Abstract
The objective was to determine the composition of the Cystic Fibrosis (CF) Population attending specialist UK CF centres in terms of age, gender, age at diagnosis, genotype and ethnicity. With the planned introduction of the national CF screening programme in the UK, cystic fibrosis transmembrane regulator (CFTR) mutations were compared between different ethnic groups enabling a UK-specific frequency of mutations to be defined. Data were analysed from the patient biographies held in the UK CF Database (see www.cystic-fibrosis.org.uk). The currently registered population of 5274 CF patients is 96.3% Caucasian with a male preponderance that significantly increases with age. The majority of the 196 non-Caucasian CF patients are from the Indian Subcontinent (ISC), of which one in 84 UK CF patients are of Pakistani origin. The commonest CFTR mutation, ΔF508, is found in 74.1% of all CF chromosomes. In the Caucasian CF population, 57.5% are ΔF508 homozygotes but the UK ISC CF population with only 24.7%, has significantly fewer ΔF508 homozygotes patients (95% confidence interval (CI) 0.2–0.4). The distribution of Caucasian patients with ΔF508/ΔF508, ΔF508/Other and Other/Other does not fit the expected distribution with a Hardy–Weinberg model unless those patients without a detected mutation are excluded (P<0.001). The UK CF Database has shown the UK CF population to have distinct characteristics separate from the North American and European CF Registries. The ISC group contains many mutations not recognised by current genetic analysis, and one in four ISC patients have no CFTR mutations identified. The CFTR analysis proposed for the screening programme would detect 96% of patients registered in the database, but is unlikely to achieve the desired >80% detection rates in the ethnic minority groups. Screen-positive, non-Caucasian infants without an identifiable CFTR mutation should be referred for a sweat test and genetic counselling when serum trypsinogen concentrations remain elevated after birth.
Similar content being viewed by others
Introduction
Cystic Fibrosis (CF) remains the commonest life-limiting autosomal recessive condition to affect the Caucasian UK population with a median age of death in the second decade for those born in the 1980s. There have been around 1000 individual CFTR mutations categorised since the landmark identification of the CFTR gene in 1989.1 The application of new anti-microbial therapies and nutritional knowledge have seen the outlook for CF patients born today improve such that survival into the fourth and fifth decades is possible with specialist care. It is presently unknown whether survival will improve further with the introduction of neonatal screening for cystic fibrosis in Scotland in 2002/3, because the impact of the CFTR mutation on the subsequent pattern and severity of symptoms experienced by the patient remains controversial. With respect to neonatal screening, Farrell's Wisconsin cohort has shown some patient benefits of screening through long-term surveillance2 but the controversy will only be settled by long-term analysis of trends using CF Registries. The UK CF Database contains such a registry within one of its modules and aims to analyse the clinical details of every cystic fibrosis patient in the United Kingdom who attends a specialist CF centre. This article presents the demographics of the currently registered UK CF population focusing on the gender, ethnicity, mode of presentation and genotypes of the 5274 patients from an estimated UK population of approximately 7500 patients.3 The considerable impact of ethnicity on CFTR mutations in the UK is shown.
Methods
The UK CF Database was established at the Tayside Institute of Child Health, University of Dundee, Scotland in 1995. The patient's age, gender, parental ethnicity, genotype, and method of diagnosis were included in the Patient Biographies and entered into the database from 56 paediatric and adult CF clinics, and validated through the system of double data entry, range checking and error correction. Full details of all procedures are available at www.cystic-fibrosis.org.uk. We divided the UK CF population into two groups (Figure 1): the Caucasian Group and the non-Caucasian Group. Within the non-Caucasian Group, we created a subgroup called the ISC Group consisting of all Pakistani, Indian, Bangladeshi and Asian Other patients.
Data was analysed using Microsoft Access 97 software and included all patients registered by May 2001. Statistical analysis is shown with 95% confidence intervals for the difference between two population proportions.
