Abstract
Altered expression of central muscarinic and nicotinic acetylcholine receptors in hippocampal and cortical regions may contribute to the cognitive impairment exhibited in patients with schizophrenia. Increasing cholinergic activity through the use of a cholinesterase inhibitor (ChEI) therefore represents a possible strategy for cognitive augmentation in schizophrenia. We examined the efficacy and safety of the ChEI donepezil as cotreatment for mild to moderate cognitive impairment in schizophrenia or schizoaffective disorder in a prospective, 12-week, placebo-controlled, double-blind, parallel-group study. In total, 250 patients (18–55 years) with schizophrenia or schizoaffective disorder who were clinically stabilized on risperidone, olanzapine, quetiapine, ziprasidone, or aripiprazole, alone or in combination, were enrolled at 38 outpatient psychiatric clinics in the United States. Patients were randomized to donepezil 5 mg q.d. for 6 weeks then 10 mg q.d. for 6 weeks, or placebo administered as oral tablets. The primary outcome measure was the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) neurocognitive battery composite score. In the intent-to-treat sample (donepezil, n=121; placebo, n=124), both treatments showed improvement in the composite score from baseline to week 12. At week 12, cognitive improvement with donepezil was similar to that with placebo (last-observation-carried-forward effect size, 0.277 vs 0.411; p=0.1182) and statistically significantly inferior for the observed-cases analysis (0.257 vs 0.450; p=0.044). There was statistically significant improvement in the Positive and Negative Syndrome Assessment Scale negative symptoms score for placebo compared with donepezil, while total and positive symptom scores were similar between both treatments. Statistically significant improvements in positive symptoms score and Clinical Global Impression-Improvement for donepezil compared with placebo were noted at Week 6. Treatment-emergent adverse events (AEs) were observed for 54.5% of donepezil- and 61.3% of placebo-treated patients; most AEs were rated as mild to moderate in severity. Donepezil was safe and well-tolerated but was not effective compared with placebo as a cotreatment for the improvement of cognitive impairment in this patient population. A significant and surprisingly large placebo/practice effect was observed among placebo-treated patients, and is a serious consideration in future clinical trial study designs for potential cognitive enhancing compounds in schizophrenia.
Similar content being viewed by others
INTRODUCTION
Schizophrenia and schizoaffective disorders are characterized by a diverse array of symptoms, including positive symptoms, negative symptoms, mood disturbances, and cognitive dysfunction (American Psychiatric Association, 1994). Cognitive impairment often accompanies (Saykin et al, 1994) or precedes (Fuller et al, 2002; Hawkins et al, 2004) the onset of psychosis, and remains throughout the course of illness (Green and Braff, 2001; Heinrichs and Zakzanis, 1998; Bilder et al, 2000). The range of cognitive impairments is diverse and can include impairment of verbal memory, attention, general intelligence, spatial ability, and executive function. Cognitive impairment has considerable detrimental effects on the social and vocational outcomes of schizophrenia patients, with the severity of impairment being closely related to the severity of community and work disability (Green, 1996; Green et al, 2004). To date, studies with first- and second-generation antipsychotic drugs have been unable to demonstrate consistently marked effects on cognitive function in schizophrenic patients (Harvey and Keefe, 2001; Keefe et al, 1999, 2007; Woodward et al, 2005), resulting in an increased emphasis on testing other agents for efficacy in cognitive enhancement.
Acetylcholine (ACh) plays a key role in working memory and reference memory. Disruption of the septo-hippocampal and nucleus basalis of Meynart-cortical cholinergic projection pathways in animal models produce memory deficits that can be reversed by cholinergic supplementation strategies (eg physostigmine administration (Mandel et al, 1989) or ACh-producing cell grafts at the lesion site (Winkler et al, 1995). Memory impairment can be induced in healthy human subjects with scopolamine, while cholinomimetics drugs can enhance memory in healthy individuals (Sitaram et al, 1978). A major cholinergic deficit is now a well-established contributor to the symptomatology of Alzheimer's disease (AD), a condition primarily characterized by memory loss and cognitive dysfunction.
Although the gross neuropathology of the cholinergic system observed in AD is not exhibited in the brains of patients with schizophrenia, alterations in central cholinergic function have been described. The activity of choline acetyltransferase, a biomarker of cholinergic neuronal function, in the parietal cortex of patients with schizophrenia at postmortem negatively correlated with the severity of cognitive impairment scored by the Clinical Dementia Rating Scale during antemortem assessments (Powchik et al, 1998).
Alterations in the density and expression of ACh receptors in the brains of patients with schizophrenia has been demonstrated with quantitative autoradiography. The binding density of [3H]pirenzepine, a radioligand selective for the M1 and M4 muscarinic receptor subtypes, is reduced in postmortem cortical tissue and several areas of the hippocampal formation (dentate gyrus, CA1–CA4 subdivisions of Ammon's Horn, subiculum and parahippocampal gyrus) of patients with schizophrenia compared to control subjects (Crook et al, 2000, 2001). A significantly lower level of [3H]pirenzepine binding was found in cortical areas corresponding to Brodmann's areas 9 and 46 in the tissue from unmedicated patients compared with controls and in Brodmann's areas 8, 9, 10, and 46 in medicated patients compared with unmediated counterparts (Crook et al, 2001). Decreases in muscarinic receptor availability has been further shown in the cortex, basal ganglia, and thalamus of living unmedicated patients compared with a matched control group, using [123I]iodoquinuclidinyl benzilate single positron emission computed tomography (Raedler et al, 2003). Decreased binding of α-bungarotoxin (Freedman et al, 1995) or decreased immunoreactivity to α(7) nicotinic acetylcholine receptors (nAChR) (Guan et al, 1999) in postmortem hippocampal and cortical tissue from patients with schizophrenia in comparison to matched controls also implicate this receptor subtype in the neuropathophysiology of schizophrenia. Studies in smokers with and without schizophrenia have further indicated a role for the α(4)β(2) nAChR. Whereas this receptor subtype was upregulated in the cortex, hippocampus, and caudate in smokers without schizophrenia its levels were reduced in patients with schizophrenia who smoke (Breese et al, 2000).
