Abstract
Krabbe disease (globoid cell leukodystrophy) is an autosomal recessive disorder of white matter resulting from deficiency of galactosylceramide beta-galactosidase (GALC) and the consequent accumulation of galactosylceramide and psychosine. Although most patients present within the first 6 months of life, i.e., the early infantile or “classic” phenotype, others present later in life including in adolescence and adulthood. The only available treatment for infants with early infantile Krabbe disease is hematopoietic cell transplantation (HCT), typically using umbilical cord blood. Although transplanted children are far better neurologically than they would have been had they followed the typical fulminant course of early infantile Krabbe disease, anecdotal reports have surfaced suggesting that the majority of presymptomatic children transplanted for Krabbe disease have developed motor and language deterioration. The cause and extent of the deterioration is unknown at this time. With the advent of universal newborn screening for Krabbe disease in New York State and the projected start of screening in Illinois in 2010, understanding the outcome of treatment becomes of paramount importance. Thus, the purpose of this workshop was to bring together child neurologists, geneticists, neurodevelopmental pediatricians, transplanters, neuroradiologists, neurophysiologists, developmental neurobiologists, neuroscientists, and newborn screeners to review the results of the transplantation experience in humans and animals and, if neurologic deterioration was confirmed, develop possible explanations as to causation. This workshop was the first attempt at a multicenter crossdiscipline evaluation of the results of HCT for Krabbe disease. A broad range of individuals participated, including clinicians, academicians, and authorities from the National Institutes of Health, American College of Medical Genetics, and Department of Health and Human Services.
Similar content being viewed by others
SESSION 1: CLINICAL OUTCOMES OF INFANTS AND YOUNG CHILDREN TRANSPLANTED FOR KRABBE DISEASE
The first issue to be addressed was the current status of presymptomatic infants transplanted for Krabbe disease (Abstract, Supplemental Digital Content 1, http://links.lww.com/A843; Abstract, Supplemental Digital Content 2, http://links.lww.com/A844; Abstract, Supplemental Digital Content 3, http://links.lww.com/A845; Abstract, Supplemental Digital Content 4, http://links.lww.com/A846). The largest cohort is from the Duke University Pediatric Blood and Marrow Transplant Program in collaboration with the University of North Carolina (UNC). In addition to this experience, the registry of the Pediatric Bone Marrow Transplantation Consortium (PBMTC) was used to identify Centers in the United States and Canada that had transplanted children with Krabbe disease. The PBMTC investigators were sent a questionnaire regarding age at transplant, transplantation regimen, complications of transplant, results of baseline neurodiagnostic studies, current neurological and developmental status, whether the child had spasticity, optic atrophy, seizures, presence or absence of deep tendon reflexes, whether assistive devices were necessary for ambulation and communication, current height, weight, and head circumference, and whether or not the child had developed progressive neurologic/developmental deterioration.
The Duke/UNC data were presented by Doctors Kurtzberg and Escolar (Abstract, Supplemental Digital Content 1, http://links.lww.com/A843 and Abstract, Supplemental Digital Content 2, http://links.lww.com/A844). Duke/UNC have evaluated 16 presymptomatic children transplanted at Duke and elsewhere for early infantile Krabbe disease. Of these, two have died in transplant. Of the remainder, all are spastic, although three are reported to be mild. Five require gastrostomies (although are able to eat by mouth), all are below the 3% for height and weight and most are below the 3% for head circumference. Receptive language is normal; however, all have abnormal expressive language because of impaired articulation. All have abnormal gross motor control, with 50% walking with assistive devices and only 25% able to walk independently. The investigators reported that all are considered to be normal cognitively. (There was a discussion at the meeting as to the difficulty in assessing intelligence accurately in children with such severe motor and language deficits.)