Results
There were a total of 5274 patients entered into the UK CF database. The gender split in the UK CF population is 2881 male (54.6%) and 2393 female (45.4%) with a male/female ratio that increases with age (Figure 2a,b). It can be seen that 49.1% of the entire population is under 15 years of age, 40.0% lies between 15 and 30 years, and only 11.0% of the population are still alive over the age of 30 years. There were 5078 patients in the Caucasian Group (96.3%) and 196 in the non-Caucasian Group. This second group contains a subset of 88 patients forming the ISC group (63 Pakistani, 12 Indian, seven Bangladeshi and six Asian Other patients), the remainder comprising six Black Caribbean, three Black African and 99 others of mixed parentage. Therefore, one in every 27 UK CF patients has some non-Caucasian origin, with those of purely Pakistani origin accounting for one in 84 UK CF patients.
The main presenting features that lead a clinician to consider a diagnosis of cystic fibrosis are failure to thrive, lower respiratory tract infections, steatorrhoea, meconium ileus, distal intestinal obstruction syndrome, family history, rectal prolapse, the presence of nasal polyps, electrolyte imbalance, prolonged jaundice or infertility (Table 1Table 1). The Caucasian and ISC subgroups both demonstrated similar patterns of presentation. Neonatal screening accounted for 11.7% of all diagnoses.
The median age of diagnosis was 4 months (range 0 months to 61 years 8 months). A diagnosis of CF occurred in 86.7% of all patients before their fourth birthday, and 63.1% were diagnosed before their first birthday. Diagnosis of cystic fibrosis beyond the age of 10 years was seen in 5.7% of all patients. To assess whether ethnic origin had any effect on age at presentation, Caucasian and ISC patterns of presentation were compared (Table 2Table 2). For Caucasian CF patients (n=5078), 63.0% were diagnosed before their first birthday, 84.7% before their fourth birthday, and 5.6% beyond their 10th birthday. In the ISC subgroup (n=88), 71.6% of patients were diagnosed before their first birthday, 87.5% before their fourth birthday and 8.0% were diagnosed over the age of 10. There was no significant difference in the proportions of those diagnosed before 1 year of age in the Caucasian and ISC populations (95% Confidence Limits –0.02 and +0.19). UK CF patients of Black African or Black Caribbean origins (n=9) had a diagnosis rate of 77.8% before the age of four, and 22.2% over the age of 10, but the numbers were too small to undertake statistical analysis.
Genotype data was available on 4933 patients that permitted further comparison of Caucasian and ISC patients to test the hypothesis that the genotypes were similar (Table 3Table 3). Patients with two chromosomes containing the ΔF508 mutation account for 57.5% of the genotyped UK CF Caucasian population (n=4753) but only 24.7% of the genotyped UK ISC CF patients (n=78) (95% CI 0.2–0.4 in the difference between the proportions). In contrast, there are no F508 homozygotes in the Black African or Black Caribbean groups. Further differences are revealed in the ISC group with 4.7% showing ΔF508 heterozygous status where the other CFTR mutation is either a known disease-associated allele or as yet uncharacterised. Importantly, patients with two known CFTR mutations, neither of which are ΔF508 make up 35.3% in the ISC population, many of these being family specific mutations. Thus at 27.1% of the ISC patients, a much larger proportion has no identifiable CFTR mutation compared to the Caucasian patient population.
The Caucasian population contains 4753 patients who have had their genotype tested (319 patients have not been tested, and six refused). The proportions of Caucasian patients with ΔF508/ΔF508, ΔF508/Other and Other/Other (where Other is either a known or an unknown non-ΔF508 mutation) were compared with expected values to see if the distribution fitted a Hardy–Weinberg model. From our data the maximum likelihood estimate of P is 0.751 (the proportion of ΔF508 in the population). Using our estimate of P to fit a Hardy–Weinberg model, we find that the observed number of ΔF508/ΔF508 and Other/Other is greater than expected. Wahlund's effect (http://darwin . eeb . uconn . edu / eeb348 / lecture - notes / wahlund /wahlund.html) may partly explain the excess of ΔF508/ΔF508, but this influence would also affect the other groups. However, when we exclude those patients without easily detectable CFTR mutations (n=124), the data satisfies Hardy–Weinberg equilibrium using a χ2 goodness-of-fit test (Observed : Expected ΔF508/ΔF508 2734 : 2755, ΔF508/Other 1674 : 1632 and Other/Other 221 : 242).
