Abstract
Newborn screening (NBS) programs aim to identify affected infants before the onset of treatable disorders. Historically, benefits to the family and society were considered secondary to this clinical benefit; yet, recent discourse defending expanded NBS has argued that screening can in part be justified by secondary benefits, such as learning reproductive risk information to support family planning (‘reproductive benefit’). Despite increased attention to these secondary benefits of NBS, stakeholders’ values remain unknown. We report a mixed methods study that included an examination of providers’ views toward the pursuit of reproductive risk information through NBS, using sickle cell disorder carrier status as an example. We surveyed a stratified random sample of 1615 providers in Ontario, and interviewed 42 providers across 7 disciplines. A majority endorsed the identification of reproductive risks as a goal of NBS (74–77%). Providers’ dominant rationale was that knowledge of carrier status is an important and inherent benefit of NBS as it allows people to make reproductive choices, which is consistent with the goals of disease prevention. However, some challenged its appropriateness, questioning its logic, timing and impact on disease prevention. Others were sensitive to intruding on individuals’ choices or children's independent rights. While the dominant view is consistent with discourse defending expanded NBS, it deviates from the traditional screening principles that underpin most public health interventions. Broader discussion of the balance between benefits to screened individuals and those to families and societies, in the context of public health programs, is needed.
Similar content being viewed by others
INTRODUCTION
Population screening programs have traditionally been guided by principles that prioritize the opportunity to identify and treat individuals early in an effort to reduce morbidity and mortality.1 This goal has formed the cornerstone of deciding whether or not to introduce (or modify) a screening intervention. Other benefits to families or society can also be realized through screening and are valued, yet have typically been considered secondary to the primary clinical benefit for the individual screened, and in most cases do not provide warrant for the intervention itself.2 Yet, newborn screening (NBS) is a model case where the previously considered secondary benefits are gaining prominence and increasingly included as a justification to expand screening programs.3
The scope of NBS programs, intended to identify infants affected with treatable diseases before the onset of symptoms, has been expanding around the world. This expansion has been fuelled by a number of factors, most notably advances in technology, which have enabled the screening of additional disorders with minimal additional, up-front costs. Some of the conditions included in expanded NBS panels, however, are not accompanied by treatments for which there is clear evidence of effectiveness.4 In this context, there is increased attention to the additional benefits that might be realized, such as the opportunity to inform individuals, both parents and the infant, about the reproductive risks they may face.5, 6 Historically, ‘reproductive benefit’ – that is, the benefit of learning reproductive risk information that may support family planning – arose as an outcome secondary to the primary goal of identifying a treatable condition. Yet, recent discourse defending expanded NBS has argued that screening can be justified, at least in part, by secondary benefits, and reproductive benefit specifically.5, 6, 7, 8, 9
Reproductive benefit can be realized as one of the primary benefits of NBS in several ways. The first is when expanded NBS panels include conditions for which clear evidence of treatment is not established,4 such that the identification of reproductive risks becomes one of the main assured benefits of screening.5, 8 A second way pertains to conditions, such as Duchenne muscular dystrophy, for which there is currently no curative treatment available and where early diagnosis is intended to permit the early identification of reproductive risks.10 Finally, NBS can also detect healthy infants who are carriers; routine disclosure of this incidental information can alert parents and children of their reproductive risks. Sickle cell disorders (SCD) provide an illustrative case.
Screening for SCD is justified by evidence that prophylactic treatment with penicillin results in reduced mortality in affected infants.11, 12 However, screening technologies that detect affected infants also identify virtually all SCD carriers. SCD carrier status is considered to be clinically benign under normal physiological conditions,13 but confers a 25% risk of having an affected offspring when both parents are SCD carriers. The question of whether and how carrier status should be disclosed has challenged policymakers who struggle to reconcile the delivery of preference-sensitive information about reproductive risks within the context of population-based interventions that typically operate through mandatory or implied consent models, as is the case for NBS.14, 15 We sought to inform this policy issue by consulting with health-care providers (HCPs) – stakeholders whose expertize often informs decisions regarding the expansion of NBS programs, but whose opinions on these issues remain largely unknown.