Thus, cholinergic enhancement strategies may well prove to be useful in the treatment of cognitive dysfunction in patients with schizophrenia. Currently available treatments with potential to enhance cognitive function in these patients include cholinesterase inhibitors (ChEIs; including donepezil, rivastigmine, and galantamine), muscarinic and nicotinic agonists, and allosteric potentiators of nicotinic function (Friedman, 2004).
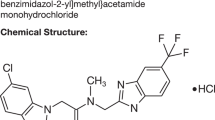
The ChEI donepezil is approved for the treatment of mild to severe AD at doses of upto 10 mg/day (Aricept, Eisai Inc. (donepezil hydrochloride tablets), package insert, Teaneck, NJ, USA). Double-blind, randomized, placebo-controlled clinical studies have consistently demonstrated that donepezil (5 or 10 mg/day) provides significant improvement in cognition and global function in AD patients (Rogers et al, 1998a, 1998b; Burns et al, 1999; Winblad et al, 2001; Whitehead et al, 2004). The substantial need for cognitive improvement in patients with schizophrenia raises the question of whether donepezil might be able to provide benefit.
Although various pilot studies have evaluated donepezil as an adjunct to commonly prescribed antipsychotic medications in schizophrenic patients, the results have proved inconclusive. While two case studies and a small, open-label study revealed some cognitive improvement with donepezil treatment (Buchanan et al, 2003; MacEwan et al, 2001; Risch et al, 2001), four double-blind, placebo-controlled trials did not (Freudenreich et al, 2005; Friedman et al, 2002; Tugal et al, 2004; Fagerlund et al, 2007). It is likely that the latter trials were not sufficiently powered to detect a treatment effect on cognition, since no study enrolled more than 36 patients.
The present study evaluated the efficacy and safety of donepezil as a cotreatment for cognitive impairment in schizophrenia or schizoaffective disorder patients stabilized with selected second-generation antipsychotic medications. This study is the first large-scale, double-blind, placebo-controlled study of an ChEI in patients with schizophrenia/schizoaffective disorder to use a comprehensive neurocognitive battery to evaluate cognitive improvement in patients with stable symptoms and mild to moderate illness.
METHODS
Participants
Male or female patients between 18 and 55 years of age with a primary diagnosis of schizophrenia or schizoaffective disorder (any subtype, as defined in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)) (American Psychiatric Association, 1994) were eligible for study enrollment. Patients were required to be clinically stable (no psychiatric hospitalization for at least 6 months before screening, and clinical symptoms documented as stable for at least 3 months before screening), and to have complied with and tolerated a current dose regimen of a selected second-generation antipsychotic medication (risperidone, olanzapine, quetiapine, ziprasidone, or aripiprazole, alone or in combination) for a minimum of 3 months before joining the study.
To be eligible for study enrollment, patients were required to be no more than moderately ill (determined by the physician as a score of ⩽4 on the Clinical Global Impression-Severity (CGI-S)), to have a Positive and Negative Syndrome Assessment Scale (PANSS) total score ⩽80, to have cognitive impairment (indicated by a z-score between −0.5 and −2.5 SD inclusive on the Brief Assessment of Cognition in Schizophrenia (BACS) composite score), and to have a minimum of a sixth-grade reading level (as measured by the Wide Range Achievement Test Reading Subtest (WRAT-3 Reading)). Patients were required to have no history of DSM-IV-defined substance abuse or dependence (other than nicotine dependence) for at least 1 year before screening and to provide a negative urine drug screen for amphetamines, cocaine, opioids, and phencyclidine before study enrollment.
Patients were excluded from study entry if they met any of the following criteria: diagnosis of any DSM-IV Axis I psychiatric disorder other than schizophrenia or schizoaffective disorder; risk of suicide, violent behavior, or homicide; hypersensitivity to a piperidine derivative or ChEI; prior use of an approved or unapproved ChEIs (donepezil, galantamine, metrifonate, physostigmine, rivastigmine, or tacrine); a history of seizure disorder or cognitive deficit following head trauma; and current use of typical antipsychotics, anticholinergic medications, or antiparkinsonian agents.
In addition, patients were excluded if they had significant co-morbidity, including any condition liable to affect absorption, distribution, or metabolism of the study medication; clinically significant obstructive pulmonary disease or asthma untreated for >3 months; recent (⩽2 years) hematologic/oncologic disorders; clinically significant gastrointestinal, renal, hepatic, endocrine, or cardiovascular disease; unstable hyperthyroidism; diabetes mellitus not adequately controlled by diet or oral medication; and chronic hepatitis. Patients who were HIV positive or had a history of, or presented with, QTc prolongation were also excluded. Female patients who were pregnant, not using an acceptable form of contraception, or breastfeeding were excluded from study entry.
