Abstract
Study design: A retrospective follow-up study.
Objectives: To assess the value of surgery on the tetraplegic hand to improve its function.
Setting: Spinal unit. Hospital La Fe. Valencia (Spain).
Method: We reviewed the functional results obtained in 15 patients (10 males and 5 females) operated on at our hospital between 1988 and 1997. We performed 66 surgical procedures on 20 upper limbs. After a year or more the patients were evaluated by two independent examiners not related with the surgeons, using the questionnaire of Lamb and Chan modified by Mohammed, taking into account the change in the performance of activities of daily living (ADL), the patient's satisfaction, and the fulfilment of their expectations.
Results: A good or excellent result was obtained in 71.4% of our patients, 85.7% were satisfied with the operation and 57.2% said that the surgery did not meet their expectations. The bad results occurred in patients with previous joint rigidity, ocular sensibility, pain, and lack of motivation.
Conclusion: Hand surgery improved the function of tetraplegics and should be performed more frequently. The hands should be cared for from the very beginning to keep them supple. The information given to the patients should be realistic.
Similar content being viewed by others
Introduction
In tetraplegic patients, hand function is very important for their independence in activities of daily living (ADL) and to increase their quality of life. Most tetraplegics prefer the recovery of hand function to that of the bladder, bowel or even to sexual function.1 Nevertheless hand surgery is not a common procedure in many spinal units and its importance in improving hand function is controversial.
While Guttmann2 (1976), McSweeney3 (1969) and Bedbrook4 (1969) believed that only a very small percentage of tetraplegics (5%) can benefit from hand surgery because they re-adjust the function of their arm and hands if properly rehabilitated, other authors like Möberg5 state that 75% of tetraplegics can obtain benefit from hand surgery.
In any case, the operation should be done at least one and a half years after the spinal cord lesion, once the neurological and functional status has been stabilised.
In 1981 Bedbrook6 considered the surgical rehabilitation of hand function of more value in the flaccid than in the spastic type of hand.
Aim
To assess the value of surgery in the upper limbs of tetraplegics we have focused our study on the following items:
-
1)
Increased hand movement and strength;
-
2)
Improvement in the ADL;
-
3)
Patient's satisfaction;
-
4)
Fulfilment of patient's expectations;
-
5)
Surgical complications.
Methods
We have reviewed the results obtained in 20 upper limbs of 15 patients (10 males and 5 females) operated on to improve hand function, between 1988 and 1997 at the Hospital La Fe (Valencia, Spain).
The patients were recruited when they attended hospital for check-up according to the following criteria:
-
Spinal cord lesion stabilized
-
More than one year after spinal cord lesion
-
Good general condition
-
Motivated and willing to improve their hand function
-
Supple hand and enough muscles to transfer.
Only 10% of the patients approached that fulfilled the selection criteria were willing to be operated on.
The age of the patients at the first operation ranged from 20 to 62 years (mean age 42 years). Regarding the aetiology, in nine cases (60%) the spinal injury was due to a Road Traffic Accident; in three cases (20%) to a fall from a height; and in the remaining three cases (20%) to a medical disease.
According to the level of the lesion: 1 case C4 incomplete; 4 cases C5 (3 incomplete and 1 complete); 5 cases C6 (3 incomplete and 2 complete); 5 cases C7 (4 incomplete and 1 complete). The mean time elapsed from the lesion to the first operation was 34 months, ranging from 15 to 239 months. We performed 66 surgical procedures on the 15 patients.
The patients were classified according to the International Classification for Surgery of the Hand in Tetraplegia7 (Table 1) developed at the International Conference held in Edinburgh in 1978, and modified in 1984. It takes into account the residual motor strength below the elbow, considering that only the muscles graded 4 or 5 according to the Medical Research Council Scale (MRCS) are adequate for muscle transfer, as well as the sensibility in thumb and index. The sensibility was evaluated by the two-point discrimination test in the thumb and the index. If it is lower than 10 mm the patient's hand belongs to the group Cutaneous (‘Cu’−), and if it is higher than 10 mm and the patient needs the visual help he is classified in the group Ocular (‘O’−).
Regarding the sensibility, that is essential for hand function, operations were carried out on 13 upper limbs belonging to the Cutaneous group (‘Cu’−) and seven upper limbs to the Ocular group (‘O’−). Table 1.