METHODS
Study design
We conducted a mixed methods study to examine the views of HCPs, consumers and advocates on the management of infant carrier status information generated through NBS for SCD in Ontario. The study was approved by the Hamilton Health Sciences Research Ethics Board. Previous articles from this study explored providers’ views about consent for NBS16, their role in informing parents about NBS before sample collection17 and their reasoning about managing carrier status results.18 Another article reported a qualitative exploration of the meanings attributed to SCD carrier status by HCPs, consumers and advocates, some of which challenge conventional interpretations of its health significance.19 Here, we report on the survey and interview data pertaining to the attitudes and rationales of HCPs regarding the reproductive significance of carrier status generally and SCD carrier status specifically (excluding any arguments about its clinical significance), and the pursuit of reproductive benefit through NBS.
Sample recruitment
Interview participants were purposively sampled key informants across seven provider disciplines known to be interested in the expansion of NBS or actively involved with the SCD community; and, individuals identified or referred by their professional group or survey respondents who expressed an interest in participating in follow-up interviews. The final sample included: seven family physicians, nine genetic professionals (genetic counsellors, medical and biochemical geneticists), three hematologists, six midwives, nine maternal/newborn nurses, three obstetricians and five pediatricians.
The survey respondents consisted of a stratified random sample of HCPs from seven disciplines involved in the clinical provision of NBS or interpretation of results: family physicians (n=729), genetic professionals (n=105), hematologists (n=148), midwives (n=339), maternal/newborn nurses (n=725), obstetrician/gynecologists (n=498) and pediatricians (n=569). Names and addresses of respondents were obtained from various lists (eg, MDSelect, the Canadian Medical Directory, and other clinician-specific associations).
Data collection
Interview questions
Semi-structured, open-ended interviews were conducted to explore providers’ attitudes and rationales regarding: (1) how to manage the SCD carrier results generated through NBS; (2) whether consent is required for carrier result disclosure and (3) assuming these results would be disclosed, how should carrier results be disclosed.
Survey measures and administration
A cross-sectional survey of 3113 HCPs in Ontario was conducted in 2007 using a mailed self-administered questionnaire. Following the Dillman tailored design method,20 up to five contacts were made; this has been described in detail elsewhere.16, 17, 18, 19
The survey instrument was developed by a multi-disciplinary team, based on a literature review and pretested among 2–3 members from each provider group to assess face and content validity. In addition to questions pertaining to whether SCD carrier status should be routinely disclosed through NBS,18 the questionnaire collected information about HCPs’ views on the purposes of NBS.
Data analysis
Interviews were transcribed verbatim and managed on NVivo software (version 7, QSR International, Cambridge, MA, USA). Transcripts were coded by two team members and analyzed using a modified grounded theory approach,21 incorporating principles of constant comparison and qualitative description.22 Codes pertaining to the generation of reproductive risk information through NBS were analyzed to identify the main arguments supporting (or questioning) the pursuit of reproductive benefit through NBS. Thematically, coherent arguments were identified and then fully described to capture underpinning values or judgments. Emerging reasoning was then contrasted with existing data and judgements, and summarized below as rationales in favor of or questioning the pursuit of reproductive benefit through NBS.
We calculated the proportion of respondents who agreed with the various goals presented using descriptive statistics. Likert items were converted into dichotomized variables. The χ2 test was used to assess differences across provider groups. We considered two-sided P-values of 0.05 or less to indicate statistical significance. Data were managed and analyzed using SPSS 16.0.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Study participants
Of the 3113 surveys distributed, 1615 providers returned a completed questionnaire, representing an uncorrected response rate of 51.9%. After adjusting for ineligible respondents who did not provide care for patients with SCD or families in the NB period, or who were no longer in practice or could not be contacted despite repeated efforts, our corrected response rate was 62.9% (adjusted N=2569; 54.1% of obstetrician/gynecologists, 76.7% of midwives, 72.6% of nurses, 50.6% of family physicians, 63.1% of pediatricians, 68.0% of genetics professionals and 51.9% of hematologists).