Written, informed consent was obtained from each patient. The study was carried out in accordance with the Declaration of Helsinki (World Medical Association declaration of Helsinki, 1997) and its amendments or the laws and regulations of the locality in which the research was conducted, whichever afforded the greater protection to the individual. The study protocol, any study modifications, and consent procedures were approved by the Institutional Review Board, operating in accordance with current federal regulations.
Study Design
This was a 12-week, randomized, double-blind, placebo-controlled, multicenter study with two parallel groups. A total of 250 patients were enrolled at 38 outpatient psychiatric clinics in the United States. Patients participated in six scheduled visits during the course of 12 weeks: screening (days 28−7), baseline (day 1), week 3 (day 21±3), week 6 (day 42±3), week 9 (day 63±3), and week 12 (day 84±3 or early termination). Primary and secondary assessments were administered at baseline, 6 and 12 weeks after initiation of treatment.
Preclinical and clinical procedures included informed consent, a medical history, complete physical examination (including vital signs), and a 12-lead electrocardiogram.
The primary efficacy measure was a composite score derived from the individual test scores from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) neurocognitive battery (Keefe et al, 2003, 2006). Cognitive tests that comprise the CATIE battery include: Controlled Oral Word Association Test (COWAT letter fluency) (Benton and Hamsher, 1989); Category Instances (semantic fluency) (Benton and Hamsher, 1989); Wechsler Intelligence Scale for Children-Third Edition (WISC-III) Mazes (Wechsler, 1991); Hopkins Verbal Learning Test (HVLT) (Brandt, 1991); Wechsler Adult Intelligence Scale-Revised (WAIS-R) Digit Symbol Test (Wechsler, 1981); letter-number test of auditory working memory (Gold et al, 1997); grooved pegboard (Matthews and Klove, 1964); computerized Continuous Performance Test (CPT) (Cornblatt et al, 1988, 1997); computerized Test of Visuospatial Working Memory Test (VWMT) (Hershey et al, 1998); and computerized Wisconsin Card Sorting Test (WCST64) (Heaton et al, 1993).
Secondary psychometric and neurologic examinations included CGI-S, CGI-Improvement (CGI-I) (US Department of Health, 1976a); PANSS (Kay et al, 1987); Montgomery-Asberg Depression Rating Scale (MADRS) (Montgomery and Asberg, 1979), Abnormal Involuntary Movement Scale (AIMS) (US Department of Health, 1976b), Simpson Angus Scale (SAS) (Simpson and Angus, 1970); Barnes Akathisia Scale (BAS) (Barnes, 1989), Patient Perception of Function Scale (PPFS) (MacEwan et al, 2001), and Role Functioning Scale (RFS) (McPheeters, 1984).
Clinical laboratory evaluations included hematology, clinical chemistry, thyroid profile, routine urinalysis, urine drug screen, hepatitis B surface antigen, glycosylated hemoglobin A1c, plasma assays for antipsychotic medications, and pregnancy test.
Safety, tolerability, and compliance evaluations included all medication use, adverse events (AEs), study drug dispensing, and medication compliance. AEs were coded to standard preferred terms using a Pfizer-modified form of the Coding Symbols for Thesaurus of Adverse Reaction Terms (COSTART) dictionary (fourth edition, 1993) (Department of Health and Human Services, 1993). AEs were assessed for severity (mild, moderate, or severe) and relationship to study drug (related or not related).
Treatments
Study drug was initiated on day 1 immediately following baseline evaluation. Study drugs, provided as film-coated tablet by Eisai Inc., were supplied in packaging that blinded the patient and investigator to the treatment administered. Patients were randomized to receive either donepezil 5 mg q.d. (one donepezil 5-mg tablet and one matching placebo tablet) for 6 weeks followed by donepezil 10 mg q.d. (two donepezil tablets, 5 mg each) for a further 6 weeks, or placebo (two placebo tablets) for 12 weeks. If the patient was unable to tolerate an increase in the dose of donepezil or placebo, the dose was temporarily reduced to 5 mg q.d. and the patient was rechallenged with 10 mg q.d. after 7–10 days. Patients who were unable to tolerate the rechallenge were allowed to continue in the study on 5 mg q.d.
Compliance with study treatment was monitored at each study visit by checking tablets returned from the previous treatment period. Compliance rate was defined as 100 multiplied by the number of tablets taken during a time interval/number prescribed during the interval. An overall compliance rate was calculated based on the total number of tablets taken during the subject's treatment period. Compliance was also calculated for study periods baseline—week 6 and week 7–12. If the date of dosing was on or before day 42, compliance statistics were slotted into week 1–6. If the date of dosing was after day 42 then dosing statistics were slotted into weeks 7–12. Compliance of <80% made the visit nonevaluable. Following two nonevaluable visits, a patient was discontinued for noncompliance.
Throughout the study period patients continued to receive the second-generation antipsychotic medication in use at study entry. The use of adjunctive anticholinergic medication for emergent extrapyramidal symptoms following study entry was not permitted. Patients on stable doses of selected antidepressants and antiepileptics were permitted. Anxiolytics were excluded. Sedative hypnotics were limited to a maximum of 3 days use in any 2-week period; in addition, these medications were not to be taken within 48 h of testing. Nicotine dependence was permitted.