One patient had pain in both hands, another rigidity, and two had spasticity grade 3 of Ashworth in both upper limbs. The three patients with rigidity or spasticity were specially motivated and willing to be operated on, and the passive extension of fingers and wrist was good enough to allow surgery.
The pre-operative evaluation consisted of:
-
Muscle balance
-
Range of joint motion
-
Two-point discrimination test
-
Identification of other pathologies like pain or spasticity
-
Patient motivation (good or bad)
The aim of the surgery was to:
-
1)
Restore active elbow extension;
-
2)
restore key pinch;
-
3)
restore grasp;
-
4)
obtain a good balance of the intrinsic muscles of the hand.
The surgical techniques were based on muscle transfer, tendon lengthening, tenodesis or arthrodesis. Timing of the surgical operation is very important and it is necessary to wait at least one year since the spinal lesion once the neurological lesion is stable and the recovery of hand function has reached a plateau.8
Our group was very heterogeneous and required different surgical approaches (Table 2):
-
1)
In Tetraplegics, elbow extension is very important to obtain more stability in their wheelchair and to raise the hands to reach elevated objects. The activity of the triceps may improve the function of its antagonist the brachioradialis (BR) when it is transferred.9,10 When active extension of the elbow was absent, it was restored in the first instance transferring the posterior deltoid according to Möberg's technique modified by Hentz11 in the first three cases and by Castro-Lopez12 in the last three.
-
2)
Afterwards the aim of our operation was to obtain the opposition between thumb and index (key-pinch) if there were few muscles to transfer, or if possible a prehension grasp with the triphalangic fingers.13 Wrist extension is essential for hand function, so if it was not present we transferred the BR to Extensor Carpi Radialis Brevis (ECRB) to obtain wrist extension, and tenodesis of the Flexor Pollicis Longus (FPL) to achieve key pinch. The stability of the carpo-metacarpal (CMC) joint is necessary for key pinch and it is stabilized by the Abductor Pollicis Longus (APL). If we do not have enough muscles to transfer to the APL we perform arthrodesis of the CMC joint at 45° of palmar abduction and 30° of abduction.8,13
-
3)
If active Extension of the wrist was present and there were enough muscles to transfer, we restored the key-pinch and grasp (according to House's technique14,15) in two stages.13,16
-
a)
Extensor stage: Extension of the fingers and thumb is very important for hand function, so before we activate its flexors we transfer the BR, Extensor Carpi Radialis Longus (ECRL) or Pronator Teres (PT) to the extensor tendons: Extensor Digitorum Comunis (EDC) and Extensor Pollicis Longus (EPL), or, if it is not possible because the former muscles are too weak or paralysed, we perform a tenodesis of the extensor tendons into the radius.8,13 (Table 2).
-
b)
Flexor stage: It is performed when extension of the fingers is functioning adequately, usually not before 6 months. For a key pinch it is necessary to activate the FPL, which in our cases has been done with the BR, ECRL or ECRB. Flexion of the fingers has been achieved activating the Flexor Digitorum Profundus (FDP) with the PT, ECRL or BR (Table 2).
-
a)
-
4)
To avoid hyperextension, or to achieve flexion of the MCP joints – very important in the index finger for the key pinch – we have performed the Zancolli's lasso8,13,17 of the Flexor Digitorum Superficialis (FDS) to the A1 pulleys of the 2nd to 5th fingers in the extensor stage, associated to the arthrodesis of the CMC joint.
-
5)
Tendon elongations were made in shortened flexors.
Postoperative program
During the period of immobilization, lasting for 3 or 4 weeks, the patients are encouraged to perform isometric contractions that are not too painful or too strong, in order to increase muscle strength.
When the plaster is removed and the patients can move their hands, they start functional activities with tasks that include the movements gained after the operation. The vision may help to control the movements when the sensibility is poor.
The patients remained in the hospital for 3–4 weeks, and could go home after plaster removal and the exercise programmes had been evaluated.
The postoperative evaluation was performed by two independent examiners not related to the surgical procedure one or more years after operation (mean time elapsed 50.5 months). The following points were considered:
-
1)
Strength of elbow extension, pinch and grasping. (Dynamometer ULRICH. ULM/DONAU)
-
2)
Subjective assessment of ADL using the questionnaire of Lamb and Chan modified by Mohammed18 (Appendix 1) that evaluates the change in ADL by means of 35 questions concerning mobility, dressing, washing and toileting, feeding and other activities. Every item is scored as follows: If much worse=0; Worse=1; Unchanged=2; Improved=3; Greatly improved=4. The overall results are considered as follows: Poor: 0–69 points. Fair: 70–84 points. Good: 85–101 points. Excellent: 102–136 points.
