Abstract
Study design:
Retrospective register-based epidemiological study.
Objective:
To estimate the prevalence rate of persons with spinal cord injury (SCI) with special reference to ASIA Impairment Grade A–D.
Setting:
Helsinki, Finland.
Methods:
Cases were identified using the registers of the Käpylä Rehabilitation Centre, Helsinki University Central Hospital and the local organization for the disabled. Local health centres were informed about the study, residential service houses were contacted, and announcements were published in patient magazines.
Results:
A regional population was found to have a prevalence rate of 28/100 000 inhabitants with SCI (ASIA Impairment Scale A–D).
Conclusion:
The prevalence rate in this study is consistent with the data published in other Nordic countries.
Sponsorship:
The Finnish Cultural Foundation.
Similar content being viewed by others
Introduction
It is important to know the epidemiology of spinal cord injury (SCI) in order to develop health care and social services. Particularly, the increasing number of those who sustained their injury decades ago need more attention. A specific follow-up system for SCI should be designed to prevent severe complications and loss of functional capacity.
Estimates of the incidence of SCI vary greatly from country to country. The reasons for this are the different local socioeconomic factors influencing, for example, the intensity of traffic or the level of violence. Likewise, dissimilar definitions of SCI and the means by which data are collected influence the end results. Data recently published in Europe on the incidence of SCI in survivors of the acute phase range from 10 to 25/million inhabitants per year.1,2
The prevalence rates also show significant variations due to differences in methodology and in estimates of the incidence and life expectancy. Blumer and Quine,3 in their review, reported prevalence rates ranging from 11 to 112/100 000 inhabitants. Most published reports on the prevalence of SCI are based on survival data or surveys instead of on case registers.3 In the Nordic countries, two register-based studies have been published, showing consistent rates between 22 and 25/100 000 inhabitants.4,5
In the Helsinki area, the acute care of all unstable fractures or other traumas of the spinal column with neurological deficits are centralized in Helsinki University Central Hospital. Primary rehabilitation nearly always takes place in Käpylä Rehabilitation Centre, Finnish Association of People with Mobility Disabilities, and also located in Helsinki.
The Käpylä Rehabilitation Centre was established in 1953, mainly to care for the victims of polio epidemics, but also to rehabilitate persons with spinal cord injuries. Since the 1960s the Käpylä Rehabilitation Centre has been the only national rehabilitation centre in Finland caring for patients with SCI immediately after acute hospital phase. This has also been the official recommendation of the Ministry of Social Affairs and Healthy of Finland.
Between the years 1978 and 1997, this centre received approximately 55 new cases of ASIA Impairment Scale A–D6 per year from all over the country, which would mean an incidence of SCI of 10 per million inhabitants per year in Finland.7 Because the injured (especially children, ASIA-E cases and some elderly patients) are not all referred to our centre, we estimate that the true incidence of those surviving the acute phase is at least 13–15 per million inhabitants per year.
In 1998, The Health Committee of Helsinki started a programme to analyse the utilization of the health care resources, the present health status and the social situation of persons with SCI. The first step in this programme was to find out the number of persons who have SCI and are citizens of Helsinki.
The aim of this study was to identify all adult citizens (18 years or more) of Helsinki who had permanent sensory or motor deficits because of traumatic SCI (ASIA A–D). ASIA-E cases were excluded. The study design was retrospective. An epidemiological study of this kind has not been made previously in Finland.
Materials and methods
Helsinki and its neighbouring towns form a geographically small urban area of about 1 million inhabitants on the south coast of Finland and in this respect the Helsinki area differs from the rest of the country, which is relatively sparsely populated. The inclusion criteria was based on a cross-section date, 1.1.1999, (subjects had to be alive on 1.1.1999). At that time, there were 546 000 inhabitants in Helsinki and 5.16 million inhabitants in Finland.
In order to carry out the study as a whole, permission was requested from the Ethics Committee, Helsinki University Central Hospital, as well as from the Ministry of Social Affairs and Healthy of Finland.
Subjects were identified with the aid of several sources:
-
Between the years 1953–1998, Käpylä Rehabilitation Centre has had altogether 1931 patients with SCI as either in- or out-patients. A computerized list of names and social security numbers of these persons was sent to the Helsinki Register Office, from which we obtained information about those who were still living and their addresses.