A total of 4933 patients have had their genotype tested, and Table 4Table 4 shows the gene frequency of different CFTR mutations amongst these 9866 chromosomes. We conducted a virtual study noting that the proposed Scottish screening programme includes a panel of 31 CFTR mutations (David Aitken, Guthrie Institute, Glasgow personal communication). These 31 mutations were compared with a ‘virtual DNA kit’ constructed from the 27 mutations shown in Table 4, composed of the 20 commonest mutations in the Caucasian Group and seven of the commonest mutations in the non-Caucasian Group. Amongst the different ethnic groups, Table 5Table 5 shows a comparison between the detection rates of at least one CFTR mutation using the 27-kit, the 31-kit and a virtual amalgam of 38 mutations (the 31-kit plus the additional seven non-Caucasian mutations used in the 27 kit). Overall, all the kits will detect 96% of all patients with at least one CFTR mutation, and 97% of pure Caucasians. Only those of purely Indian origin approach the >80% ideal threshold for a screening programme (detection rate 75%). Irrespective of the kit used, a detection rate of >87% will always occur in the mixed group and the screening programme will prove increasingly successful as the offspring of mixed relationships increase. Our data also shows that the 38-mutation kit performs no better than our proposed 27 kit for ethnic minorities. Irrespective of the final decision on the UK panel of mutations to be included, the index of clinical suspicion should remain high in the ISC, Black African or Black Caribbean patients who have no Caucasian parentage. Achieving a >80% detection rate for the UK patients in these ethnic groups is unlikely to be economically feasible due to the many individual/family specific mutations that would need to be included.
The regional distribution of CF patients, divided into three categories (ΔF508/ΔF508, ΔF508/Other and Other/Other) is shown in Table 6Table 6. The much greater proportion of Other/Other CF patients in Northern Ireland (and the corresponding drop in ΔF508/ΔF508) was statistically significant compared to every other region in the UK (P<0.05).
Discussion
The UK CF database has registered 5274 patients and characterises the majority of the CF specialist clinic population for the start of the new millennium. We have shown that the non-Caucasian CF population makes up 3.6% of the UK CF population and their range of CFTR mutations are markedly different to the Caucasian patients although they were diagnosed at similar ages and with similar symptoms.
Screening in the UK
Some of the best evidence for supporting a neonatal screening programme is based on Farrell's evidence for nutritional benefits.2 The Cochrane review4 found a second randomised controlled trial from the UK5 that did not show a benefit to early diagnosis but is of interest that in the latter study, patients screened for CF were not all referred to a specialist centre for their care. Thus the criterion that appropriate treatment facilities should be in place post-screening was not met in this study.
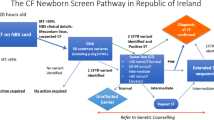
Screening in Scotland is scheduled to commence in 2002/3. It is envisaged that the proposed screening programme will be based on a three-stage protocol.6 In the first stage, a confirmed raised immunoreactive trypsinogen (IRT) level on a day 4–6 blood spot sample would be followed by a second stage DNA analysis for CFTR mutations from the same blood spot card. Individuals with two CFTR mutations will be referred with a definite diagnosis of CF. Infants with only one CFTR mutation, or those with a very high IRT and of non-Caucasian origin who have no identified CFTR mutation, would undergo a third stage repeat blood spot for IRT on day 27 of life. If the latter IRT is also raised, the infant has a high probability of CF and will be referred for sweat testing and genetic counselling. If not, the infant has a low probability of CF and the family will be offered genetic counselling alone. With current knowledge, CFTR mutation analysis cannot provide the full answer for all, but selective application of an IRT–IRT strategy is the only way of providing reasonable sensitivity, especially when screening non-Caucasian babies.
