Abstract
Background/Objectives:
To determine whether a ‘junk food’ diet at age 4½ is associated with behavioural problems at age 7.
Subjects/Methods:
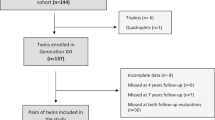
Data on approximately 4000 children participating in the Avon Longitudinal Study of Parents and Children, a birth cohort recruited in Avon, UK in 1991/92 were used. Behavioural problems were measured at age 7 using the Strengths and Difficulties Questionnaire (SDQ; maternal completion). Total difficulties and scores for the five sub-scales (hyperactivity, conduct and peer problems, emotional symptoms and pro-social behaviour) were calculated. Principal components analysis of dietary data (frequency of consumption of 57 foods/drinks) collected at age 4½ by maternal report was used to generate a ‘junk food’ factor. Data on confounders were available from questionnaires.
Results:
A one standard deviation increase in ‘junk food’ intake at age 4½ years was associated with increased hyperactivity at age 7 (odds ratio: 1.19; 95% confidence interval: 1.10, 1.29). This persisted after adjustment for confounders including intelligence quotient score (odds ratio: 1.13; 95% confidence interval: 1.01, 1.15). There was little evidence to support an association between ‘junk food’ intake and overall behavioural difficulties or other sub-scales of the SDQ.
Conclusions:
Children eating a diet high in ‘junk food’ in early childhood were more likely to be in the top 33% on the SDQ hyperactivity sub-scale at age 7. This may reflect a long-term nutritional imbalance, or differences in parenting style. This finding requires replication before it can provide an avenue for intervention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Ahmad A, Murthy M, Greiner RS, Moriguchi T, Salem NJ (2002). A decrease in cell size accompanies a loss of docosahexanenoate in the rat hippocampus. Nutr Neurosci 5, 103–113.
Bateman B, Warner JO, Hutchinson E, Dean T, Rowlandson P, Gant C et al. (2004). The effects of a double blind, placebo controlled, artificial food colourings and benzoate preservative challenge on hyperactivity in a general population sample of preschool children. Arch Dis Child 89, 506–511.
Bellisle F (2004). Effects of diet on behaviour and cognition in children. Br J Nutr 92, S227–S232.
Cox JL, Holden JM, Sagovsky R (2004). Edinburgh Postnatal Depression Scale (EPDS). Department of Psychiatry, University of Edinburgh: Edinburgh.
Crown S, Crisp AH (1979). Manual of the Crown-Crisp Experiential Index. Hodder & Stoughton: London.
Gesch CB, Hammond SM, Hampson SE, Eves A, Crowder MJ (2002). Influence of supplementary vitamins, minerals and essential fatty acids on the antisocial behaviour of young adult prisoners. Randomised, placebo-controlled trial. Br J Psychiatry 181, 22–28.
Golding J, Pembrey M, Jones R, ALSPAC Study Team (2001). ALSPAC—the Avon Longitudinal Study of Parents and Children. I. Study methodology. Paediatr Perinat Epidemiol 15, 74–87.
Goodman R (1997). The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry 38, 581–586.
Goodman R (2001). Psychometric properties of the Strengths and Difficulties Questionnaire. J Am Acad Child Adolesc Psychiatry 40, 1337–1345.
Hirayama S, Hamazaki T, Terasawa K (2004). Effect of docosahexaenoic acid-containing food administration on symptoms of attention-deficit/hyperactivity disorder—a placebo-controlled double-blind study. (see comment). Eur J Clin Nutr 58, 467–473.
Langseth L (1996). Nutritional Epidemiology: Possibilities and Limitations. ILSI Europe: Belgium.
Lauritzen L, Hansen HS, Jorgensen MH, Michaelsen KF (2001). The essentiality of long chain n−3 fatty acids in relation to development and function of the brain and retina. Prog Lipid Res 40, 1–94.
Lawlor DA, Davey Smith G, Bruckdorfer R, Kundu D, Ebrahim S (2004). Those confounded vitamins: what can we learn from the differences between observational versus randomised trial evidence? Lancet 363, 1724–1727.
MAFF (1994). The Dietary and Nutritional Survey of British Adults: Further Analysis. HMSO: London.
Maughan B, Kim-Cohen J (2005). Continuities between childhood and adult life. Br J Psychiatry 187, 301–303.
