Abstract
Study design: Case report of recovering radiation myelopathy.
Objective: To present autopsy and functional imaging findings on a unique case of slowly recovering radiation myelopathy with the aim of the clarification of the underlying mechanism.
Patient: The cervical spinal cord and the distal part of the medulla oblongata of a 36-year-old thyroid cancer patient had been incorrectly irradiated with a total dose of 61 Gy and a fraction size of 3.4 Gy (J Neurol Sci 1999; 163:39–43), resulting in incomplete cervical transection with a 5-month latency period following the termination of radiotherapy. This was followed by a 9.5-year spontaneous improvement until her demise, during which the check-ups were supplemented by positron emission tomography (PET) investigations; these indicated increased [18F]deoxyglucose and [15O]butanol uptakes, but a diminished [11C]methionine accumulation by the irradiated spinal cord segment.
Results: Autopsy revealed demyelination (with axonal loss) and neuronal damage in the cervical spinal cord and the distal part of the medulla oblongata. In the same region, only minimal vascular injury (thickening of some of the capillary walls) was detected, but not cell proliferation or chronic inflammation. Bilateral, secondary pyramidal tract degeneration caudal to the irradiated segment was observed. The PET and autopsy findings, although separated by 2 years, are consistent.
Conclusions: The pathological state of the spinal cord revealed by the autopsy is concordant with the incomplete cervical transection, implying that the functional recovery is supported by a process that probably differs from the restoration of the mechanism destroyed by the radiotherapy. For the restoration of the function, we suggest an altered conduction mechanism of the action potential, involving an increased number of sodium channels along the demyelinated segments of the injured axons, which is fully congruent with the PET findings.
Similar content being viewed by others
Introduction
It is well known that the spinal cord is a critical organ as it displays an enhanced radiosensitivity relative to those of neighbouring normal organs or neoplastic tissues.1,2 This circumstance explains why any calculation error in radiotherapy planning or misalignment during the irradiation sessions may result in radiation myelopathy. This rare complication of radiotherapy can affect the white and grey matter structures separately or in combination.3,4,5,6,7,8,9,10,11 The clinical picture of predominantly white matter injury (demyelination and vascular injury) consists of spastic motor sequelae, and sensory and vegetative deficits. Radiation myelopathy may also manifest itself less frequently as grey matter damage, that is, the destruction of neurones. The most marked damage generally involves the large motor neurones of the anterior horns, resulting in consecutive flaccid paresis.4,5,6,7,11,12,13
Radiation myelopathy usually runs a chronic, progressive, irreversible and relentless clinical course, with only rare recovery from established motor sequelae. A thorough literature search unearthed only seven well-documented published cases of remission.12,14,15,16 Here, we report on the autopsy findings on one of these patients,12 who had undergone positron emission tomography (PET) studies during the 10-year clinical course. The results of the present autopsy findings, together with those of previous PET imaging, offer a more complete description of this case with its partially reversible radiation myelopathy and the underlying pathologic processes.
Case report and autopsy findings
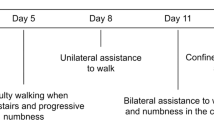
A 36-year-old papillary thyroid cancer patient erroneously received an overdose (18 × 3.4 Gy/fraction, total dose: 61 Gy) to her cervical spinal cord and the distal part of the medulla oblongata during postoperative telecobalt radiotherapy in 1990.12 With a 5-month latency period after the termination of radiotherapy, incomplete cervical transection developed: spastic paraplegia of her lower extremities, spastic paresis of her left arm, flaccid paresis affecting her left hand, and sensory deficits below the cervico-thoracic junction on the left side, and below the 10th thoracic dermatome on the right side. The patient experienced bladder dysfunction and constipation. The symptoms culminated 9 months following radiotherapy, and then gradually improved over the 9 years from the 11th month after the last fraction. She eventually became ambulatory (the lower-limb paraplegia partially ceased and progressed to spastic paraparesis), some of her sensory deficits also disappeared, and her constipation-related symptoms lessened, but the degree of atrophy in the small muscles of the left hand remained.