Statistical Analysis
The planned sample size for this study was 100 randomized patients per treatment group, with each patient contributing at least 1 baseline and 1 post-randomization CATIE neuropsychological battery assessment per treatment arm. This calculation was based on a two-sided test with a type I error rate of 5 and 80% power to show statistically significant differences between treatments (assuming a between treatments effect size of 0.4 in the CATIE composite score). An assumed patient dropout rate of 20% led to a randomization target of 125 patients per treatment group.
Patients were stratified before randomization according to the type of antipsychotic used before screening (risperidone, olanzapine, quetiapine, ziprasidone, or other agent (including aripiprazole)), and length of illness (less than or greater than 5 years of illness). Within each stratum, patients were randomized 1 : 1 to the donepezil or placebo treatment arms according to a computerized randomization schedule.
Efficacy outcomes were evaluated for two samples: the intent-to-treat (ITT) sample (all patients who received at least one dose of study drug, had a baseline visit, and had at least one efficacy evaluation after the start of treatment irrespective of compliance), and the fully evaluable sample (all ITT patients who met all inclusion and exclusion criteria and had a study drug compliance rate of ⩾80%). All efficacy outcomes were analyzed using OC analysis at the time points specified and week 12 last observation carried forward (LOCF). The safety sample included all patients who had received at least one dose of study drug.
The primary efficacy analysis was based on the change from baseline in the CATIE neurocognitive composite score, evaluated in the ITT sample at the last post-randomization visit (ie week 12 LOCF). The composite score is the weighted sum of the 10 individual standardized test scores, where the weights are derived from the first component from the principal components analysis of the pooled CATIE scale scores at baseline. The test scores were standardized for each patient by subtracting the baseline sample mean for that measure and dividing the difference by the baseline SD for the sample. An increase in the score demonstrated cognitive improvement. Secondary efficacy analyses included the rating scales and the 10 individual CATIE neurocognitive test scores.
Patient disposition, treatment group comparability (demographic and baseline variables, medical history, and exposure to study medication), and safety assessments were summarized using descriptive statistics. For efficacy variables, an analysis of covariance model or an analysis of variance model was used. A test result was considered significant if p<0.05 for a two-sided test. No statistical tests were performed on the safety variables.
The ITT sample was subjected to additional secondary analyses that used baseline smoking status, antipsychotic medication use during the study, and baseline cognitive impairment (defined by CATIE neurocognitive composite score) as independent variables. None of these secondary analyses were corrected for multiple comparisons.
The association between change in cognition and change in relevant clinical factors such as positive symptoms and negative symptoms as measured by the PANSS was determined with Pearson correlations.
RESULTS
Patient Disposition
The first patient visit took place in December 2002 and the last patient visit in July 2004. Out of 418 patients screened at 38 sites throughout the United States, 251 patients (donepezil, 124; placebo, 127) were randomized to treatment (Figure 1). Of the 245 (donepezil, 121; placebo, 124) patients who received treatment, 98 (81.0%) donepezil- and 97 (78.2%) placebo-treated patients completed the study.
The primary efficacy variable was analyzed for 111 donepezil- and 115 placebo-treated patients. Protocol violation was recorded for one (0.8%; failed to meet inclusion criteria) patient in the donepezil group and five (4.0%; prohibited medication or comedication) patients in the placebo group.
Patient Characteristics at Baseline
The study drug exposure profile of the safety sample was similar for the donepezil and placebo groups. The mean duration of treatment was 73.7 day (range: 1–94 day) for donepezil (n=121) and 74.0 day (1–92 day) for placebo (n=124). The mean average daily dose of donepezil was 6.9 mg/day (3.8–8.2 mg/day) and of placebo was 9.1 mg/day (3.3–10.1 mg/day); the mean maximum daily doses of donepezil and placebo were 9.6 mg/day (range: 5–20 mg/day) and 9.8 mg/day (range: 5–20 mg/day), respectively. The overall compliance rate was 97.8% for donepezil and 97.4% for placebo.
The treatment groups were similar with regard to demographic characteristics of the safety sample at baseline (Table 1). Approximately 70% of patients in each group were men. The mean age of patients was approximately 40 years, and there were no patients aged ⩽18 or ⩾56 years in either treatment group.
71.1% of donepezil- and 76.6% of placebo-treated patients had a primary diagnosis of schizophrenia (the remaining patients were diagnosed with schizoaffective disorder). The duration of illness since first diagnosis was similar for both treatment groups.
CATIE neurocognitive composite, CGI-S, BACS, WRAT-R, and PANSS total scores at baseline were similar for both treatment groups (Table 1). Significant differences between treatment groups in the PPFS and RFS scores were observed at baseline (PPFS, p=0.0292; RFS, p=0.0178), indicating greater role function and less perception of functional deficit among placebo-treated patients. The overall sample performed slightly (between 0.1 and 0.4 SD) better than the CATIE sample (Keefe et al, 2006) on all tests.
For the safety sample, the most commonly used prior medications were antidepressants (donepezil, 40.5%; placebo, 39.5%), antiepileptics (20.7 vs 20.2%), and drugs used in rheumatic diseases and gout (17.4 vs 19.4%). The medication used earlier was similar for the donepezil and placebo groups, with the exception of analgesics (6.6 vs 12.9%), diabetic drugs (5.0 vs 10.5%), gastrointestinal ulcer healing drugs (7.4 vs 17.7%), and vitamins (8.3 vs 14.5%).
Efficacy
All results shown are derived from the ITT sample. Data analyses for the fully evaluable sample generated similar trends and are not presented.