-
3)
General opinion of the patient (Better or Worse).
-
4)
Fulfilment of patient's expectations (Yes or Not).
-
5)
Surgical complications.
Recently new classifications like that of Rancho Los Amigos for hand function19 have been published, but we have preferred to use the above mentioned classification.
The evaluation of the results was based on 14 patients (19 hands) as one of them died in a traffic accident before evaluation.
Results
Strength
The strength of the key-pinch was measured in 14 upper limbs, with an average of 17.2 kPa, ranging from 5 to 50.
The grasp strength, measured in 14 hands, ranged from 3 to 45 kPa, the average was 18.8.
No relation was found between the activities of daily living test and the key-pinch strength (P=0.7976), neither with the grasp strength (P=0.6948). The improvement in the activities of daily living was not directly related to the increase in key-pinch or grasp strength, probably due to the confusing factor of measuring only muscle strength without taking into account sensibility and coordination.
The modification of the ADL, according to the Mohammed et al18 questionnaire, was as follows:
-
Excellent (3 cases): 21.4%;
-
Good (7 cases): 50%;
-
Fair (2 cases): 14.3%;
-
Poor (2 cases): 14.3%.
The score ranged between 54 and 122 points.
Patient's satisfaction
Twelve patients said they were better after the operation (85.7%) and two that had previous spasticity said they were worse (14.3%), both belonging to the Ocular group.
Fulfilment of patient's expectations
In only six cases (42.8%) the patients felt that the operation had fulfilled their expectations, and eight of them (57.2%) expected better results.
Complications of the surgery
After 66 surgical procedures, we had eight complications (12.1%) detailed in Table 3. We had no wound infections or ruptures of anastomoses. The most serious complication was pain suffered by the patient prior to surgery and subsequently aggravated by the operation.
Sensibility
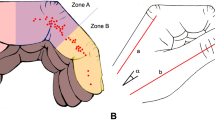
Ninety per cent of patients with sensibility Cu− obtained a good or excellent result in the ADL questionnaire, while in the group of patients with O− sensibility, 75% of the result was fair or poor. Figure 1Figure 2
Discussion
It is very difficult to assess the value of hand surgery in tetraplegic patients because of the many differences between them regarding their neurological lesion, motivation and also the surgical procedures employed. Even greater differences may exist between both upper limbs of the same patient.
Some of our patients may have improved more in their hand function if all the surgical interventions planned had been performed, but for several reasons further surgery had been refused.
Four patients were not willing to allow the surgical programme to be completed because they though that the possible functional benefits did not justify the longer hospital stay. In two of these cases the operation was advised to correct the failure of arthrodesis.
Different authors use different methods of evaluation, which makes it more difficult to compare the results.
Although we measured the strength of the key-pinch and the grasp we have focused our attention on the functional and psychological results of the surgery, that is to say on the improvement of the performance of the ADL, on the patients' satisfaction, and on the fulfilment of their expectations. These last two items are included in the Mohammed et al scale18 but we thought it was worthwhile to consider them separately.
On the whole our results do not differ very much from those of other authors employing the same scale to evaluate their results. We obtained good or excellent results in 10 (71.4%) of our cases, Mohammed et al18 in their larger group of 57 patients (97 upper limbs) obtained the same results in 75% of the cases, and Lamb and Chan20 in their study of 41 patients, obtained 83% of good results. The positive results of other studies and the evaluation method employed are detailed in Table 4.
The bad results were obtained in the patients with a previous history of pain, spasticity and O-sensory classification that we believe should have been a contraindication for operation. The majority of our patients (85.7%) were satisfied with the results of the surgery performed and with the functional improvement, and only two (14.3%) said they were worse, due to pain in one case and hand rigidity in another. As Möberg pointed out, a rigid hand impairs the familiar and social relationship.
Regarding the fulfilment of their expectations, eight (57.2%) patients said that they had expected more from the surgery and were somewhat disappointed in spite of the functional improvement.