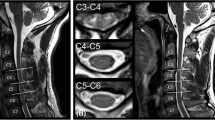
Magnetic resonance imaging (MRI) (1.5 T Magnetom, Siemens, Erlangen, Germany) of the spinal cord was first performed 4 years after the completion of radiotherapy and revealed atrophy of the entire spinal cord (Figure 1). Repeated PET measurements (GE 4096 Plus scanner, General Electric, Uppsala, Sweden) during the 6–8 years of the clinical course documented an increased [18F]deoxyglucose (FDG) uptake and augmented [15O]butanol perfusion, while the [11C]methionine uptake in the irradiated spinal cord segment was negligible (Figure 2).
PET examinations (attenuation-corrected median sagittal section of the head and neck region) reveal increased (arrows) FDG and [15O]butanol, but low [11C]methionine accumulation within the irradiated cervical spinal cord segments. The BUT and MET panels are shifted relative to the FDG panel in order to ensure the same vertical location of the identical anatomical structures in all three images
In 2000, the otherwise apparently healthy patient had been complaining for months of short episodes of dyspnoea, but investigations by experts in relevant specialities (oto-rhinolaryngology, neurology and radiation oncology) had not revealed any definite explanatory reason. Later during the same year, she suddenly lost consciousness as a consequence of a central respiratory arrest that could not be explained by any clinical evidence. During the subsequent 2 weeks, assisted ventilation was performed, but without any improvement, and her condition was complicated by acute meningitis, which led to her death.
Besides acute purulent meningitis throughout the central nervous system (CNS), the autopsy did not reveal signs of any other illnesses (including recurrent thyroid cancer). The primary radiogenic injury was limited to the irradiated segments of the cervical cord and medulla oblongata. Grossly, extreme atrophy and bizarre distortion of the spinal cord were observed, accompanied by marked fibrosis of the meninges and dura mater.
The histopathology verified the macroscopically diagnosed acute purulent meningitis, revealing extensive perivascular and meningeal granulocytic infiltration within the entire CNS. There was no indication of chronic inflammation, as no astrocytosis, gliosis or accumulation of mononuclears was detected.
The cervical portion of the spinal cord that had received the miscalculated high dose of radiation displayed a pronounced, bilateral loss of myelin and axons within the lateral (mainly) and posterior columns (Figure 3a–c). A few thinly remyelinated sheaths were present at the edges of the demyelinated plaques (Figure 3d). Moreover, bilateral, extensive damage to the neurones was also observed, most markedly among the motor neurones of levels C1 and C2 (Figure 4), and was practically identical on each side. The larger and smaller arterioles and venules of the irradiated spinal cord were intact (Figure 5a,b), but the walls of some capillaries exhibited thickening (Figure 5c). No telangiectasia was observed and the antibody to factor VIII gave only slight positivity (not shown). Below the irradiated cervical spinal cord segments, bilateral, secondary pyramidal tract degeneration was to be seen (Figure 6).
The medulla oblongata exhibited patchy demyelination and neuronal degeneration (especially in the dorso-medullary respiratory group); this was most probably caused by the erroneously delivered high radiation dose at the margin of the cervical radiation fields, which might have been responsible for the clinically unexplained central apnoea. Although the demise of the patient was not directly related to this radiation-induced side effect, the radiation injury through central apnoea was an initiating factor of the presumably iatrogenic purulent CNS infection.
Discussion
The response of the CNS to radiation involves several pathological components, generally regarded as permanent.3,4,5,6,7,8,9,10,11 One of them is demyelination (mainly related to the loss of oligodendrocytes and glial progenitor cells), which causes consecutive axonal loss, gliosis and astrocytosis (Type 1 lesion). Vascular (Type 2) lesions include endothelial cell damage in all vessels, preferentially in arterioles and venules,11 but also in capillaries, accompanied by a chronic inflammatory reaction involving mononuclears (lymphocytes, mainly T cells, macrophages and microglia) and often fibrinoid necrosis of the vascular wall (radiation vasculitis). Eventually, thickening of the vessel walls, telangiectasia and thrombosis/occlusion evolve. Vascular obstruction frequently causes infarction in the area supplied by the affected vessels (radiation necrosis). Type 3 lesions involve the simultaneous occurrence of the above-mentioned two types of injuries. Besides white matter reactions, grey matter sequelae (neuronal degeneration, chromatolysis, and a coarse tigroid appearance of the Nissl substance) may also occur in the anterior and posterior horns of the spinal cord,4,5,6,7,11,13 but the grey matter per se is less radiosensitive than the white matter.4,5,6,11
Tables 1 and 2 present data on 17 cases of Type 1 lesions and 10 cases of Type 2 injuries, collected from the English literature.4,5,6,9,12,17,18,19,20,21,22,23,24,25,26 The Type 2 lesions were further subclassified on the basis of the delivered dose, as cases with doses in the conventional therapeutic range (six cases) and those with an accidental, extremely high overdosage (four cases).