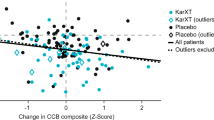
In the primary efficacy analysis, both groups of patients showed significant improvements in the CATIE composite score from baseline to week 12 (Figure 2 and Table 2). For the LOCF analysis, there was no significant difference between the treatment groups. For the OC analysis, the effect-size improvement was significantly different between the treatment groups (p=0.044), indicating greater improvement in cognitive function among placebo-treated patients. This difference remained significant when PPFS and RFS were included as covariates in the primary analysis.
The CATIE neurocognitive measures of letter fluency (COWAT) and semantic fluency (category instances) each showed a significant between-group difference at week 12 LOCF that indicated greater improvement in cognition with placebo treatment (Table 2). No significant treatment difference was observed for any of the other component measures.
There was no statistically significant difference between the treatment groups in PANSS total score LS mean change from baseline at any of the time points measured or at week 12 LOCF (Figure 3). For the PANSS positive symptom subscale, baseline least squares (LS) mean (±SE) was similar for donepezil (13.5±0.34) and placebo (13.4±0.33); LS mean change from baseline was similar for both treatments at all time points except for a treatment difference that favored donepezil at week 6 (donepezil, −0.8±0.26; placebo, 0.1±0.26; p=0.0137). Similarly, for the PANSS negative symptom subscale, LS mean values were similar at baseline for donepezil (16.5±0.41) and placebo (16.3±0.41); a treatment difference that favored placebo was observed at weeks 6 (donepezil, −0.0±0.31; placebo, −0.9±0.31; p=0.033) and 12 (0.3±0.36 vs −1.1±0.36; p=0.0050) and at week 12 LOCF (0.4±0.34 vs −0.8±0.34; p=0.0143).
A significant treatment difference on the CGI-I scale in favor of donepezil was observed at week 6 (LS mean: donepezil, 3.5; placebo, 3.7; p=0.0157). No significant treatment difference was observed at week 12 LOCF (donepezil, 3.6; placebo, 3.8) or at any other time point. Treatments were comparable at all time points for all of the remaining secondary efficacy measures, including the RFS, MADRS, AIMS, SAS, BAS, and PPFS.
Post hoc secondary analyses evaluated the efficacy of treatments according to patient subgroups based on smoking status, antipsychotic drug use, and baseline cognitive function (CATIE composite score). No significant treatment effect was observed for the CATIE neurocognitive battery composite score for subgroups of patients who were smokers or were ex-smokers/had never smoked. When patients were categorized according to the antipsychotic drug that they received during the study, no significant treatment effect was observed using the same efficacy measurement. A subanalysis that included the upper quartile of cognitively impaired patients (ie those most cognitively intact) revealed statistically significantly greater improvement in the placebo group, in keeping with the primary analysis. For patients in the >50 to ⩽75 percentile group, there was a trend towards greater improvement with donepezil.
An additional secondary analysis evaluated the correlation between improvement in CATIE composite score and improvement in PANSS negative symptom scale. For treatments combined, the Pearson correlation coefficients were −0.0539 at week 6 and −0.1171 at week 12, indicating no significant correlation between the two measures. No significant correlation was observed for either study treatment group.
Safety and Tolerability
The pattern of concomitant medication use during the study period was similar for patients in the donepezil and placebo groups. Eight donepezil- and six placebo-treated patients received an antimanic drug in addition to the antipsychotic study drug. The most commonly used concomitant medications were antidepressant drugs (approximately 40% of patients), antiepileptics (20%), and drugs used in rheumatic diseases and gout (17–19%).
The overall occurrence and incidence of treatment-emergent AEs in the safety population were similar between the donepezil group (54.5%) and the placebo group (61.3%; Table 3). Most AEs were rated as mild to moderate in severity; the frequency of severe AEs and the frequency of serious AEs (SAEs) were similar for both treatment groups. Treatment groups were also similar with regard to the frequency of dose reduction or temporary study drug discontinuation due to AEs (donepezil, three (2.5%) patients; placebo, two (1.6%) patients), and the frequency of AE-related withdrawal from the study (donepezil, 10 (8.3%); placebo, 13 (10.5%)). No patient died during the study period.
The most frequently reported AEs were headache and those affecting the digestive system and nervous system, the majority of which were rated as mild to moderate in nature (Table 3). The treatment groups were comparable with regard to changes in vital signs throughout the study. In general, systolic and diastolic blood pressure, heart rate, and weight remained stable and were similar for both groups from baseline to week 12.
Physical examination results were similar for both treatment groups from baseline to week 12. There was no consistent or notable trend in any ECG parameter in either group. No ECG abnormality was reported as an SAE and none led to discontinuation of a patient from the study.
Clinically significant laboratory abnormalities were generally isolated, with the exception of elevations in creatine kinase (Meltzer, 1976; Terao et al, 1999) and glucose (Gury, 2004), which were to be expected in this population. Creatine kinase abnormalities were seen in eight (7.1%) donepezil- and seven (6.3%) placebo-treated patients, and glucose abnormalities in four (3.5%) donepezil- and nine (7.9%) placebo-treated patients. No laboratory abnormality was reported as an SAE and none led to discontinuation of a patient from the study.
DISCUSSION
This large-scale, placebo-controlled, double-blind study investigated the efficacy and tolerability of donepezil as adjunctive therapy for cognitive impairment in patients with stable schizophrenia or schizoaffective disorder. The study indicated that donepezil was safe and well tolerated, but was not effective compared with placebo as a cotreatment for the improvement of cognitive impairment in patients stabilized on selected second-generation antipsychotics.