A description of our survey and interview respondents has been provided elsewhere.16, 17, 18, 23 Briefly, the majority of our survey respondents were female (73.1%). The number of years providers had been in practice was evenly distributed: 22.9% were in practice 0–5 years, 20.9% for 6–10 years, 25.1% for 11–20 years and the remaining 31.1% for over 20 years. The majority of providers were located in a metropolitan/central city (67.9%), and work in non-academic settings (74.8%) (Table 1). The majority of our interview respondents were female (n=28/42; 66.7%).
Interview findings
We identified two main rationales in the qualitative analysis, one dominant and one minor. The dominant rationale involved enthusiasm for the idea that knowledge of carrier status is an important and necessary benefit of NBS, as it allows people to make reproductive choices. The minor rationale was critical of the presumption that the identification of reproductive risks through the disclosure of carrier status is a benefit of NBS for SCD, and questioned the appropriateness of using NBS as a means to inform reproductive decision making.
Enthusiasm toward pursing reproductive benefit through NBS (dominant rationale)
Participants who supported the disclosure of reproductive risk information through NBS articulated two arguments to support their position: (1) identification of reproductive risk through NBS is an important and inherent consequence of NBS and (2) in turn, the disclosure of reproductive risk information facilitates disease prevention, which is one of the main goals of NBS.
First, these HCPs considered the generation of reproductive risk information as an important benefit of NBS as it allows people to make reproductive choices. One HCP outlined how carrier disclosure would translate into a benefit for the parents in particular:
By detecting this (carrier status) and finding out (if) the partner also has it… could affect reproductive behavior. (Hematologist (#8))
Inherent in the argument that the generation of reproductive risk information is a benefit of NBS is the assumption that parents would want to know the information in their reproductive decisions: ‘Parents want to know (yeah) I think parents want to know.’ (Nurse (#7)) Further, HCPs reasoned that genetic information necessarily affects other family members, making it difficult to limit the benefits of NBS to the screened infants:
I think we recognize the importance (of carrier information) for that baby's future reproductive decisions. It's important. I think that's been established. So by all means for the parents that (information) also has implications, that's at the heart of what genetics is about. So I, I think yeah there's definite justification and value in having the information for that purpose … there's really no way of separating those two things. Basically, you have the result and you have it for multiple family members to use in different ways. To pursue that additional testing of the parents or you know whatever else that would be. (Geneticist (#31))
Thus, for these proponents, the goal of NBS inherently extends beyond solely seeking clinical benefit for the screened infant, to offering reproductive benefits to other family members, which are considered important and desirable consequences of NBS.
Some HCPs considered informing parents of their reproductive risks to be a form of disease prevention and one of the main goals of NBS. Indeed, for some participants, the clinical goals of NBS were ‘less important than’ reproductive benefit:
Identifying somebody who actually has a disease to me is probably even less important than actually trying to prevent the disease… That may not be the original purpose or what the original purpose of newborn screening but again newborn screening was set up around PKU and hypothyroidism so …. (Hematologist (#35))
Respondents characterized the identification of reproductive risk as a goal that aligns with the primary intent of NBS: a way to reduce the burden of the disease. NBS, they argued, provides an ‘opportunity to educate’ individuals of their reproductive risks toward the ultimate goal of reducing disease burden:
It's prevalent and to me it would be unthinkable if … (pause) … you have an opportunity … (pause) … to counsel and educate many more people with a view to reducing the burden of the disease in the future… So we are not, we are not going to impose (on parents’ reproductive decisions). I think that is an opportunity to educate. I think that in the long run we in the health-care system have a responsibility to seek ways to reduce the burden of the disease. (Hematologist (#8))
These HCPs assumed that informed parents would make choices to reduce the incidence of SCD – that the identification of carrier status is a route to reduced numbers of individuals with SCD:
So you need to know if you have the trait. That's how we’re going to reduce Sickle Cell. So this is. It's a preventive thing in that you know what you both have. You get counselling, genetic counselling so that you can make reproductive choices. We’re not telling you what you should do but you’ve made reproductive choices. (Nurse (#9))
The choices that HCPs emphasized included decisions about whom to marry, and stressed the importance of learning early enough to influence preconception decisions: ‘It is more likely that that information is going to become relevant to the child as an older child, before they enter marital relationships’ (Hematologist (#8)).