The most striking difference between the two main types (ie Type 1 and Type 2, conventional radiotherapeutic dosage subtype) of radiation injury is observed in the length of the latency period preceding the first observed symptoms. The mean latency period for demyelination is 11 months and that for vascular injury is 30 months. This corroborates the data reviewed by Schultheiss, that is, 14 and 29 months for the two groups, respectively.9 At the same time, the average durations of survival of the patients following radiotherapy were almost identical: 30 months for Type 1 lesions and 34 months for Type 2 (therapeutic dose range subtype), as calculated from the data in Table 1 and 2. The noteworthy difference in the average survival from the time of appearance of the symptoms might imply a less effective repair of the consequences of the vascular damage. The specified fraction size or the total dose or both was too high (>2 and >50 Gy, respectively) in all cases in both groups. Additional known risk factors (reirradiation, diabetes mellitus, hypertension, hyperbaric O2 inhalation, chemotherapy and old age) were documented in most cases in the ‘demyelination group’, and in all cases in the group dominated by vascular sequelae. Although the listed differences are distinct and the associated histopathologies differ appreciably, the exact pathogenetic factors and the determinants of the actual scenario for the development of a dominant white matter or a dominant vascular injury remain uncertain. The features of the history of our case are characteristic of the group of predominantly demyelination injuries, as she had no additional risk factors, and there was a short latency period (5 months) and a long survival (9.5 years) following the appearance of the symptoms.
A special group of radiation myelopathic patients with extremely high fraction size (20 Gy) and exceedingly high total dose (>120 Gy), because of a malfunctioning linear accelerator, comprises a distinct clinical entity.18,22 The latency period in these patients was very short (around 1 month) and the disease had a very fast progression. The vascular injuries developed exceptionally quickly, and all patients died within 3 months, before the development of significant demyelination.
No data have been published so far on the histopathology of reversible radiation myelopathy; thus, our case may be of interest. As expected from the clinical symptoms, we found extensive demyelination with axonal loss and marked lower motor neurone sequelae. It is worth pointing out that, although the radiation dose was delivered homogeneously, as reflected by the practically homogeneous histopathological reaction on both sides, an obvious asymmetry appeared in certain clinical signs and symptoms (eg spasticity and flaccid paresis only in the left arm, side differences in sensory symptoms, etc.). This may be related to the fact that radiation-induced damage detected as a significant decrease in the number of a given cell type does not necessarily result in the same obvious functional deficit. A decrease in the population of a single cell type is too simple a pathogenetic explanation to account for the development of a defined loss of function.
The almost complete lack of vascular injuries in our case deserves discussion. Although the vascular endothelium is one of the structures that is most sensitive to irradiation, there might be a significant individual variation in its response.27 Factors such as the age of the patient, the presence of hypertension, diabetes mellitus, other vascular diseases, the efficiency of the blood supply (eg developmental abnormalities), the endocrinological status, etc. may also be of importance. Our patient was a low-risk case for vascular injury from the point of view of additional predisposing factors, since she was relatively young (36 years old) and, apart from her papillary thyroid cancer, she did not suffer from any illness during the 10-year clinical course.
A single set of pathological data cannot provide direct evidence against recovery of the morphological and functional structure of the spinal cord from a damaged state that was even more serious than disclosed by the autopsy. However, the pathological state revealed by the post-mortem examination is completely concordant with the functional deficit observed with the culminating clinical symptoms. Thus, it could be concluded that the probability of a pathological recovery displaying parallelism to and explaining the partial restoration of the functional damage is low. This reasoning implies that functional recovery may be supported by a mechanism differing from that destroyed by ionizing radiation.