CFTR mutations in Caucasians
Large-scale CF studies have revealed common genotypes more prevalent in certain populations. Schwarz et al studied the distribution and frequency of Caucasian UK CFTR mutations in 19957 and listed 20 of the commonest mutations. Nineteen of these mutations feature in the commonest UK Caucasian 20 mutations listed in Table 4. Our data confirms the proportion of ΔF508 in the Caucasian population at 75.2%, comparable to the Schwarz value of 75.3%. There are similar frequencies for the more common mutations between our UK Caucasian CF data (Table 4) and the Schwarz data (respectively, G551D 3.43% and 3.08%; G542X 1.84% and 1.68%; 621+1G→A 1.27% and 0.93%; 1717-1G→A 0.58% and 0.57%). In North America, ΔF508 accounts for 71.2%, with G542X (2.4%), G551D (2.4%), W1282X (1.4%), N1303K (1.3%) and R553X (0.9%).8
Genotype frequencies in CF have previously been shown to fit a Hardy–Weinberg model in a smaller regional UK study.9 In the current study, we find that the genotype frequencies only satisfy the Hardy-Weinberg equilibrium provided we exclude those without an identified CFTR mutation in the Other/Other category. This suggests that defects in non-CFTR genes may contribute to the CF phenotype. Our pragmatic exclusion of all patients with untyped mutations in CFTR from the Other/Other group will of necessity exclude some patients with very rare mutations that are not picked up by routine genetic tests (20 kit, 31 kit etc). This might explain why the new observed values now fall below the expected values in the Other/Other category.
When compared with a European CFTR geographic distribution,10 the UK CF patients possess a greater proportion of ΔF508, G551D and 621+1G→T mutations, and a smaller proportion of G542X, N1303K, W1282X and R1162X mutations. In France, the five most common genotypes were ΔF508/ΔF508 (47.8%), ΔF508 /G542X (3.4%), ΔF508/N1303K (2.7%), ΔF508 /1717-1G→A (2.1%) and ΔF508/2789+5G→A (1.5%) (Desgeorges M, personal communication) which is different to the commonest genotypes found in the UK population (Table 3). N1303K and G542X occur at a frequency of around 5% in Italy.11 In Germany, a study of 658 CF families revealed mutation frequencies of R553X (1.8%), N1303K (1.3%), G542X (1.1%), G551D (0.8%) and R347P (0.8%).12 The frequency of CFTR mutations recorded for just over 1000 patients for the Irish CF Database include G551D in 7%, R117H in 2% and ΔF508 in 72% of patients.13 In the white South African population, a paper based on 192 patients found that ΔF508 accounts for 76% of the mutations with 3272-26A→G (4%), 394delTT (3.6%) and G542X (1.3%) the other most common mutations.14 It is suggested that the 3272-26A→G and 394delTT mutations are more common due to a founder effect in white South Africans of European descent. Northern Ireland has a much greater proportion of Other/Other CF patients (where neither mutation is ΔF508) and although there is a higher incidence of CF in Northern Ireland (one in 1850), the population frequency of ΔF508 is similar to other regions of the UK.7
CFTR mutations in the Non-Caucasian population
Cystic Fibrosis is being increasingly diagnosed in the non-Caucasian populations, and the range of presenting features is similar between Caucasian and ISC groups (Table 1). The genotypes of non-Caucasian patients often contain individual or family specific mutations along with mutations more commonly found in Caucasians due to admixture of the populations. A recent paper by Malone et al,15 detected five novel CFTR mutations in 26 Pakistani patients and three of these mutations are reported in our 63 Pakistani patients. Malone's subgroup analysis of 14 Pakistani patients showed 32% of chromosomes had the ΔF508 mutation, similar to the 29% in our Pakistani patient data. In a small study of UK Asian CF patients,16 Bowler et al reported that these patients appeared to have a poorer respiratory and nutritional status compared to age matched controls, and noted that only 44% (four out of nine) patients had the ΔF508 mutation. In Spencer's study of ethnic minority children in the West Midlands17, 31% (4/13) of patients from the ISC had the ΔF508 mutation, but no other mutations were found. This study also found no overall delay in diagnosis between the white European CF patients and the CF patients from ethnic minorities. Our data confirms this finding that there is no delay in diagnosis between the Caucasian and non-Caucasian groups. ΔF508 carrier status has been estimated at one in 238 women from North India (Kapoor V, personal communication), giving an estimated frequency of the homozygote at one in 228 000. In a later study of 13 Indian CF children, Kapoor found the ΔF508 mutation in 53.8% of chromosomes.18 Our study represents the largest reported group of UK CF patients from the ISC and finds that one in four has no CFTR mutation identified. The relative infrequency of the most common CFTR mutations in the ISC patients has implications for the national CF screening programme. Screening for the commonest mutations will detect smaller proportions of non-Caucasian CF individuals than their Caucasian counterparts. Our 27-mutation virtual kit of mutations is particularly suited to detect mutations in the non-Caucasian as well as the Caucasian population, compared to the proposed 31-mutation kit or a combined kit of 38 mutations.