Many HCPs drew analogies to the Jewish experience with Tay-Sachs screening: ‘It's like Tay-Sachs gene in Jews. … you have the ability then to make decisions about your offspring and your partner.’ (Family Physician (#26))
Few HCPs were explicitly directive and would actively encourage people to avoid the birth of children with SCD, though there were some exceptions:
That is what we probably have to enforce, or, you know, have patience in our clientele, that this is something which is potentially, you know, if two heterozygotes get together and you have an affected child, talk about all the morbidity and mortality so I think it's maybe a little bit of the scare tactics would help, so that is the way I feel that it's something which is very important. (Pediatrician (#20))
Others clarified that identifying carrier status for the purpose of reproductive decision making does not have to lead to decisions to avoid such births. Decisions to have children with SCD were possible, and learning about reproductive risk information enabled preparation:
And then the more important thing is that even if you decide okay well it doesn’t matter I’m going to go have children, you’re aware of the possibility you may have a child with SCD so that you can then be prepared if you do end up with a child that you have some sort of information ahead of time that you might have a child with SCD. (Hematologist (#35))
Despite their views on the range of reproductive choices available, HCPs were clear that voluntarism must be maintained. They stressed that parents be allowed to choose how to make use of infants’ carrier status:
That decision should rest solely with them (parents). What the system should do is just provide the options that are available and let the family have the full confidence without any prejudice as to what option they choose. And they should understand that whatever option they choose the medical team and the health-care team should respect that. That's the fundamental principle. (Hematologist (#8))
However, they described providing the infant's carrier status to parents as information ‘they would need to know’ (Nurse (#39)). Indeed, participants did not anticipate that there was a choice to make with respect to receiving reproductive risk information, despite emphasizing the need for choice with respect to how to act on such information:
I think all we have to do is provide the information and discuss the information and I think parents decide to what extent they want (more) information. (Pediatrician (#10))
Thus, a distinction was implicitly drawn between the choices that would and would not be available to parents: whether or how to act on reproductive risk information was seen as a clear choice for parents to make, but whether to know these risks in the first instance was not necessarily seen as a matter of choice.
Questioning the pursuit of reproductive benefit through NBS (minor rationale)
While many HCPs saw potential benefits to individual families of knowing their reproductive risks, some also envisioned problems. These respondents questioned the appropriateness of using NBS as a mechanism to inform reproductive decision making. Their position centered on two arguments; they questioned: (1) the logic and feasibility of disease prevention through NBS and (2) the implications for communities and minors.