Radiation myelopathy is generally accepted as not having pathognomic MRI signs. It is safe to state that the signs accompanying this disease and detected by MRI, such as oedema in the acute disease, gadolinium enhancement in the subacute period and atrophy in the chronic phase, are aspecific.18,23,24,28,29,30,31,32 For this reason and in order to gain a deeper insight into the processes underlying the investigated case history, we applied functional imaging. The PET investigations of our patient repeatedly demonstrated an increased FDG accumulation and [15O]butanol perfusion, but a negligible [11C]methionine uptake in the irradiated spinal cord segment.12
In an attempt to interpret the clinical peculiarities in the case history of our patient, together with the results of the PET imaging and histopathology, we refer first of all to the gradual recovery of the functions lost because of radiotherapy. It is generally accepted that remyelination allows the restoration of saltatory conduction and the regaining of the normal function lost during demyelination. Some authors claim that remyelination is a clear prerequisite to a sustained functional recovery.33 This specific regeneration often fails in demyelinating diseases such as multiple sclerosis, although the consecutive functional deficit may be eliminated spontaneously. Recent studies have revealed that many regions of the adult CNS contain neuronal progenitors that have the ability to generate new neurones and glia.34,35,36 Several adult CNS regions exhibit neurotropic-factor responsiveness, including the spinal cord.37 Nieder et al38 surveyed data relating to the pathogenesis of radiation myelopathy and suggested that the administration of cytokines could increase the proliferation of oligodendrocyte progenitors, upregulate the synthesis of myelin constituents and promote myelin regeneration in the adult CNS. Sasaki et al39 demonstrated that transplantation of an isolated bone marrow fraction led to the repair of X-ray-demyelinated adult rat spinal cord axons, apparently as a result of the bone marrow stem cells having been differentiated into myelin-forming cells. Moreover, neurones in several CNS regions extend neurites after injury when presented with growth-promoting substrates. It has also been shown that the number of oligodendrocyte progenitor cells increases following mechanical spinal cord injury.40 Thus, the mature CNS is highly plastic when stimulated by appropriate cues.
The induced differentiation and proliferation of progenitor cells must be extremely low, as judged on the basis of the high percentage of still demyelinated axons in our case, revealed by the histopathology in the involved region of the spinal cord at the end of the 10-year case history. The length of the period of spontaneous remission and the far from complete repair of the injured axons argue strongly against a noteworthy cell proliferation rate related to this special regeneration process. Thus, intensive cell proliferation does not seem a possible explanation for the high FDG accumulation. At the same time, this conclusion accords well with the very low methionine uptake by the irradiated segments of the spinal cord. The subthreshold accumulation of this tracer is additionally concordant with the lack of high-level chronic inflammation involving astrocytosis and/or gliosis required by possible scavenger activity, as revealed by autopsy. This argumentation, and the lack of any clinical sign of acute inflammation simultaneous with the PET imaging, precludes inflammatory processes as a possible explanation for the elevated FDG uptake.
The microvasculature is a ubiqutous system, which often plays a major role in the pathogenesis of radiation damage to normal tissues. A late effect of irradiation is the manifestation of injury not only to the endothelial system, but also to the basement membrane, smooth muscle cells and adventitial tissues.11 There is an irregular proliferation of endothelial cells, leading to vessels of irregular diameter and shape.41,42 Archer and Gardiner43 described a pattern of progressive degenerative vascular changes in response to ionizing irradiation of the retina, ranging from occlusion and microaneurysm formation to microvascular abnormalities such as telangiectasia. As a consequence, the vascular supply to the irradiated structures was altered and resulted in a decreased perfusion. Accordingly, our previous PET data on increased perfusion, although unusual, are consistent with the present morphological observation of the lack of any remarkable sign of vasculopathy at the time of autopsy, as the almost complete lack of this progressive pathological process reliably rules out its earlier existence.
The autopsy revealed neuronal loss in the irradiated segments of the spinal cord, in accord with the detected flaccid paresis. The decrease in the number of viable and functioning cells could not have contributed to the metabolic activity of the appropriate segments, and thus cannot explain the increased FDG acumulation.