A composite group of nine children from other PBMTC transplant centers in the United States and Canada was also presented. (None of these children was transplanted at Duke.) (Abstract, Supplemental Digital Content 3, http://links.lww.com/A845.) Six infants with a positive family history of early infantile Krabbe disease and low GALC activity were transplanted before symptom onset. One died of complications of transplant. Of the remaining five, all have delayed development and abnormal neurologic examinations. Three of the four children beyond 3 years of age are unable to walk without assistance because of slowly progressive spasticity. Three of four have acquired microcephaly, four of four have weights below the 3%, and three of four have heights <5%. Progressive neurological deterioration is present in three of four. (The child with stable, albeit delayed development, is only 3 years old.) An additional presymptomatic child transplanted because of a family history of probable later onset disease has a normal neurologic exam but acquired microcephaly and growth failure. Because there is wide variability in the later onset variants even within families, it is difficult to know what the child's outcome would have been in the absence of transplant. In addition to the presymptomatic children, two symptomatic children were transplanted for later onset disease. Both have abnormal neurologic examinations, cognitive impairment, and seizures.
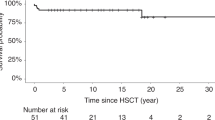
To put these results in perspective, untreated children with early infantile Krabbe disease have an average survival of 23 months, although survival beyond 8 years has been reported. The course of the disease is stereotypic and is characterized by rapid neurologic deterioration, evolving over days to weeks, in which the child becomes extremely irritable, develops spastic quadriplegia with opisthotonus, loses the ability to eat orally, loses milestones, becomes blind and deaf, develops seizures and apnea, and typically dies of respiratory complications.1
In contrast, children with early infantile Krabbe disease who receive transplant presymptomatically have a more indolent course and seem to have improved survivals. In the cohorts of children treated at Duke and elsewhere, the mortality from transplantation is 15%. Of the remaining children, none have died of progressive Krabbe disease although the longest follow-up is only 13 years. Although it is uncertain at this time whether transplantation significantly lengthens survival, it clearly attenuates the severity of the symptoms. Most patients, however, will develop slowly progressive neurologic deterioration over several years. It seems that the younger children have developmental delays, but as they get older they develop increasing spasticity, loss of motor milestones, language deficits, progressive microcephaly, and heights and weights below the 3%.
The almost universal finding (in both the Duke and composite cohorts) of heights and weights below the 5% is of particular interest. One child in the composite group had formal endocrine testing and was found to be growth hormone deficient, a finding that has previously been reported in some patients transplanted with a preparative regimen that included busulfan. Several of the Duke cohort received endocrine evaluations. None were hypothyroid. Formal growth hormone testing has not been performed, but a few had random growth hormone levels that were normal. Several children who had not been on steroids were found to be cortisol deficient.
In addition to the clinical outcomes of the infants transplanted for Krabbe disease, sequential neuroimaging and neurophysiologic studies have been performed at Duke and at the other sites. Magnetic resonance imaging (MRI) scans were performed on three presymptomatic children transplanted in the composite group. MRI results did not correlate with neurologic examinations as normal scans were found in the presence of both progressive spasticity and acquired microcephaly, whereas a child with only developmental delay had atrophy, ventriculomegaly, and white matter changes.
Sequential neurophysiologic studies of children transplanted for Krabbe disease at Duke revealed improvement after transplant, particularly the nerve conduction studies and brainstem auditory evoked potentials (Abstract, Supplemental Digital Content 4, http://links.lww.com/A846). Whether these improvements in neurophysiological parameters reflect similar improvements in clinical course await further studies, but based on the clinical outcomes, it is likely that these studies will not correlate well with neurologic status either.