The baseline values of CATIE composite score were consistent with the exclusion of severely cognitively impaired patients. Likewise, the baseline values of PANSS total score and the modest improvements seen in the total, positive, and negative symptom subscale scores are consistent with the enrollment of patients stabilized on antipsychotic therapy and in the residual phase of illness.
The primary efficacy data indicated that patients in both treatment groups initiated treatment with similar levels of cognitive impairment and experienced mild cognitive test performance improvement. The effect sizes of cognitive improvement (0.45 for placebo; 0.26 for donepezil) were between small and medium, close to what would be considered clinically significant. The placebo group showed statistically significantly greater improvement than the donepezil group at week 12 OC and a trend towards greater improvement at week 12 LOCF. In the context of a double-blind study design, the degree of cognitive enhancement observed for each treatment group is a function of three variables: treatment effect, placebo effect, and practice effect. These data might suggest a substantial placebo effect and/or practice effect within the placebo group that might also be expected to factor in the response within the donepezil group. That a treatment difference in favor of placebo was observed suggests that either a lesser practice effect occurred within the donepezil group or that donepezil had a negative effect on cognitive improvement in this study population.
The magnitude of the response observed for the placebo group in this study (0.45 z-score change at week 12), approaching a ‘medium’ effect (Cohen, 1977) was surprising. Previous work on patients tested twice within a briefer period than the test-retest interval in this study suggests that schizophrenia patients demonstrate relatively small improvements in executive functions (Keefe et al, 2004; Nuechterlein et al, 2007), the WAIS digit-symbol test (Nuechterlein et al, 2007), and medium improvements on tests of verbal memory only when identical versions are repeated (Hawkins and Wexler, 1999; Keefe et al, 2004) but not on tests of verbal fluency (Keefe et al, 2004; Nuechterlein et al, 2007). In this study, patients who received placebo improved substantially across many domains. This surprising result suggests that, possibly due to expectation bias in patients and/or testers, the magnitude of placebo effects in cognitive enhancement trials may exceed the reported size of practice-related improvements in studies of schizophrenia patients tested twice without the prospect of the initiation of a cognitive intervention. Another factor that might have contributed to the magnitude of the placebo effect is the inclusion of patients who were required, based on several criteria, to be clinically stable upon inclusion and to remain clinically stable throughout the study, with only minor antipsychotic dosage adjustments permitted. In fact, few patients experienced a psychiatric relapse during the course of this study and PANSS scores remained stable throughout. Thus, patients in this study were closely monitored with respect to their clinical status, which may have resulted in greater compliance with their antipsychotic regimen and possibly exerted a beneficial effect on cognition.
Both treatment groups showed improvement in cognition and improvement in positive and negative symptoms. Surprisingly, patients who received placebo experienced significantly greater improvement in negative symptoms. This might suggest that, despite the randomization inherent in the study design, the placebo group included an overrepresentation of patients who were liable to improve clinically and cognitively during the study period. Yet the fact that the treatment groups exhibited many similarities at baseline in demographics, clinical characteristics, and neurocognitive functioning argues against this. Furthermore, a post hoc analysis revealed no significant correlation between improvement in cognition and improvement in negative symptoms. In the context of a double-blind study design, this observation suggests that the response within the placebo group cannot be explained by overrepresentation of clinically responsive patients.
It is noteworthy that placebo-treated patients scored significantly better than donepezil-treated patients on the PPFS and RFS at baseline, indicating greater role function and less perception of functional deficit among placebo-treated patients. It is possible that the expectation of potential cognitive improvement upon study treatment enabled modest improvements on effort-related tests such as verbal fluency. However, when the primary efficacy analysis was re-run to include PPFS and RFS as co-variates, the statistically significant difference in cognitive improvement in favor of placebo remained, suggesting that these features cannot explain the response within the placebo group.
It seems likely, therefore, that we observed a greater practice effect within the placebo group compared to the practice effect seen in the donepezil group. Since the placebo group trended towards greater improvement on the cognitive end point, it is possible that donepezil treatment might have exerted a negative influence on cognition, as seen in diminished practice-induced learning relative to the placebo group. This speculation is based on the assumption that, in the context of a double-blind study with repeated task exposure, we would expect the same practice-induced learning effect to be equally present among both placebo- and donepezil-treated patients. It is noteworthy that a diminished practice effect may also be found in patients switching from moderate doses to low doses of haloperidol or fluphenazine compared to those switching to risperidone (Harvey et al, 2000). The present study did not employ any a priori methodological strategies to reduce the magnitude of potential practice effects, such as the use of a placebo run-in period with one or more administrations of the CATIE battery before randomization. Based on the present findings, this and other techniques should be considered in future cognitive enhancement studies in schizophrenia to reduce the magnitude of practice effects.
It is noteworthy that patients in the donepezil group received a dose of 5 mg/day up to week 6 and 10 mg/day thereafter. According to LS mean change values of the CATIE total score, cognitive improvement with donepezil was equivalent to that with placebo at week 6, but essentially remained flat in the donepezil group beyond week 6, while the placebo group continued to demonstrate improvement to week 12. Whereas the study was not designed to assess the association between donepezil dose and cognitive improvement, it is possible that the escalation to the 10 mg dose may have exerted a deleterious effect on cognition in these patients.