The increased metabolic activity in the irradiated segment of the spinal cord cannot be explained either by intensive regenerating processes involving marked cell proliferation, or by vasculopathy or chronic inflammation. In an earlier communication,12 we suggested that all functional imaging findings can be interpreted as consequences of an altered conduction mechanism of the action potential, involving an increased number of sodium channels along the demyelinated segments of the injured axons. During action potential propagation, the activity of these channels of higher than normal density in chronically demyelinated axons induces a greater change in the intracellular sodium concentration, which in turn requires a larger amount of energy to maintain homeostasis. This interpretation is consistent with the autopsy results and is at least partially supported by the latter. This train of thought is strengthened by data from the literature.44,45
References
Burman C et al. Fitting of normal tissue tolerance data to an analytical function. Int J Radiat Oncol Biol Phys 1991; 21: 123–135.
Emami B et al. Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys 1991; 21: 109–122.
Godwin-Austen RB, Howell DA, Worthington B . Observations on radiation myelopathy. Brain 1975; 98: 557–568.
Jellinger K, Sturm KW . Delayed radiation myelopathy in man. Report of twelve necropsy cases. J Neurol Sci 1971; 14: 389–408.
Kristensson K, Molin B, Sourander P . Delayed radiation lesions of the human spinal cord. Report of five cases. Acta Neuropathol 1967; 9: 34–44.
Palmer JJ . Radiation myelopathy. Brain 1972; 95: 109–122.
Reagan TJ, Thomas JE, Colby Jr MY . Chronic progressive radiation myelopathy. Its clinical aspects and differential diagnosis. JAMA 1968; 203: 128–132.
Schultheiss TE, Higgins EM, El-Mahdi AM . The latent period in clinical radiation myelopathy. Int J Radiat Oncol Biol Phys 1984; 10: 1109–1115.
Schultheiss TE, Stephens LC, Maor MH . Analysis of the histopathology of radiation myelopathy. Int J Radiat Oncol Biol Phys 1988; 14: 27–32.
Schultheiss TE et al. Radiation response of the central nervous system. Int J Radiat Oncol Biol Phys 1995; 31: 1093–1112.
Fajardo LF, Berthrong M, Anderson RE . Nervous system. In: Radiation Pathology. Oxford University Press: Oxford-New York 2001; pp 351–363.
É sik O et al. Radiation myelopathy with partial functional recovery: PET evidence of long-term increased metabolic activity of the spinal cord. J Neurol Sci 1999; 163: 39–43.
Sanyal B et al. Radiation myelopathy. J Neurol Neurosurg Psy 1979; 42: 413–418.
Dynes JB, Smedal MI . Radiation myelitis. Am J Roentgenol 1960; 83: 78–87.
Glanzmann C, Aberle HG, Horst W . The risk of chronic progressive radiation myelopathy. Strahlentherapie 1976; 152: 363–372.
Solheim P . Radiation injury of the spinal cord. Acta Radiol Ther Phys Biol 1971; 10: 474–480.
Cohen ME, Duffner PK, Terplan KL . Myelopathy with severe structural derangement associated with combined modality therapy. Cancer 1983; 52: 1590–1596.
Alfonso ER et al. Radiation myelopathy in over-irradiated patients: MR imaging findings. Eur Radiol 1997; 7: 400–404.
Black MJ, Motaghedi B, Robitaille Y . Transverse myelitis. Laryngoscope 1980; 90: 847–852.
Burns RJ, Jones AN, Robertson JS . Pathology of radiation myelopathy. J Neurol Neurosurg Psychiatry 1972; 35: 888–898.
Coy P, Dolman CL . Radiation myelopathy in relation to oxygen level. B J Radiol 1971; 44: 705–707.
Escó R et al. Accidental overirradiation syndrome. Radiother Oncol 1993; 28: 177–178.
Koehler PJ et al. Delayed radiation mylopathy: serial MR-imaging and pathology. Clin Neurol Neurosurg 1996; 98: 197–201.
Komachi H et al. Radiation myelopathy: a clinicopathological study with special reference to correlation between MRI findings and neuropathology. J Neurol Sci 1995; 132: 228–232.