SESSION 2: ANIMAL MODELS OF KRABBE DISEASE: LONG-TERM OUTCOMES AFTER DIFFERENT TREATMENT STRATEGIES
There are three naturally occurring animal models for Krabbe disease, the mouse (twitcher), the dog (Cairn and West Highland terrier), and the monkey (macaque) (Abstract, Supplemental Digital Content 5, http://links.lww.com/A847; Abstract, Supplemental Digital Content 6, http://links.lww.com/A848; Supplemental Digital Content 7, http://links.lww.com/A849; Supplemental Digital Content 8, http://links.lww.com/A850; Supplemental Digital Content 9, http://links.lww.com/A851). Treatment trials have been employed most extensively in the mouse and dog models. The monkey model shows great promise, but the number of affected animals until recently has been limited. The results of the various treatment regimens have been uniformly disappointing. Trials have included antiinflammatory agents (indomethacin), substrate reduction (l-cycloserine), retroviral gene therapy, and recombinant GALC enzyme therapy, injection of stem cells into the brain, bone marrow transplantation, and combined therapy. The best survivals have been associated with bone marrow transplantation, often combined with other therapies. Most of the investigators reported initial improvement in neuropathology, a reduction in psychosine levels, as well as improved nerve conduction studies and neuroimaging. Despite this, all treated animals died of progressive disease.
The report by Kondo and Duncan (Abstract, Supplemental Digital Content 5, http://links.lww.com/A847) demonstrated that although long-lived twitcher mice, transplanted using a regimen of myeloablation with busulfan, initially had neuropathologic signs of improvement, ultimately there was evidence of extensive myelin destruction (>200 days). Thus, although transplantation is associated with prolonged survival and early signs of a reduction in demyelination, all animals died of active disease. The authors also described the unusual presence of bilateral defects in the ventrolateral thalamic nuclei, a finding not previously reported. Of interest, a 1-year-old wild-type mouse also developed similar thalamic lesions after myeloablation with busulfan. Because this abnormality has not been reported in untreated twitcher or wild-type mice, it is likely that the thalamic defects were not due to progressive Krabbe disease but resulted from the induction chemotherapy.
Gama-Sosa (Abstract, Supplemental Digital Content 6, http://links.lww.com/A848) presented studies that pointed to a role for endothelial cells affecting the properties of neural progenitor cells. If the two types of cells were grown in transwells that allowed exchange of media and secreted products but did not touch, the endothelial cells secreted something that prevented differentiation of the neural progenitor cells. However, if the cells were grown together (in contact), the endothelial cells induced differentiation of the neural progenitor cells and caused alignment of neuronal processes. He presented some evidence that collagen IV may be the factor that induces this effect.
Bunnell presented the monkey model. (Abstract, Supplemental Digital Content 7, http://links.lww.com/A849.) Clinically and neuropathologically, the animals bear a marked resemblance to the disease in humans. Perhaps the most interesting observation is that despite the fact that there is a single genetic mutation (unlike humans in which there are >100 identified to date), there is wide phenotypic variability. Indeed age at onset of symptoms can vary from 19 to 140 days and survivals from 52 to 642 days. This wide range of phenotypic variability is not present in twitcher mice. Because a major concern in the area of human newborn screening is the inability to predict phenotype (i.e., based on enzyme level, genetic mutation or neurodiagnostic studies), the availability of a later onset Krabbe disease animal model becomes extremely important and may allow us to develop new insights into the disease process.
Mark Haskins presented the experience with the canine model (Abstract, Supplemental Digital Content 8,http://links.lww.com/A850). Although this animal model, unlike the monkey, does not seem to have a later onset phenotype, there is a wide range of symptom onset, with some not showing symptoms for 210 days. Several different treatment trials were reported including the antiinflammatory approach (indomethacin), bone marrow transplantation, substrate reduction using l-Cycloserine alone, a combination of HCT and l-cycloserine, and retroviral gene therapy. The best results were seen when HCT (using lethal total body radiation) was combined with l-cycloserine. Despite significantly improved survivals, however, the animals ultimately succumbed to the disease. An interesting observation was that magnetization transfer ratios revealed changes in the internal capsule, corpus callosum, and corona radiata of control animals who had received lethal radiation, similar to that found in both untreated and transplanted affected animals. Thus, the treatment itself caused significant damage to white matter tracts.