Differences in presentation between UK and North America
In common with CF populations studied in North America, Canada, Europe and Australasia, there is a male preponderance,19,20,21 and half of the patients remain in the paediatric age group. The over 30s represent only one in 10 patients. Comparison of the mode of presentation between the UK CF Database (Table 1) and the North American CF Patient Registry8 reveals (respectively) differences in the rates of lower respiratory tract infection (34.6% and 51.7%), failure to thrive/malnutrition (35.8% and 43.4%), steatorrhoea (29.0% and 35.3%), meconium ileus (13.2% and 20.8%) and screening (11.7% and 3.5%). It is noteworthy that the UK rate for presentation with meconium ileus (13.2%) is very similar to the Canadian data (13.4%).21 In the UK, there were 63% patients diagnosed by 1 year of age (Table 2) compared to 70% in North America8 and 56.4% from the Canadian Patient Data Registry.22 In the UK CF Database, neonatal screening accounts for around one in 10 CF patients and the overall median age of diagnosis is 4 months, whilst in populations without screening, the mean age of CF diagnosis is reported at 5.7 months23 and 11.7 months.5
Summary
The UK CF Database provides a framework for analysing the changing demographics of the CF population in the UK. The population is 96.4% Caucasian with a slight male preponderance. The commonest CFTR mutation, ΔF508, is found in 74.1% of CF patients’ chromosomes, and ΔF508 homozygotes make up 57.5% of the Caucasian CF population. Detection of 96% of patients registered in the database is possible with the CFTR analysis proposed for the screening programme, but is unlikely to achieve the desired >80% detection rates in the ethnic minority groups. The National Screening programme for CF must take account of the different range of CFTR mutations in the non-Caucasian CF population, so that screening also benefits patients from ethnic minorities.
References
Riordan JR, Rommens JM, Kerem B et al. Identification of the cystic fibrosis gene: cloning and characterization of complementary DNA Science 1989 245: 1066–1073
Farrell PM, Kosorok MR, Rock MJ et al. Early diagnosis of cystic fibrosis through neonatal screening prevents severe malnutrition and improves long-term growth Pediatrics 2001 107: 1–13
Dodge JA, Morison S, Lewis PA et al. Incidence, population, and survival of cystic fibrosis in the UK, 1968–95 Arch Dis Child 1997 77: 493–496
Merelle ME, Lees CM, Nagelkerke NF et al. Newborn Screening for Cystic Fibrosis (Cochrane Review). In the Cochrane Library 2000 4: Oxford: Update Software
Chatfield S, Owen G, Ryley HC et al. Neonatal Screening for cystic fibrosis in Wales and the West Midlands: clinical assessment after five years of screening Arch Dis Child 1991 66: 29–33
Pollitt RJ, Dalton A, Evans S et al. Neonatal screening for cystic fibrosis in the Trent region (UK): two-stage immunoreactive trypsin screening compared with a three-stage protocol with DNA analysis as an intermediate step J Med Screen 1997 4: 23–28
Schwarz MJ, Malone GM, Haworth A et al. Cystic Fibrosis Mutation Analysis: Report from 22 UK Regional Genetics Laboratories Hum Mut 1995 6: 326–333
Cystic Fibrosis Patient Registry 2000 – Annual Data Report September 2001.