The first set of arguments raised by providers concerned the logic and feasibility of providing such information through the infant screening process. One provider asked: ‘Why are you screening babies in order to retrospectively, in essence, analyze the parents’ reproductive risk?’ (Geneticist (#6)). Others considered the pursuit of reproductive risk information through NBS as a ‘backdoor’ and inefficient way to inform parents:
I think it is a backdoor way of screening parents and if parents… if we think people ought to be making decisions about SCD and pregnancy, if folks want this information which I think for the most part they do, although as I mentioned I think the literature on whether they actually use it is limited. But it makes sense to screen parents, prospective parents during pregnancy as opposed to screening the babies and then saying that's a good way of informing parents about their risks. (Pediatrician (#6))
A number of respondents preferred the idea of offering a screening program to identify reproductive risks for hemoglobinopathies before or during pregnancy instead of, or as a necessary adjunct to, NBS for SCD. Providers who saw the benefits of an antenatal approach to the identification of reproductive risks for SCD (or the hemoglobinopathies as a whole) saw value in efforts to identify and help parents to manage reproductive risks. In addition to supporting an antenatal approach to identifying reproductive risks, this provider challenged the ability of parents to make active choices about reproduction if carrier status is automatically disclosed through NBS:
I think if Ontario wants to be in the business of preventing the future birth of children with anything, in this case SCD, when we have a very effective screening test then what we ought to be doing is putting dollars into preconceptual screening for those disorders. You wouldn’t need to think about whether you want to know your carrier status, that's already determined. What you would need to think about is, ‘Do I as an individual from this community, where there's a higher risk to be a carrier for ‘x’ do I want to be screened for that as I plan a pregnancy?’ Or even early in a pregnancy if that was an unplanned pregnancy. So that it just comes down to individual choice. Not individual knowledge that something was done before and I can make a choice whether or not to learn that information. (Geneticist (#37))
Others reflected on how disclosing carrier results would challenge individuals’ choices to learn of their reproductive risks. One provider pointed out that, for parents who have religious or other objections to antenatal screening, the disclosure of carrier status through NBS may also be problematic:
If they didn’t want to have children with SCD they could produce carriers or unaffected children but then you’d have to do the antenatal screening and from a religious point of view that might be challenging for families… So they might then choose not to procreate. (Nurse (#1))
These providers were also ambivalent about the likely success of disease prevention through the identification of reproductive risks. Some questioned whether professionals’ values about reproductive decisions were consistent with the values of the public. As this HCP put it, ‘medicine is dominated – and genetics in particular – by people from a specific social stratum with a relatively narrow range of values which they generalize to the population’ (Pediatrician (#3)). Others wondered whether disease prevention was feasible using reproductive risk information. One HCP recounted a personal story to illustrate how people do not necessarily govern their reproductive behaviors in a ‘rational’ manner when aware of their reproductive risks. Despite a lethal dominant genetic disease in the family, the couple chose to take their chances; the provider recalled how they’ve: ‘rolled the dice three times and three times we’ve been lucky’ (Health-care provider; Identification is withheld to preserve anonymity).
A second argument raised by providers involved questioning the implications of the pursuit of reproductive benefit through NBS for communities and minors. Some providers spoke about the ‘optics’ of state involvement in reproductive matters, especially for vulnerable communities. These potential harms were seen to involve stigmatization or discrimination (eg, in insurance, employment) of communities as a whole, and the potential for pressures on the community to avoid the birth of persons with SCD. Some providers were explicit that these hazards were racialized, deriving from the particular history and experience of the Afro-Caribbean community, and that community-focused efforts would be required. This HCP recounted the US history with SCD carrier screening:
The whole issue of testing and being identified either with the disease or more as a carrier and the negative sequelae that followed really created an air of mistrust that I think has lasted ‘til today and we can see it with a lot of the African-Americans in the States who don’t want to pursue breast cancer screening or testing because they feel that they’ll be marked in some way and so I think that that had a very long lasting negative impact… It was when the United States first implemented carrier screening for SCD and then the misunderstanding and the misinformation that was generated so that people were discriminated against both in employment and in insurance. People who were carriers and that created a lot of ill (will). (Geneticist (#40))
Some HCPs prioritized the rights of minors in advocating against identifying carriers through NBS. These HCPs considered carrier status disclosure an inefficient way to inform the infant and one that removes the choice of minors to remain ignorant of their carrier status. One provider reasoned that learning one's carrier status information should be an active choice and not ‘routine’:
I think it's okay that the general public doesn’t know the carrier status of their kids and the kids don’t know themselves. I think if they are older and they want to find out the results they should be able to but I don′t think it should be routine. (Obstetrician (#11))
Survey results
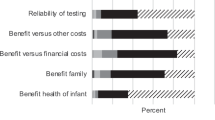
The majority of HCPs endorsed the goal of identifying the infant's carrier status (77.9% agree or strongly agree) and identifying the parent's reproductive risks (68.1% agree or strongly agree). There was less support for limiting screening to presymptomatic diagnosis only when treatment exists (56.5% agree or strongly agree), or for expanding screening to include presymptomatic diagnosis in the absence of treatment (55.8% agree or strongly agree) (Table 2).