Wenger (Abstract, Supplemental Digital Content 9, http://links.lww.com/A851) presented an extensive body of work on the treatment of twitcher and another mouse model with bone marrow transplantation (using radiation or busulfan), gene therapy using viral vectors, nonsteroidal antiinflammatory agents, recombinant GALC enzyme, and injections of stem cells into the brain. Despite prolongation of life and even improvement in the neuropathology of the brains of these animals, they all ultimately succumbed to disease.
SESSION 3: POSSIBLE ETIOLOGIES FOR THE LONG-TERM NEUROLOGICAL DEFICITS IN TRANSPLANTED CHILDREN
At the conclusions of Sessions 1 and 2, it had become clear to the participants that long-term outcomes of both humans and animals transplanted for Krabbe disease were not optimal and that progressive neurologic deterioration is found in many of the treated subjects (Abstract, Supplemental Digital Content 10, http://links.lww.com/A852; Abstract, Supplemental Digital Content 11, http://links.lww.com/A853; Abstract, Supplemental Digital Content 12, http://links.lww.com/A854; Abstract, Supplemental Digital Content 13, http://links.lww.com/A855; Abstract, Supplemental Digital Content 14, http://links.lww.com/A856). Possible etiologies included inflammation, preexisting damage to white matter, and oligodendroglia that preceded engraftment, damage to oligodendroglia, and myelin from chemotherapy, and the possibility of active, albeit attenuated disease, because of insufficient enzyme entering the central nervous system after transplant.
Inflammation clearly plays a role in the pathology of Krabbe disease, even if the inflammation is not as extreme as in adrenoleukodystrophy (Abstract, Supplemental Digital Content 10, http://links.lww.com/A852). Treating the inflammation, however, may be a double-edged sword in the context of transplant, as it may stabilize the blood-brain barrier, thereby limiting the access of donor-derived microglia into the central nervous system. On the other hand, reducing inflammation may slow the disease process. One of the questions about the use of HCT in a rapidly progressive disorder such as early infantile Krabbe disease has been how can it be effective if it takes at least 3 months to engraft while the disease can progress to profound spastic quadriplegia in a matter of weeks? Perhaps, the high-dose chemotherapy and steroids suppress the inflammatory component of the disease, providing a window of disease suppression during which the transplant can engraft and secrete enzyme.
The presence of preexisting damage to white matter and oligodendroglia identified on the neuropathology of infants with Krabbe disease also raised serious questions (Abstract, Supplemental Digital Content 11, http://links.lww.com/A853). If there is evidence of abnormalities in the spinal cord and brainstem as early as the first trimester, transplant at birth is unlikely ever to be fully successful. Although this preexisting damage does not explain the progressive neurologic deterioration, it does explain the developmental delays that are seen in most of these children. Clearly, to be effective, future treatment strategies will have to include both enzyme replacement therapy in one form or another as well as myelin repair.
Although the results of combined therapies in twitcher (in this case using viral transduction in combination with HCT) (Abstract, Supplemental Digital Content 12, http://links.lww.com/A854) demonstrated improved survivals (105 days for twitcher treated on this regimen compared with survivals of 40 days for untreated twitcher and 730 days for unaffected mice), improved motor performance by 20% and reduced proinflammatory markers, it is clear that while the disease is attenuated, it is not cured. (It should be noted, that the survivals of Sands' mice were shorter than those of Wenger and Kondo, presumably because he transplanted them at a younger age and they were unable to tolerate complete marrow ablation.) At 40 days, the treated mice had no globoid cells, increased myelination, and minimal macrophage activation. Despite this, the animals went on to develop significant neurologic deficits and early death. Thus much like the transplanted children, the disease is not cured but reduced in intensity for a time.
The discussion of the effects of HCT on the brain of patients with severe MPS 1 (Abstract, Supplemental Digital Content 13, http://links.lww.com/A855) demonstrated that although HCT may protect hippocampal function, it also causes damage to fiber systems, as seen on fractional anisotropy. Thus, presumably the chemotherapy itself is destructive to white matter. This was also found in the experience with 5 FU, in which the agent caused a syndrome of delayed degeneration of white matter tracts. Because the primary clinical deterioration found in transplanted children is motoric, further study of the adverse effects of the induction chemotherapy used in HCT is warranted to determine whether it contributes to the neurologic deterioration that occurs in these patients.