Green MR, Weaver LT, Heeley AF et al. Cystic fibrosis identified by neonatal screening: incidence, genotype, and early natural history Arch Dis Child 1993 68: 464–467
Estivill X, Bancells C, Ramos C et al. Geographic distribution and regional origin of 272 cystic fibrosis mutations in European populations Hum Mut 1997 10: 135–154
Rendine S, Calafell F, Capello N et al. Genetic Distribution of cystic fibrosis mutations in Italy. 1 Regional distribution Ann Hum Genet 1997 61: 411–424
Tummler B, Storrs T, Dziadek V et al. Geographic distribution and origin of CFTR mutations in Germany Hum Genet 1996 97: 727–731
Cashman SM, Patino A, Delgado MG et al. The Irish Cystic Fibrosis Database J Med Genet 1995 32: 972–975
Goldman A, Labrum R, Claustres M et al. The molecular basis of cystic fibrosis in South Africa Clin Genet 2001 59: 37–41
Malone G, Haworth A, Schwarz MJ, Cuppens H, Super M . Detection of five novel mutations of the cystic fibrosis transmembrane regulator (CFTR) gene in Pakistani patients with cystic fibrosis: Y569D, Q98X, 296+12(T>C), 1161delC and 621+2(T>C) Hum Mut 1998 11: 152–157
Bowler IM, Estlin EJ, Littlewood JM . Cystic Fibrosis in Asians Arch Dis Child 1993 68: 120–122
Spencer DA, Venkataraman M, Higgins S, Stevenson K, Weller PH . Cystic fibrosis in children from ethnic minorities in the West Midlands Respir Med 1994 88: 671–675
Kabra M, Ghosh M, Kabra SK, Khanna A, Verma IC . Delta F508 molecular mutation in Indian Children with cystic fibrosis Indian J Med Res 1996 104: 355–810
Rosenfeld M, Davis R, Fitzsimmons S, Pepe M, Ramsey B . Gender gap in cystic fibrosis mortality Am J Epidemiol 1997 145: 794–803
Fogarty A, Hubbard R, Britton J . International Comparison of Median Age at Death from Cystic Fibrosis Chest 2000 117: 1656–1660
Kerem E, Corey M, Kerem B et al. Clinical and genetic comparisons of patients with cystic fibrosis, with or without meconium ileus J Pediatr 1989 114: 767–773
Corey M, Farewell V . Determinants of mortality from cystic fibrosis in Canada, 1970–1989 Am J Epidemiol 1996 143: 1007–1017
Waters DL, Wilcken B, Irwig L et al. Clinical outcomes of newborn screening for cystic fibrosis Arch Dis Child Fetal Neonatal Ed 1999 80: F1–F7
Acknowledgements
The authors are grateful for the financial support of the CF Trust and the National Services Division of NHS (Scotland). We thank M Fraser and K Nicol for their expert data validation, and in the large CF Clinics, all the data entry staff and the Directors for their support. There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McCormick, J., Green, M., Mehta, G. et al. Demographics of the UK cystic fibrosis population: implications for neonatal screening. Eur J Hum Genet 10, 583–590 (2002). https://doi.org/10.1038/sj.ejhg.5200850
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejhg.5200850
Keywords
This article is cited by
-
Understanding protein kinase CK2 mis-regulation upon F508del CFTR expression
Naunyn-Schmiedeberg's Archives of Pharmacology (2011)
-
A methodology to establish a database to study gene environment interactions for childhood asthma
BMC Medical Research Methodology (2010)
-
Light and alcohol evoked electro-oculograms in cystic fibrosis
Documenta Ophthalmologica (2006)
-
Bacterial activity in cystic fibrosis lung infections
Respiratory Research (2005)