It is not completely clear why donepezil delays cognitive decline in patients with AD, but does not improve cognition schizophrenia. It is certainly possible that the benefit of ChEIs in AD is related to the various abnormalities of the cholinergic system found in AD but not in schizophrenia, and that procholinergic treatment will not be effective in schizophrenia. The dosing regimen chosen for this study may also be a factor in explaining the results. The donepezil dosing strategy employed in this study design was based on previous studies in AD patients, which demonstrated cognitive improvements with both 5 and 10 mg/day dosing (Rogers et al, 1998a, 1998b; Winblad et al, 2001; Pratt et al, 2002). Dose escalation from 5 to 10 mg/day at 4–6 weeks was included in the study design as it has been linked to a reduced incidence of cholinergic AEs in AD populations. It is possible that the dose–cognitive response curve for donepezil differs between patients with AD and those with schizophrenia. It is conceivable that donepezil achieves higher concentrations within the cholinergic systems of schizophrenic patients than within the same systems of AD patients. While studies in schizophrenic patients have overall suggested that increased cholinergic activity is associated with cognitive benefits, some studies have demonstrated a relationship between decreased acetycholinesterase activity and increased cognitive impairment (Stip et al, 2005).
It is also worth noting that the study enrolled a group of schizophrenic patients who were chronically and moderately ill, and similar to the CATIE sample on all cognitive tests. While data were not collected on previous treatment history, it is likely given the age of the patients and duration of illness that they had previous exposure to conventional antipsychotics and anticholinergic medication and this may have influenced patients' potential to respond to treatment with a pro-cholinergic agent. It is possible that donepezil and placebo might achieve different effects on cognition in patients who have only recently begun to experience cognitive dysfunction.
In this population of stable schizophrenia/schizoaffective patients maintained on selected second-generation antipsychotics, donepezil appeared to be as safe and as well-tolerated as placebo, in agreement with a previous double-blind, placebo-controlled study in schizophrenic patients (Freudenreich et al, 2005) and studies in AD patients (Pratt et al, 2002). In particular, the rate of anticipated cholinomimetic AEs, such as diarrhea and nausea, was less frequent than observed in studies with patients who received donepezil 10 mg/day for the treatment of AD dementia.
The FDA-NIMH-MATRICS guidelines have suggested that certain study design features may help to detect changes in cognitive impairment by isolating neurocognitive improvement from other clinical changes (Buchanan et al, 2005). These suggestions include a randomized, double-blind design, a sufficiently large sample to detect changes in cognition, use of a comprehensive neurocognitive battery and a placebo comparator arm, and the restriction of enrollment to patients who are clinically and pharmacologically stable, with no more than moderately severe symptoms. Although this study was designed and initiated before the MATRICS guidelines and MATRICS Consensus Battery were established, the present study is consistent with these suggestions and represents a rigorous study of donepezil adjunctive therapy in a sample size of schizophrenic patients that is far larger than any study conducted to date.
The results of this study reinforce the findings of some of the previously reported double-blind, placebo-controlled trials in smaller samples, which suggested that adjunctive donepezil therapy does not significantly improve cognitive impairment in moderately ill patients with schizophrenia or schizoaffective disorder maintained on antipsychotic medication (Freudenreich et al, 2005; Friedman et al, 2002; Tugal et al, 2004; Fagerlund et al, 2007). Whether this conclusion applies to other AChEIs remains to be demonstrated. Small-scale studies with rivastigmine have demonstrated either some (Lenzi et al, 2003; Mendelsohn et al, 2004) or no improvement (Aasen et al, 2005; Kumari et al, 2006) in cognitive function among schizophrenia patients, whereas two case reports have recorded improved cognition with galantamine adjuvant therapy (Bennouna et al, 2005; Bora et al, 2005). Recent work with α-7 nicotinic agonists suggest that this mechanism may be more promising in improving cognition in patients with schizophrenia (Olincy et al, 2006), which is supported clinically by the large percentage of patients with schizophrenia who smoke cigarettes (Hughes et al, 1986; Kelly and McCreadie, 1999). These and various other strategies are currently underway to determine the best pharmacologic mechanisms for improving cognition in schizophrenia (Geyer and Tamminga, 2004).
References
Aasen I, Kumari V, Sharma T (2005). Effects of rivastigmine on sustained attention in schizophrenia: an FMRI study. J Clin Psychopharmacol 25: 311–317.
American Psychiatric Association (1994). Schizophrenia and other psychotic disorders. In: American Psychiatric Association (ed). Diagnostic and Statistical Manual of Mental Disorders, 4th edn. American Psychiatric Association: Washington, DC. pp 273–315.
Barnes TR (1989). A rating scale for drug-induced akathisia. Br J Psychiatry 154: 672–676.
Bennouna M, Greene VB, Defranoux L (2005). Adjuvant galantamine to risperidone improves negative and cognitive symptoms in a patient presenting with schizophrenialike psychosis after traumatic brain injury. J Clin Psychopharmacol 25: 505–507.
Benton AL, Hamsher KD (1989). Multilingual Aphasia Examination. AJA Associates: Iowa City (IA), USA.
Bilder RM, Goldman RS, Robinson D, Reiter G, Bell L, Bates JA et al (2000). Neuropsychology of first-episode schizophrenia: initial characterization and clinical correlates. Am J Psychiatry 157: 549–559.
Bora E, Veznedaroglu B, Kayahan B (2005). The effect of galantamine added to clozapine on cognition of five patients with schizophrenia. Clin Neuropharmacol 28: 139–141.