The discussion of stem cell biology, including cell lineage and suitability for replacement therapy, the need for specific cell types in transplantation therapies, the cellular redox state and signal transduction, and finally the concept of complex systems, emphasized that outcome is not readily predicted from the initial conditions and that improvement cannot be expected to be simply a reversal of the disease process (Abstract, Supplemental Digital Content 14, http://links.lww.com/A856). It must instead reflect a substantially new set of cell and biological mechanisms. To date, treatment trials have focused on replacing the missing enzyme either by viral transduction, HCT, or gene therapy This talk pointed out that to be successful it will be necessary to use a multifaceted approach which will have to include eventual repair of damaged myelin. It was also a sobering refection on how little we understand the ultimate effects of these approaches and the possibility of unintended consequences.
CONCLUSIONS
The participants reached consensus that presymptomatic children with early infantile Krabbe disease who are transplanted in the first 3 weeks of life survive longer than would be expected without intervention. The vast majority of these infants, however, develop microcephaly, motor and other neurological deficits on follow-up, most of which are progressive in nature. In addition to these neurologic deficits, somatic growth impairment is nearly universal in children and animals transplanted for Krabbe disease. The reason for the failure to thrive is just one more area that demands research attention.
Another area of interest is the poor correlation between neuroimaging, neurophysiologic studies, and clinical course. Improvements identified in the white matter on standard MRI and diffusion tensor imaging posttransplant have been reported in patients despite evidence of progressive neurologic dysfunction. Similarly, although most nerve conduction studies improve posttransplant, clinical deterioration is the norm. Clearly, more sensitive techniques are needed to monitor response.
Research on Krabbe disease has been greatly enhanced because of the availability of animal models. The work on the mouse and dog models, in particular, have conclusively demonstrated that although bone marrow transplantation improves survival and even transiently decreases psychosine and improves myelination, the disease is not cured. All transplanted animals to date have ultimately died of Krabbe disease. At death, evidence of severe myelin destruction is universal.
The overarching question is why the various treatment regimens used in animals and humans with Krabbe disease have been only somewhat effective and are never curative. The answer reflects the complexity of the disease. The pathology of Krabbe disease involves many components, including storage of psychosine and galactosylceramide, cell death, inflammation, macrophage response, and myelin arrest and degeneration. In addition, because the formation of myelin is a temporal event, any potential treatment needs to be timely as well as global to improve both the central and peripheral nervous systems. Many of the treatments tried so far address a limited portion of the overall problem. It surely will take a combined approach to effectively treat this disease.
It is clear that the clinical manifestations of Krabbe disease after transplantation in humans and animal models are progressive, almost certainly because of active disease. Based on the available data, HCT should be viewed as a treatment that attenuates the clinical course and improves survival but is not curative. In addition, inflammation, the neurotoxic effects of drugs used in the preparative regimen for transplantation, and other so far unrecognized factors may be contributing to the neurologic deterioration.
What are the next steps?
-
1
Further progress in understanding the long-term outcomes of patients transplanted for Krabbe disease and other lysosomal storage disorders will require the collection and analysis of comprehensive data from multiple centers participating in a prospective study. To achieve this goal, it will be necessary to establish uniform guidelines (across centers) for the indications of offering this intervention. Similarly, informed consents should be consistent in their presentation of the potential risks and benefits of the procedure. Finally, a standardized research protocol should be established for both baseline and longitudinal follow-up of transplanted patients, which will include central review of neuroimaging, neurophysiology, neuropsychologic testing, and neurologic examinations. To achieve these goals, funding will be necessary. In the meantime, the Hunter James Kelly Research Institute is planning to initiate the process by holding a multidisciplinary workshop to address these issues, beginning with the development of a standardized consensus driven clinical evaluation protocol for baseline and long-term follow-up of patients transplanted for Krabbe disease and other lysosomal disorders.