-
From the register of patients of the Department of Orthopaedic Surgery, Helsinki University Central Hospital subjects were searched for by diagnosis codes since 1989, when the register was computerized. ICD-9 (International Statistical Classification of Diseases and Related Health Problems) was used in Finland until 1995 and all cases with the codes 806, 952 and 9072A were checked. In 1996, ICD-10 was introduced in Finland and cases with codes S14.0, S14.1, S14.2, S24.0, S24.1, S24.2, S34.0, S34.1, S34.2, S34.3 and T91.3 were taken into account in our study. On checking the registers of patients in Helsinki University Central Hospital, we noticed that ICD codes did not necessarily match the actual situation documented in the medical records. While ICD-9 was used, some patients were found coded with SCI, who turned out to have only fractures of the spine without any neurological deficits. They were excluded by checking the medical records thoroughly. On the other hand, we found that after 1996, when ICD-10 was introduced, the new way of coding apparently leads to the neglect of some cases with SCI.
-
The membership register of the local organization of the disabled was checked manually from 1940 in order to find persons meeting the inclusion criteria.
-
The local health centres were informed about the study in order to find subjects.
-
Residential service houses with potential citizens of Helsinki were contacted.
-
In order to find other cases not included in any of the above-mentioned sources, announcements were published in patient magazines.
A total of 152 cases of SCI were found. For data collection, the subjects were first contacted by sending them a detailed, structured questionnaire. A total of 131/152 subjects (86%) participated in the study and returned a filled-in questionnaire.
The drop-out group consisted of 21 subjects. We tried to contact them as follows:
-
One died before the sending of the questionnaire;
-
10 were contacted, of whom eight refused and two promised to take part, but never returned the questionnaire;
-
10 did not answer their mail and could not be contacted by phone.
All those 10 who could not be contacted by any means were, according to the Helsinki Register Office, alive and living in Helsinki. This was confirmed twice.
Those who were willing to participate in the study were invited to a clinical visit lasting from 2.5 to 4 h. During the visit, a medical history was obtained, and the medical status, including the ASIA classification and possible interventions, was noted. The subjects met doctor and physiotherapist and also a nurse, when needed.
A total of 125/152 subjects (82%) made a clinical visit. Of the six subjects who participated only by questionnaire, two had recently visited our out-patient clinic and the data were obtained in this way, three refused an invitation to a clinical visit and one had moved outside the Helsinki area.
Results
Altogether 152 patients who met the inclusion criteria were found. The distribution of the sources through which the patients were found is shown in Table 1.
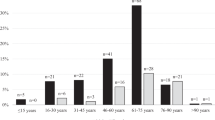
A total of 36 (24%) of the patients were women and 116 (76%) were men (Table 2).
The mean age of the patients during the follow-up was 47.9 (SD 13.0) years (women 49.2 (SD 12.4) years, men 47.5 (SD 13.1) years).
The mean time since the injury was 16.9 years (SD 11.4; min. 3 months and max. 50 years) (women 18.6 (SD 13.6) years, men 16.4 (SD 16.9) years).
The prevalence of SCI in Helsinki was 28/100 000 inhabitants (95% CI: 24–32). The prevalence of women with SCI was 12/100 000 (95% CI: 9–17) and of men 46 (95% CI: 38–55).
The distribution of the prevalence rate by age groups is shown in Table 2. The highest prevalence rate was in the age group 45–59 years.
The causes of injury were most often falls (43%), followed by traffic accidents (35%). The rate of violence was only 4%. The distribution of causes of injury is shown in Table 3.
Additionally, 10% (n=15/152) of the injuries were related to suicide attempts.
Up-to-date data of the ASIA Impairment Scale were available for 121 subjects and the distribution is shown in Figure 1.
A total of 46% of the study group (n=56/121) had tetraplegia and 54% (n=65/121) paraplegia. In 57% (n=69/121), the lesion was incomplete and 43% (n=52/121) complete.
Discussion
A reasonable effort was made to find as many SCI cases as possible. For subject identification, several methods were used, some of them quite time-consuming. Because identification was done first from the registers of the Käpylä Rehabilitation Centre, out of a total of 152 cases only five were found from Helsinki University Central Hospital and 12 by other means. This reflects the good functioning of the Käpylä Centre. However, we can assume that some cases were missed by not checking the registers of minor hospitals.
Comparison with most of the other studies of prevalence presented has difficulties because of methodological differences. Only a few register-based reports covering the population in a defined area have been published.3 Some studies also take into account subjects with nontraumatic aetiologies, which should be noticed when comparing the results.
Most of the studies from the US show higher prevalences.3 In Europe, rates similar to those in our study have been published.4,5 In our work, we used a clear cross-section date (1.1.1999), which makes the end result more precise.