The difference between the functional improvement and the fulfilment of patient's expectations can be explained by inadequate or too optimistic information given by the surgeon in charge. This point has already been corrected. As clearly stated by Möberg,21 the hand function depends on its mobility and its sensibility. If by means of muscle transfer the mobility is restored but there is no sensibility, the hand is blind, requires the aid of the vision, and consequently its function is poor.
Some authors state that the patients with O− sensibility should not be submitted to hand surgery22 and the majority include in their criteria for surgery a two-point discrimination test in thumb and index lower than 10 mm,20 or 15 mm.23
This was clear in our study as 90% of the patients with Cu− sensibility achieved good or excellent results, while in the group of O− sensibility only 25% achieved good results. Authors such as House15 and Vanden Berghe24 obtained satisfactory functional results in patients with O− sensibility.
Other authors include in their studies, patients with O− sensibility but do not relate the results obtained with the type of sensibility (Rieser,25 Ejeskär,26 and Paul27).
The results of hand surgery are usually bad in patients with a previous history of pain, rigidity, O− sensibility and lack of motivation, and therefore these points should be considered before surgery.
Conclusions
-
1)
This study shows that hand function was improved in 10 out of 14 patients.
-
2)
As we found bad results in patients with pain, joint rigidity, severe spasticity and O− sensibility, we suggest that the patient selection for hand surgery should be very strict, excluding these conditions.
-
3)
The patients should be informed realistically of the possible functional gains, so the results will meet their expectations.
-
4)
Hand surgery in tetraplegics should be offered more often and by expert hand surgeons. Their hands should be cared for from the very beginning for a possible operation in the future.
References
Hanson RW & Franklin WR . Loss in relation to other sexual losses for spinal cord injured males. Arch Phys Med Rehabil 1976; 57: 291–293.
Guttmann L Spinal cord injuries. Comprehension, management and research. 2nd edn. Oxford: Blackwell Scientific Publications, 1976; pp 558–560.
McSweeney T . Discussion to Freehafer AA. Care of the hand in cervical spinal cord injuries. Paraplegia 1969; 7: 118–130.
Bedbrook G . Discussion to Freehafer AA. Care of the hand in cervical spinal cord injuries. Paraplegia 1969; 7: 118–130.
Moberg E . Surgical treatment for absent single-hand and elbow extension in quadriplegia. J Bone Joint Surg 1975; 57: 196–206.
Bedbrook G The care and management of spinal cord injuries. New York: Springer-Verlag, 1981; pp 149–151.
McDowell CL, Moberg EA & House JH . The second International Conference on Surgical Rehabilitation of the Upper Limb in Traumatic Quadriplegia. J Hand Surg 1986; 11A: 604–608.
McDowell CL . Tetraplegia. In: Green D (ed). Operative Hand Surgery. 2nd edn. New York: Churchill Livingstone. 1988; pp 1597–1617.
Moberg E . Reconstruction hand surgery in tetraplegia, stroke and cerebral palsy. Some basic concepts in physiology and neurology. J Hand Surg 1976; 1: 29–34.
Ejeskär A, Dahllöf AG & Möberg E . Upper limb surgery in Tetraplegia. In: Hunter JM. Rehabilitation of the hand: Surgery and Therapy. 4th edn. Saint Louis: Mosby, 1995; pp 1413–1421.
Hentz VR, Brown M & Keoshian LA . Upper limb reconstruction in quadriplegia: functional assessment and proposed treatment modifications. J Hand Surg 1983; 8: 119–131.
Castro-Sierra A & Lopez-Pita A . A new surgical technique to correct triceps paralysis. The Hand 1983; 15: 42–45.
Zancoli EA Structural and dynamic bases of hand surgery. 2nd edn. Philadelphia: JR Lippincott, 1979; pp 229–262.
House JH & Shannon MA . Restoration of strong grasp and lateral pinch in tetraplegia: a comparation of two methods of thumb control in each patient. J Hand Surg 1985; 10A: 22–29.
House JH, Comadoll J & Dahl AL . One-stage key pinch and release with thumb carpal-metacarpal fusion in tetraplegia. J Hand Surg 1992; 17A: 530–538.
House JH . Reconstruction of the thumb in tetraplegia following spinal cord injury. Clin Orthop 1985; 195: 117–128.
Zancolli E . Surgery of the quadriplegic hand with active strong wrist extension preserved: a study of 97 cases. Clin Orthop 1975; 112: 101–113.