-
2
A workshop, sponsored by HRSA (Maternal and Child Health Bureau) and Hunter's Hope Foundation will be held in August 2009 to address the topic, “HCT in Metabolic Disease: Rationale, Efficacy and Long Term Complications.” It is essential that more research be done to define the basic mechanism of action of HCT in metabolic disorders. What is the capacity of the microglia to secrete GALC? Where in the nervous system and in what amounts does the enzyme go? What is the role of inflammation? Why does psychosine decrease and myelination increase in the animal models posttransplant while the animal continues to deteriorate?
In addition, the workshop will compare the outcomes of children transplanted for Krabbe disease with those with other metabolic disorders. Is there something unique about patients with Krabbe disease or do patients with other metabolic diseases face similar problems?
Finally, the meeting will address the long-term outcomes of infants transplanted for metabolic and oncologic diseases. In particular, the potential adverse effects of high-dose neurotoxic chemotherapy on cognitive abilities, endocrine function, neurologic status, and oncogenesis will be discussed.
Final thoughts
Although the workshop did not specifically address the rationale for performing newborn screening for Krabbe disease in light of the less than optimal results with transplant, the topic does deserve mention (P.K.D.). It seems to me that newborn screening for an inherited disease such as Krabbe disease serves several purposes. First, it allows early diagnosis of a condition that is often misdiagnosed for many months (reflux, cerebral palsy, etc.). Earlier diagnosis, even in the absence of transplant, would improve the quality of life of the infants by allowing the prompt delivery of appropriate palliative interventions and, for the families, a realistic understanding of their child's prognosis. Moreover, newborn screening allows the family to make rational decisions as to family planning. Too often, the diagnosis of Krabbe disease is not made until the second or even third child is born.
Finally, the issue of transplant needs to be addressed. Even with the long-term neurologic deficits, the quality of life of many of these children is superior to that of those with the untreated early infantile phenotype. One reviewer stated, “One day these children will raise the terrible question to their physician, why did you transplant me to be in the state I am today?” This is an issue that child neurologists face with many devastating conditions including spina bifida, brain tumors, and the very aggressive treatment of neuromuscular disease when tracheostomies and ventilators become part of the child's future. In pediatrics, the child's parents must make the decision as to the degree of medical intervention their child will receive. At the same time, the doctors must provide as accurate a prognosis as possible, not only in terms of survival but also in terms of long-term quality of life. Some families, armed with this knowledge, will refuse transplant, whereas others will welcome it. For those latter families, there is the enduring hope that the extension of life provided by HCT may allow their child to be treated with additional, more effective therapies as they become available in the future.
Reference
Duffner PK, Jalal K, Carter RL . The Hunter's Hope Krabbe family database. Pediatr Neurol 2009; 40: 13–18.
Acknowledgements
Funding for this conference was made possible (in part) by a Grant (NS063609-01) from the National Institute of Neurological Disorders and Stroke (NINDS), the Office of Rare Diseases, NICHD, a Grant from Maternal and Child Health Bureau (1H1TMC10605-01-00), and Hunter's Hope Foundation. The following investigators received funding from the following sources for part or all of the work they presented: Patricia K. Duffner, MD, Maternal and Child Health Bureau (1H1TMC10605-01-00 and Hunter's Hope Foundation; Bruce Bunnell, PhD, NIH-NCRR, R24 RR022826-01; Marc Patterson MD Actelion pharmaceuticals: a phase I/II randomized controlled study of OGT 918 in adult and juvenile patients with Niemann Pick C disease). PI, Mark Haskins, PhD, NIH, Yoichi Kondo MD, PhD and Ian Duncan, PhD, NIH and the Myelin Project; Florian Eichler, MD, NINDS, David Wenger, PhD, NIH; Miguel Gama-Sosa, PhD, Alzheimer's Association; Mark Sands, PhD, NIH and Hunter's Hope Foundation; Elsa Shapiro, PhD, is funded by the Ryan Foundation and Genzyme; Mark Noble, PhD, is funded by NIH and the Koman Foundation for the Cure.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.geneticsinmedicine.org).