Northstone K, Emmett P, ALSPAC Study Team (2005). Multivariate analysis of diet in children at four and seven years of age and associations with socio-demographic characteristics. Eur J Clin Nutr 59, 751–760.
Parker G, Gibson NA, Brotchie H, Heruc G, Rees AM, Hadzi-Pavlovic D (2006). Omega-3 fatty acids and mood disorders. Am J Psychiatry 163, 969–978.
Reisbick S, Neuringer M, Hasnain R, Connor WE (1994). Home cage behavior of rhesus monkeys with long-term deficiency of omega-3 fatty acids. Physiol Behav 55, 231–239.
Rogers I, Emmett P, ALSPAC Study Team (1998). Diet during pregnancy in a population of pregnant women in South East England. EurJ Clin Nutr 52, 246–250.
Schab DW, Trinh NT (2004). Do artificial food colors promote hyperactivity in children with hyperactive syndromes? A meta-analysis of double-blind placebo-controlled trials. Dev Behav Pediatr 25, 423–434.
Schnoll R, Burshteyn D, Cea-Aravena J (2003). Nutrition in the treatment of attention-deficit hyperactivity disorder: a neglected but important aspect. Appl Psychophysiol Biofeedback 28, 63–75.
StataCorp (2003). Stata Statistical Software: Release 8. Stata Corporation: College Station, TX.
Stevens L, Zhang W, Peck L, Kuczek T, Grevstad N, Mahon A et al. (2003). EFA supplementation in children with inattention, hyperactivity, and other disruptive behaviors. Lipids 38, 1007–1021.
UK Department for Environment, FARA (2005). Family Food. A Report on the 2003–04 Expenditure and Food Survey. TSO: London.
van Buuren S, Boshuizen HC, Knook DL (1999). Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med 18, 681–694.
Voigt RG, Llorente AM, Jensen CL, Fraley JK, Berretta MC, Heird WC (2001). A randomized, double-blind, placebo-controlled trial of docosahexaenoic acid supplementation in children with attention-deficit/hyperactivity disorder. J Pediatr 139, 189–196.
Wechsler D, Golombok S, Rust J (1992). WISC-III: Wechsler Intelligence Scale for Children—Third Edition UK Manual. The Psychological Corporation: Sidcup, UK.
Wiles NJ, Peters TJ, Heron J, Gunnell D, Emond A, Lewis G (2006). Fetal growth and childhood behavioural problems: results from the ALSPAC cohort. Am J Epidemiol 163, 829–837.
Wolraich ML, Wilson DB, White JW (1995). The effect of sugar on behavior or cognition in children. JAMA 274, 1617–1621.
Acknowledgements
We thank all the families who took part in this study, the midwives for help in recruiting them and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses. The UK Medical Research Council, the Wellcome Trust and the University of Bristol provided core support for ALSPAC. The funding bodies have had no influence over this work or its publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guarantors: K Northstone and NJ Wiles.
Contributors: The study idea was conceived by GL and PE, with input from NJW and KN. KN analysed the data, with input from NJW, PE and GL. NJW wrote the first draft of the paper, which was revised after comments from all other authors. The ALSPAC study team designed the original study and collected and entered the data. This publication is the work of the authors.
Rights and permissions
About this article
Cite this article
Wiles, N., Northstone, K., Emmett, P. et al. ‘Junk food’ diet and childhood behavioural problems: results from the ALSPAC cohort. Eur J Clin Nutr 63, 491–498 (2009). https://doi.org/10.1038/sj.ejcn.1602967
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1602967
Keywords
This article is cited by
-
Dietary patterns in middle childhood and behavior problems in adolescence
European Journal of Clinical Nutrition (2021)
-
Fructose Intake Impairs Cortical Antioxidant Defenses Allied to Hyperlocomotion in Middle-Aged C57BL/6 Female Mice
Neurochemical Research (2020)
-
Possible links between gut–microbiota and attention-deficit/hyperactivity disorders in children and adolescents
European Journal of Nutrition (2020)
-
Dietary patterns are associated with attention-deficit/hyperactivity disorder (ADHD) symptoms among preschoolers in mainland China
European Journal of Clinical Nutrition (2018)
-
Exposure to gestational diabetes mellitus induces neuroinflammation, derangement of hippocampal neurons, and cognitive changes in rat offspring
Journal of Neuroinflammation (2017)