The goals of NBS were valued differently among HCP groups (P<0.0001). Geneticists were least supportive of providing parents with their infants’ reproductive risk information as a goal of NBS (30.2%). Midwives were least supportive of the notion that providing parents with their own reproductive risk information is a goal of NBS (48.7%) (Table 2).
DISCUSSION
We found that a majority of HCPs endorsed identification of infants’ SCD carrier status and parents’ reproductive risks as a goal of NBS. This majority support was also evident in the dominant rationales made evident through qualitative interviews. Providers reasoned that knowledge of carrier status is an important and inherent benefit of NBS, as it allows people to make reproductive choices. Further, they argued that disease prevention is a main goal of NBS, which is facilitated by the disclosure of infants’ carrier status. Yet, contrary rationales were also evident, though to a lesser extent. Indeed, some providers challenged the appropriateness of the pursuit of reproductive benefit through NBS, questioning its logic and timing, as well as its impact on disease prevention. Further, some were sensitive to the ‘optics’ of state involvement in reproductive matters, especially for vulnerable communities, while others focused on the potential intrusion into individuals’ choices and children's independent rights. The difference of opinion derived, in part, from disagreement over what constituted harm, with some seeing the existence of even-subtle pressures to engage in rational reproductive decision making as harmful, and others seeing these encouragements as a clear benefit of NBS.
Debates over the notion of genetic prevention, and its role within the domain of public health, are longstanding within genetics. In an attempt to clarify these presumably distinct goals, Juengst24 distinguished between ‘phenotypic prevention’ and ‘genotypic prevention’, where the goal of the former is to prevent the clinical manifestation of a disease while the latter is focused on preventing the birth of people with particular genotypes. For most public health programs, these goals are kept distinct. Juengst cited NBS as an example of ‘phenotypic prevention’, distinguishing it from ‘genotypic prevention’ as characterized by reproductive risk reducing strategies for prospective parents. Yet, perhaps reflecting developments in NBS since Juengst wrote, infant screening is seen to serve both purposes by most providers in this study.
However, there are significant ethical challenges to pursuing reproductive benefit through NBS. In addition to the potential for misunderstanding and stigmatization that learning carrier state may engender,23 reproductive risk information is not typically available without informed consent,3 nor is it usually pursued in minors.25, 26 Historically, reproductive risk information has been provided through prenatal and adult carrier screening programs or through individual testing requested by families. Voluntarism and non-directive genetic counselling are characteristic hallmarks of these initiatives, which aim to facilitate informed decision making.27 Indeed, most preconception and prenatal guidelines require that individuals be given a ‘cascade of choices’, ensuring that each step in the decision-making process is well informed, from deciding whether to pursue information about reproductive risks to deciding how to manage it.9 Providers’ support of reproductive benefit as one of the primary goals of NBS and their expectation that reproductive risk information should be given to parents, without regard for their preference to know these risks, poses ethical challenges. The historic legacy of NBS is as a mandated (or implied consent) response to a perceived ‘public health emergency’.28 Given this service delivery context, the pursuit of reproductive benefit through NBS deviates from the prevailing policy guiding genetic testing or screening in minors as well as population screening for reproductive risk information in adults.3 To borrow and extend Juengst's24 argument, pursuing reproductive benefit through NBS conflates the goals of phenotypic and genotypic prevention and ‘is dangerous because it blurs the lines between medical interventions appropriate to prescribe to individuals and reproductive choices that should be theirs alone to make’.
Furthermore, the pursuit of reproductive benefit through NBS threatens to upset the traditional hierarchy of benefits that population screening programs seek to achieve.3 The overriding benefit pursued by screening interventions is in fact clinical benefit for individuals screened. Benefits to the family and society have been considered secondary, and in themselves do not provide warrant for public health interventions. Further, pursuing reproductive benefits through NBS in its historic mandatory or implied-consent structure is challenging.29 In essence, what began as a serendipitous ‘by-product’24 of NBS has been elevated within the hierarchy of goals, without sufficient clarity regarding how, or even whether, these should be pursued.