The views expressed in written conference materials or publications and by speakers and moderators do not necessarily reflect the official policies of the Department of Health and Human Services; nor does mention by trade names, commercial practices, or organizations imply endorsement by the US Government.
Disclosure: Lawrence Charnas, MD, PhD, had no conflicts of interest regarding the data presented at the meeting. Lawrence Charnas, MD, PhD, is currently at Shire HGT Cambridge, MA. Shire HGT was not involved in the study described herein. Dr. Elsa Shapiro is a member of the MPS I Registry Board of Advisors for Genzyme. None of the other authors, cochairs, speakers, or contributors have conflict of interest.
APPENDIX: MEETING PARTICIPANTS
APPENDIX: MEETING PARTICIPANTS
Meeting Organizer: Patricia K. Duffner, MD, University at Buffalo School of Medicine and the Hunter James Kelly Research Institute.
Session 1: Cochairs: Marc C. Patterson, MD, Mayo Clinic and Kirk R. Schultz, MD, BC Children's Hospital.
Speakers: Joanne Kurtzberg, MD, Duke University Medical Center, Maria L. Escolar, MD, University of North Carolina at Chapel Hill, Aatif M. Husain, MD, Duke University School of Medicine, Lawrence Charnas, MD, PhD, University of Minnesota, Rajinder Bajwa, MD, Nationwide Children's Hospital, Morris Kletzel, MD, Northwestern University, Daniel W. Pietryga, MD, Nationwide Children's Medical Center, Brandon Triplett, MD, St Louis University, Martin A. Champagne, MD, Hôpital de Verdun, Kirk R. Schultz, MD, BC Children's Hospital
Session 2: Cochairs: Richard W. Erbe, MD, University at Buffalo, David A. Wenger, PhD, Jefferson Medical College.
Speakers: Yoichi Kondo, MD, PhD, University of Wisconsin, Ian D. Duncan, PhD, University of Wisconsin, Miguel Gama-Sosa, PhD, Mt Sinai School of Medicine, BruceA Bunnell, PhD, Tulane National Primate Research Center, Mark Haskins,VMD, PhD, Washington University, David Wenger, PhD, Jefferson Medical College.
Session 3: Cochairs: Verne S. Caviness, Jr, MD, DPhil, Massachusetts General Hospital, Chester Whitley, MD, PhD, University of Minnesota.
Speakers: Florian Eichler, MD, Massachusetts General Hospital, James M. Powers, MD, University of Rochester, Mark S. Sands, PhD, Washington University, Mark Noble, PhD, University of Rochester, Elsa G. Shapiro, PhD, University of Minnesota.
Rights and permissions
About this article
Cite this article
Duffner, P., Caviness, V., Erbe, R. et al. The long-term outcomes of presymptomatic infants transplanted for Krabbe disease: Report of the workshop held on July 11 and 12, 2008, Holiday Valley, New York. Genet Med 11, 450–454 (2009). https://doi.org/10.1097/GIM.0b013e3181a16e04
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e3181a16e04
Keywords
This article is cited by
-
Consensus guidelines for newborn screening, diagnosis and treatment of infantile Krabbe disease
Orphanet Journal of Rare Diseases (2018)
-
Long-term Improvements in Lifespan and Pathology in CNS and PNS After BMT Plus One Intravenous Injection of AAVrh10-GALC in Twitcher Mice
Molecular Therapy (2015)
-
Design of a regulated lentiviral vector for hematopoietic stem cell gene therapy of globoid cell leukodystrophy
Molecular Therapy - Methods & Clinical Development (2015)
-
Fetal Brain-directed AAV Gene Therapy Results in Rapid, Robust, and Persistent Transduction of Mouse Choroid Plexus Epithelia
Molecular Therapy - Nucleic Acids (2013)
-
Newborn screening for lysosomal diseases: current status and potential interface with population medical genetics in Latin America
Journal of Inherited Metabolic Disease (2012)