Lampert PW, Davis RL . Delayed effects of radiation on the human central nervous system. ‘Early’ and ‘late’ delayed reactions. Neurology 1964; 14: 912–917.
Marty R, Minckler DS . Radiation myelitis simulating tumor. Arch Neurol 1973; 29: 352–354.
Safwat A et al. Deterministic rather stochastic factors explain most of the variation in the expression of skin telangiectasia after radiotherapy. Int J Radiat Oncol Biol Phys 2002; 52: 198–204.
Calabró F, Jinkins JR . MRI of radiation myelitis: a report of a case treated with hyperbaric oxygen. Eur Radiol 2000; 10: 1079–1084.
Maranzano E et al. Radiation-induced myelopathy in long-term surviving metastatic spinal cord compression patients after hypofractionated radiotherapy: a clinical and magnetic resonance imaging analysis. Radiother Oncol 2001; 60: 281–288.
Melki PS et al. MRI in chronic progressive radiation myelopathy. J Comput Assist Tomogr 1994; 18: 1–6.
Wang P-Y, Shen W-C, Jan J-S . Serial MRI changes in radiation myelopathy. Neuroradiology 1995; 37: 374–377.
Wang P-Y, Shen W-C, Jan J-S . MR imaging in radiation myelopathy. Am J Neuroradiol 1992; 13: 1049–1055.
Keirstead HS, Blakemore WF . The role of oligodendrocytes and oligodendrocyte progenitors in CNS remyelination. Adv Exp Med Biol 1999; 468: 183–197.
Chari DM, Blakemore WF . Efficient recolonisation of progenitor-depleted areas of the CNS by adult oligodendrocyte progenitor cells. Glia 2002; 37: 307–313.
Yamamoto S et al. Transcription factor expression and notch-dependent regulation of neural progenitors in the adult rat spinal cord. J Neurosci 2001; 21: 9814–9823.
Yamamoto S et al. Proliferation of parenchymal neural progenitors in response to injury in the adult rat spinal cord. Exp Neurol 2001; 172: 115–127.
Tuszynski MH, Gage FH . Maintaining the neuronal phenotype after injury in the adult CNS. Neurotrophic factors, axonal growth substrates, and gene therapy. Mol Neurobiol 1995; 10: 151–167.
Nieder C et al. Radiation myelopathy: new perspective on an old problem. Radiat Oncol Invest 1999; 7: 193–203.
Sasaki M et al. Transplantation of an acutely isolated bone marrow fraction repairs demyelinated adult rat spinal cord axons. Glia 2001; 35: 26–34.
Ishii K et al. Increase of oligodendrocyte progenitor cells after spinal cord injury. J Neurosci Res 2001; 65: 500–507.
Baker DG, Krochak RJ . The response of the microvascular system to radiation: a review. Cancer Invest 1989; 7: 287–294.
Cromheecke M et al. Short- and long-term histopathological changes in the canine liver following single high-dose intraoperative radiation therapy (IORT). Int J Radiat Biol 1999; 75: 1437–1448.
Archer DB, Gardiner TA . Ionizing radiation and the retina. Curr Opin Ophthalmol 1994; 5: 59–65.
Felts PA, Baker TA, Smith KJ . Conduction in segmentally demyelinated mammalian central axons. J Neurosci 1997; 17: 7267–7277.
Waxman SG . Demyelinating diseases – new pathological insights, new therapeutic targets. N Eng J Med 1998; 338: 323–325.
Acknowledgements
This work was supported in part by a grant of the Hungarian Research Fund (OTKA T-25827).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Lengyel, Z., Rékó, G., Majtényi, K. et al. Autopsy verifies demyelination and lack of vascular damage in partially reversible radiation myelopathy. Spinal Cord 41, 577–585 (2003). https://doi.org/10.1038/sj.sc.3101480
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101480
Keywords
This article is cited by
-
18F-FDG uptake of the spinal cord was decreased after conventional dose radiotherapy in esophageal cancer patients
Annals of Nuclear Medicine (2016)
-
Lhermitte sign and myelopathy after irradiation of the cervical spinal cord in radiotherapy treatment of head and neck cancer
Strahlentherapie und Onkologie (2012)