There are several caveats with the interpretation of our results. We describe the themes as ‘dominant’ and ‘minor’ to refer to their qualitative strength as dominant and minor thematic positions among providers, and not to their status as quantitative ‘majority’ or ‘minority’ opinions. In addition, the survey question from which the quantitative data were drawn was phrased in a normative manner; yet, it is possible that participants responded in a descriptive manner, reflecting on the current climate of NBS in Ontario. Further, it is possible that the respondents may have wanted to send a particular message, supporting a disclosure policy for SCD carrier status. This is especially plausible given the fact that SCD was already included in the Ontario panel and the survey was established to query the management of carrier results. Thus, despite our objective to explore the general purposes of NBS (beyond SCD), it may not be possible to generalize these findings beyond NBS for hemoglobinopathies, or similar disorders. Further research examining this issue with other disorders and stakeholders is thus warranted.
Despite these caveats, the qualitative and quantitative results align and suggest that most providers are supportive of the pursuit of reproductive benefit through NBS. They reasoned that its pursuit is consistent with the goals of disease prevention, which were considered as an important and inherent benefit of NBS. While these dominant views are consistent with discourse defending expanded NBS, they deviate from traditional screening principles that provide warrant for public health interventions that primarily seek clinical benefit. Broader discussion of these conflicts is needed to inform the balance between benefits to individuals and those to families and societies in the context of public health programs.
References
Wilson JMG, Jungner G : Principles and Practice of Screening for Disease. Geneva: World Health Organization, 1968.
Kass NE : An ethics framework for public health. Am J Public Health 2001; 91: 1776–1782.
Bombard Y, Miller FA, Hayeems RZ et al: The expansion of newborn screening: is reproductive benefit an appropriate pursuit? Nat Rev Genet 2009; 10: 666–667.
American College of Medical Genetics: Newborn Screening: Toward a Uniform Screening Panel and System. Bethesda: American College of Medical Genetics, 2005.
Alexander D, van Dyck PC : A vision of the future of newborn screening. Pediatrics 2006; 117: 350–354.
Bailey DBJ, Beskow LM, Davis AM, Skinner D : Changing perspectives on the benefits of newborn screening. Ment Retard Dev Disabil Res Rev 2006; 12: 270–279.
Health Council of the Netherlands: Screening: Between Hope and Hype. The Hague: Health Council of the Netherlands, 2008.
Bailey Jr DB, Skinner D, Warren SF : Newborn screening for developmental disabilities: reframing presumptive benefit. Am J Public Health 2005; 95: 1889–1893.
Bombard Y, Miller FA, Hayeems RZ, Avard D, Knoppers BM : Reconsidering reproductive benefit through newborn screening: a systematic review of guidelines on preconception, prenatal and newborn screening. Eur J Hum Genet 2010; 18: 751–760.
Ross LF : Screening for conditions that do not meet the Wilson and Jungner criteria: the case of Duchenne muscular dystrophy. Am J Med Genet A 2006; 140: 914–922.
US Preventive Services Task Force: Screening for Sickle Cell Disease in Newborns: U.S. Preventive Services Task Force Recommendation Statement. Rockville: Agency for Healthcare Research and Quality, 2007.
Davies S, Cronin E, Gill M, Greengross P, Hickman M, Normand C : Screening for sickle cell disease and thalassaemia: a systematic review with supplementary research. Health Technol Assess 2000; 4: 99.
National Heart Lung and Blood Institute: The Management of Sickle Cell Disease. National Institutes of Health: Division of Blood Diseases and Resources, 2002.
Mandl KD, Feit S, Larson C, Kohane IS : Newborn screening program practices in the United States: notification, research, and consent. Pediatrics 2002; 109: 269–273.
