therefore, further studies should examine the clinical correlation.
Twa et al20 compared similar laser systems (VISX S3 vs B&L 217C) using wavefront analysis and psychophysical testing in addition to corneal topography.20 Interestingly, they found greater spherical aberration for the VISX laser. In addition, many studies have explained night halos and glare using the disparity between the scotopic pupil size and optical zone,5, 6, 7 so the difference between the programmed ablation zone and postoperative topographic ablation zone might explain this phenomenon. Therefore, it is necessary to study the relationship between a patient's symptoms and the disparity of the postoperative topographic ablation zone.
The ablation depth may affect the size of the postoperative ablation zone, although we found no correlation between the preoperative spherical equivalent and the postoperative topographic ablation zone. Therefore, the relatively wide range of preoperative refractive error (−1.25 to −6.50 D) may be a limitation of our study.
In conclusion, there is a difference between the programmed and postoperative topographic diameters of the ablation zone that depends on the excimer laser system, and the postoperative ablation zones differ in shape and size between the two laser systems. Therefore, the postoperative ablation zone should be considered when determining the programmed ablation zone.
References
Hersh PS, Stulting RD, Steinert RF, Waring III GO, Thompson KP, O’Connell M et al. Result of phase 3 excimer laser photorefractive keratectomy for myopia. Ophthalmology 1997; 104: 1535–1553.
McDonald MB, Deitz MR, Frantz JM, Kraff MC, Krueger RR, Salz JJ et al. Photorefractive keratectomy for low-to-moderate myopia and astigmatism with a small-beam, tracker-directed excimer laser. Ophthalmology 1999; 106: 1481–1489.
Pop M, Payette Y . Photorefractive keratectomy versus laser in situ keratomileusis: a control-matched study. Ophthalmology 2000; 107: 251–257.
Litwak S, Zadok D, Garcia-de Quevedo V, Robledo N, Chayet AS . Laser-assisted subepithelial keratectomy versus photorefractive keratectomy for the correction of myopia: a prospective comparative study. J Cataract Refract Surg 2002; 28: 1330–1333.
Tahzib NG, Bootsma SJ, Eggink FA, Nabar VA, Nuijts RM . Functional outcomes and patient satisfaction after laser in situ keratomileusis for correction of myopia. J Cataract Refract Surg 2005; 31: 1943–1951.
Schallhorn SC, Kaupp SE, Tanzer DJ, Tidwell J, Laurent J, Bourque LB . Pupil size and quality of vision after LASIK. J Cataract Refract Surg 2003; 110: 1606–1614.
Fan-Paul NI, Li J, Miller JS, Florakis GJ . Night vision disturbances after corneal refractive surgery. Surv Ophthalmol 2002; 47: 533–546.
Macsai MS, Stubbe K, Beck AP, Ravage ZB . Effect of expanding the treatment zone of the Nidek EC-500 laser on laser in situ keratomileusis outcomes. J Cataract Refract Surg 2004; 30: 2336–2343.
Pop M, Payette Y . Risk factors for night vision complaints after LASIK for myopia. Ophthalmology 2004; 111: 3–10.
Canals M, Elies D, Costa-vila J, Coret A . Comparative study ablation profiles of six different excimer lasers. J Refract Surg 2004; 20: 106–109.
Partal AE, Manche EE . Diameters of topographic optical zone and programmed ablation zone for laser in situ keratomileusis for Myopia. J Refract Surg 2003; 19: 528–533.
Kim EK, Lee DH, Park JW, Chu YK, Seo KY . New fixation device for photorefractive surgery and its effect on corneal epithelial wound healing. J Refract Surg 1999; 15: 594–601.
Mulhem MG, Foley-Nolan A, O’Keefe M, Condon PI . Topographical analysis of ablation centration after excimer laser photorefractive keratectomy and laser in situ keratomileusis for high myopia. J Cataract Refract Surg 1997; 23: 488–494.
Tsai YY, Lin JM . Ablation centration after active eye-tracker-assisted photorefractive keratectomy and laser in situ keratomileusis. J Cataract Refract Surg 2000; 26: 28–34.
Giaconi JA, Manche EE . Ablation centration in myopic laser in situ keratomileusis comparing the VISX S3 Active Trak and the VISX S2. J Cataract Refract Surg 2003; 29: 1522–1529.
Coorpender SJ, Klyce SD, McDonald MB, Doubrava MW, Kim CK, Tan AL et al. Corneal topography of small-beam tracking excimer laser photorefractive keratectomy. J Cataract Refract Surg 1999; 25: 675–684.
Roberts CW, Koester CJ . Optical zone diameters for photorefractive corneal surgery. Invest Ophthalmol Vis Sci 1993; 34: 2275–2281.
Boxer Wachler BS, Huynh VN, El-Shiaty AF, Goldberg D . Evaluation of corneal functional optical zone after laser in situ keratomileusis. J Cataract Refract Surg 2002; 28: 948–953.
Holladay JT, Janes JA . Topographic changes in corneal asphericity and effective optical zone after laser in situ keratomileusis. J Cataract Refract Surg 2002; 28: 942–947.
Twa MD, Lembach RG, Bullimore MA, Roberts C . A prospective randomized clinical trial of laser in situ keratomileusis with two different lasers. Am J Ophthalmol 2005; 140: 173–183.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented as a poster at the 93rd Annual Meeting of the Korean Ophthalmological Society, Busan, Korea, April 2005. Conflict of interest: None. Financial interest: This work was supported by ‘GRRC’ project of Gyeonggi Provincial Government, Korea and by the ‘National Research Foundation of Korea (NRF) grant funded by the Korea government (MEST) (No.M1AQ19, 2009-0082186)’
Rights and permissions
About this article
Cite this article
Ahn, J., Yang, H., Lew, H. et al. Comparison of the topographic ablation zone after photorefractive keratectomy for myopia using two different excimer lasers. Eye 24, 553–557 (2010). https://doi.org/10.1038/eye.2009.169
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.169
Keywords
This article is cited by
-
Six modes of corneal topography for evaluation of ablation zones after small-incision lenticule extraction and femtosecond laser-assisted in situ keratomileusis
Graefe's Archive for Clinical and Experimental Ophthalmology (2020)