Mohammed KD, Rothwell AG, Sinclair SW, Willems SM & Bean AR . Upper-limb surgery for tetraplegia. J Bone Joint Surg 1992; 74B: 873–879.
Waters RL, Sie IH, Gellman H & Tognella M . Functional hand surgery following tetraplegia. Arch Phys Med Rehabil 1996; 77: 86–94.
Lamb DW & Chan KM . Surgical reconstruction of the upper limb in traumatic tetraplegia. J Bone Joint Surg 1983; 65B: 291–298.
Moberg E . Surgical rehabilitation of the upper limb in tetraplegia. Paraplegia 1990; 28: 330–334.
Freehafer AA . Tendon transfers in tetraplegia patients: The Cleveland experience. Spinal Cord 1998; 36: 315–319.
Waters R, Moore KR, Graboff SR & Paris K . Brachio-radialis to flexor pollicis longus tendon transfer for active lateral pinch in the tetraplegic. J Hand Surg 1985; 10A: 385–391.
Vanden Berghe A, Van Laere M, Hellings S & Vercauteren M . Reconstruction of the upper extremity in tetraplegia: functional assessment, surgical procedures and rehabilitation. Paraplegia 1991; 29: 103–112.
Rieser TV & Waters RL . Long term results of the Moberg Key grip procedure. J Hand Surg 1986; 11A: 724–728.
Ejeskär A & Dallhöf A . Results of reconstructive surgery in the upper limb of tetraplegic patients. Paraplegia 1988; 26: 204–208.
Paul SD, Gellman H, Waters R, Willstein G & Tognella M . Single-stage reconstruction of key pinch and extension of the elbow in tetraplegic patients. J Bone Joint Surg 1994; 76A: 1451–1456.
Gansel J, Waters R & Gellman H . Transfer of the pronator teres tendon to the tendons of the flexor digitorum profundus in tetraplegia. J Bone Joint Surg 1990; 72A: 427–432.
Author information
Authors and Affiliations
Appendix 1. Assessment of ADL according to Mohammed et al. (1983)18
Appendix 1. Assessment of ADL according to Mohammed et al. (1983)18
Mobility:
1 Raise yourself in seat
2 Propel wheelchair on level ground
3 Propel up and down a gentle slope
4 Transfer from wheelchair to bed
5 Drive a car
Dressing:
6 Upper garments
7 Lower garments
Communication:
8 Using a telephone
9 Writing or typing
10 Handling money
Washing and toileting:
11 Getting in and out of shower/bath
12 Washing and drying upper limbs
13 Washing and drying lower limbs
14 Cleaning teeth
15 Shaving or applying cosmetics
16 Brushing hair
17 Bladder: use of urodome or catheter
18 Bowel: inserting suppositories and cleaning after bowel action
Feeding and drinking:
19 Use of cutlery
20 Cutting meat
21 Holding a cup or glass
Miscellaneous:
22 Making a meal or snack
23 Reaching a shelf above
24 Opening and closing drawers
25 Operating buttons
26 Turning pages in book/newspaper
27 Picking up things from the floor
28 Using a key
29 Putting a plug into a point
30 Have your educational vocational options changed?
31 Were your overall expectations met?
32 Have you become more independent?
33 Has your self-confidence changed?
34 Has the surgery changed your quality of life?
35 Any comments.
Points
Much worse 0
Unchanged 1
Improved 3
Greatly improved 4
Overall results
Poor: 0 to 69 points.
Fair: 70 to 84 points.
Good: 85 to 101 points.
Excellent: 102 to 136 points.
Rights and permissions
About this article
Cite this article
Forner-Cordero, I., Mudarra-García, J., Forner-Valero, J. et al. The role of upper limb surgery in tetraplegia. Spinal Cord 41, 90–96 (2003). https://doi.org/10.1038/sj.sc.3101415
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101415
Keywords
This article is cited by
-
Surgical Rehabilitation of a Tetraplegic Hand: Comparison of Various Methods of Reconstructing an Absent Pinch and Hook
HAND (2014)
-
Identification of Three Movement Phases of the Hand during Lateral and Pulp Pinches Using Video Motion Capture
HAND (2013)
-
Long-term patient satisfaction after reconstructive upper extremity surgery to improve arm–hand function in tetraplegia
Spinal Cord (2011)
-
Upper limb reconstructive surgery uptake for persons with tetraplegia in New Zealand: a retrospective case review 2001–2005
Spinal Cord (2010)