Hiller EH, Landenburger G, Natowicz MR : Public participation in medical policy-making and the status of consumer autonomy: the example of newborn-screening programs in the United States. Am J Public Health 1997; 87: 1280–1288.
Miller FA, Hayeems RZ, Carroll JC et al: Consent for newborn screening: The attutides of Health Care Providers. Public Health Genomics 2009; 13: 181–190.
Hayeems RZ, Miller FA, Little J et al: Informing parents about expanded newborn screening: influences on provider involvement. Pediatrics 2009; 124: 950–958.
Miller FA, Hayeems RZ, Bombard Y et al: Clinical obligations and public health programmes: healthcare provider reasoning about managing the incidental results of newborn screening. J Med Ethics 2009; 35: 626–634.
Miller FA, Paynter M, Hayeems RZ et al: Understanding sickle cell carrier status identified through newborn screening: a qualitative study. Eur J Hum Genet 2010; 18: 303–308.
Dillman D : Mail and Internet Surveys: The Tailored Design Method. Toronto: John Wiley and Sons, Inc., 2000.
Strauss A, Corbin J : Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory, 2nd edn, Thousand Oaks: Sage Publications, 1998.
Sandelowski M : Whatever happened to qualitative description? Res Nurs Health 2000; 23: 334–340.
Miller FA, Paynter M, Hayeems RZ et al: Understanding sickle cell carrier status identified through newborn screening: a qualitative study. Eur J Hum Genet 2010; 18: 303–308.
Juengst ET : ‘Prevention’ and the goals of genetic medicine. Hum Gene Ther 1995; 6: 1595–1605.
Borry P, Nys H, Dierickx K : Carrier testing in minors: conflicting views. Nat Rev Genet 2007; 8: 828.
Miller FA, Robert JS, Hayeems RZ : Questioning the consensus: managing carrier status results generated by newborn screening. Am J Public Health 2009; 99: 210.
Fraser FC : Genetic counseling. Am J Hum Genet 1974; 26: 636–659.
Grosse SD, Boyle CA, Kenneson A, Khoury MJ, Wilfond BS : From public health emergency to public health service: the implications of evolving criteria for newborn screening panels. Pediatrics 2006; 117: 923–929.
Ross LF : Mandatory versus voluntary consent for newborn screening? Kennedy Inst Ethics J 2011; 20: 299–328.
Acknowledgements
We are grateful to our research participants, and thank the Ontario Ministry of Health and Long-Term Care for project funding (06358). YB is supported by a Canadian Institutes of Health Research (CIHR) Postdoctoral Fellowship and fellowships from the CIHR Strategic Training Programs of ‘Public Health Policy’ and ‘Health Care, Technology and Place’. FAM is supported by a New Investigator Award from CIHR (80495). RZH is supported by a CADRE Postdoctoral Fellowship from CIHR and CHSRF. JC is supported by the Sydney G Frankfort Chair in Family Medicine. JL holds a Canada Research Chair in Human Genome Epidemiology. Sponsors’ support does not imply endorsement of the conclusions, for which the authors retain sole responsibility.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bombard, Y., Miller, F., Hayeems, R. et al. Health-care providers’ views on pursuing reproductive benefit through newborn screening: the case of sickle cell disorders. Eur J Hum Genet 20, 498–504 (2012). https://doi.org/10.1038/ejhg.2011.188
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejhg.2011.188
Keywords
This article is cited by
-
Expanding the Australian Newborn Blood Spot Screening Program using genomic sequencing: do we want it and are we ready?
European Journal of Human Genetics (2023)
-
Primary care provider perspectives on using genomic sequencing in the care of healthy children
European Journal of Human Genetics (2020)
-
Genetics Professionals’ Opinions of Whole‐Genome Sequencing in the Newborn Period
Journal of Genetic Counseling (2015)
-
Newborn screening for sickle cell disease: whose reproductive benefit?
European Journal of Human Genetics (2012)
-
Reply to Ross' commentary: Reproductive benefit through newborn screening: preferences, policy and ethics
European Journal of Human Genetics (2012)