In the Stockholm Spinal Cord Injury Study (SSCIS)3 using similar methods the prevalence rate was 22.3/100 000 inhabitants, but also included children and persons with ASIA Impairment Grade E. In this respect, our result (28/100 000) is higher, which could be explained by the higher incidence in Finland. However, in the SSCIS the mean time since injury was about 10 years, as compared to 17 years in this study. This might indicate a longer life expectancy in Finland, although the SSCIS was done some years earlier.
The leading cause of injury was falls, followed by transportation accidents. There is no specific explanation for the relatively high rate of falls, but a similar finding has been reported by van Asbeck et al.2
In our work, 10% of injuries could be related to attempts at suicide, which were more frequent than in other studies.8,9 This is characteristic of Helsinki, in which the average male age-standardized rate of suicide attempts is the highest reported in Europe.10
These data also confirm the findings of the SSCIS that the prevalence of paraplegia is higher than tetraplegia and that of incomplete than that of complete lesions.8 On the other hand, the distribution of patients among the incomplete group is valuable, because such information has not been reported earlier in prevalence studies. In tetraplegia, over half of the incomplete cases, 18/33 (55%) have ASIA Impairment Scale D. Information of this kind is important when planning services for persons with SCI, because inside the group ‘incomplete’ there is a huge variation of functional capacity.
In conclusion, epidemiology relying only on ICD-9 codes will lead to significant overestimation. In our work, apparently more than half of these codes were misleading. This has also been found in other studies.2 On the other hand, according to the 3 years (1996–98) checked in this study, the new method of coding SCI in ICD-10 seems to neglect some cases of permanent neurological deficits.
From the results of this study, it is now easier to estimate more accurately the need for health care and rehabilitation services for SCI in Finland.
References
Martins F et al. Spinal cord injuries – epidemiology in Portugal's central region. Spinal Cord 1998; 36: 574–578.
van Asbeck FWA, Post MWM, Pangalila RF . An epidemiological description of spinal cord injuries in The Netherlands in 1994. Spinal Cord 2000; 38: 420–424.
Blumer CE, Quine S . Prevalence of spinal cord injury: an international comparison. Neuroepidemiology 1995; 14: 258–268.
Levi R The Stockholm spinal cord injury study: medical, economical and psycho-social outcomes in a prevalence population. Doctoral Dissertation 1996. Karolinska Institutet, Stockholm.
Knutsdottir S . Spinal cord injuries in Iceland. A follow up study. Paraplegia 1993; 31: 68–72.
Maynard FM et al. International standards for neurological and functional classification of spinal cord injury. Spinal Cord 1997; 35: 266–274.
Alaranta H, Valtonen K, Dahlberg A . Epidemiology of traumatic spinal cord injuries in Finland from 1978 to 1997. Abstract. 11th European Congress of Physical Medicine and Rehabilitation. Göteborg 1999.
Levi R, Hultling C, Nash MS, Seiger Å . The Stockholm spinal cord injury study: 1. Medical problems in a regional SCI population. Paraplegia 1995; 33: 308–315.
Biering-Sörensen F, Pedersen W, Giörz Muller P . Spinal cord injury due to suicide attempts. Paraplegia 1992; 30: 139–144.
Schmidtke A et al. Attempted suicide in Europe: rates, trends and sociodemographic characteristics of suicide attempters during the period 1989–1992. Results of the WHO/EURO Multi centre Study on Parasuicide. Acta Psychiatr Scand 1996; 93: 327–338.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Dahlberg, A., Kotila, M., Leppänen, P. et al. Prevalence of spinal cord injury in Helsinki. Spinal Cord 43, 47–50 (2005). https://doi.org/10.1038/sj.sc.3101616
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101616
Keywords
This article is cited by
-
Rehabilitation outcome in people with spinal cord injuries resulting from diving in South Korea
Spinal Cord Series and Cases (2022)
-
Pulse article: survey of neurogenic bladder management in spinal cord injury patients around the world
Spinal Cord Series and Cases (2021)
-
Inequalities in pharmacologic treatment of spasticity in Sweden – health economic consequences of closing the treatment gap
Health Economics Review (2020)
-
Entstehungsursachen, Lebenserwartung und Todesursachen bei Menschen mit traumatischer Querschnittlähmung – Eine monozentrische Analyse von 190 Fällen
Trauma und Berufskrankheit (2018)
-
Incidence of acute spinal cord injury in the Czech Republic: a prospective epidemiological study 2006–2015
Spinal Cord (2017)