Brandt J (1991). The Hopkins verbal learning test: development of a new verbal memory test with six equivalent forms. Clin Neuropsychol 5: 125–142.
Breese CR, Lee MJ, Adams CE, Sullivan B, Logel J, Gillen KM et al (2000). Abnormal regulation of high affinity nicotinic receptors in subjects with schizophrenia. Neuropsychopharmacology 23: 351–364.
Buchanan RW, Davis M, Goff D, Green MF, Keefe RS, Leon AC et al (2005). A summary of the FDA-NIMH-MATRICS workshop on clinical trial design for neurocognitive drugs for schizophrenia. Schizophr Bull 31: 5–19.
Buchanan RW, Summerfelt A, Tek C, Gold J (2003). An open-labeled trial of adjunctive donepezil for cognitive impairments in patients with schizophrenia. Schizophr Res 59: 29–33.
Burns A, Rossor M, Hecker J, Gauthier S, Petit H, Moller HJ et al (1999). The effects of donepezil in Alzheimer's disease—results from a multinational trial. Dement Geriatr Cogn Disord 10: 237–244.
Cohen J (1977). Statistical Power Analysis for the Behavioral Sciences. Academic Press: New York.
Cornblatt BA, Obuchowski M, Schnur DB, O'Brien JD (1997). Attention and clinical symptoms in schizophrenia. Psychiatr Q 68: 343–359.
Cornblatt BA, Risch NJ, Faris G, Friedman D, Erlenmeyer-Kimling L (1988). The continuous performance test, identical pairs version (CPT-IP): I. New findings about sustained attention in normal families. Psychiatry Res 26: 223–238.
Crook JM, Tomaskovic-Crook E, Copolov DL, Dean B (2000). Decreased muscarinic receptor binding in subjects with schizophrenia: a study of the human hippocampal formation. Biol Psychiatry 48: 381–388.
Crook JM, Tomaskovic-Crook E, Copolov DL, Dean B (2001). Low muscarinic receptor binding in prefrontal cortex from subjects with schizophrenia: a study of Brodmann's areas 8, 9, 10, and 46 and the effects of neuroleptic drug treatment. Am J Psychiatry 158: 918–925.
Department of Health and Human Services (1993). COSTART: Coding Symbols for Thesaurus of Adverse Reaction Terms. FDA: Rockville, MD, USA.
Fagerlund B, Soholm B, Fink-Jensen A, Lublin H, Glenthoj BY (2007). Effects of Donepezil adjunctive treatment to Ziprasidone on cognitive deficits in schizophrenia: a double-blind, Placebo-Controlled Study. Clin Neuropharmacol 30: 3–12.
Freedman R, Hall M, Adler LE, Leonard S (1995). Evidence in postmortem brain tissue for decreased numbers of hippocampal nicotinic receptors in schizophrenia. Biol Psychiatry 38: 22–33.
Freudenreich O, Herz L, Deckersbach T, Evins AE, Henderson DC, Cather C et al (2005). Added donepezil for stable schizophrenia: a double-blind, placebo-controlled trial. Psychopharmacology (Berl) 181: 358–363.
Friedman JI (2004). Cholinergic targets for cognitive enhancement in schizophrenia: focus on cholinesterase inhibitors and muscarinic agonists. Psychopharmacology (Berl) 174: 45–53.
Friedman JI, Adler DN, Howanitz E, Harvey PD, Brenner G, Temporini H et al (2002). A double blind placebo controlled trial of donepezil adjunctive treatment to risperidone for the cognitive impairment of schizophrenia. Biol Psychiatry 51: 349–357.
Fuller R, Nopoulos P, Arndt S, O'Leary D, Ho BC, Andreasen NC (2002). Longitudinal assessment of premorbid cognitive functioning in patients with schizophrenia through examination of standardized scholastic test performance. Am J Psychiatry 159: 1183–1189.
Geyer MA, Tamminga CA (2004). Measurement and treatment research to improve cognition in schizophrenia: neuropharmacological aspects. Psychopharmacology (Berl) 174: 1–2.
Gold JM, Carpenter C, Randolph C, Goldberg TE, Weinberger DR (1997). Auditory working memory and Wisconsin card sorting test performance in schizophrenia. Arch Gen Psychiatry 54: 159–165.
Green MF (1996). What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry 153: 321–330.
Green MF, Braff DL (2001). Translating the basic and clinical cognitive neuroscience of schizophrenia to drug development and clinical trials of antipsychotic medications. Biol Psychiatry 49: 374–384.
Green MF, Kern RS, Heaton RK (2004). Longitudinal studies of cognition and functional outcome in schizophrenia: implications for MATRICS. Schizophr Res 72: 41–51.
Guan ZZ, Zhang X, Blennow K, Nordberg A (1999). Decreased protein level of nicotinic receptor alpha7 subunit in the frontal cortex from schizophrenic brain. Neuroreport 10: 1779–1782.
Gury C (2004). Schizophrenia, diabetes mellitus and antipsychotics. Encephale 30: 382–391.
Harvey PD, Keefe RS (2001). Studies of cognitive change in patients with schizophrenia following novel antipsychotic treatment. Am J Psychiatry 158: 176–184.
Harvey PD, Moriarty PJ, Serper MR, Schnur E, Lieber D (2000). Practice-related improvement in information processing with novel antipsychotic treatment. Schizophr Res 46: 139–148.
Hawkins KA, Addington J, Keefe RS, Christensen B, Perkins DO, Zipurksy R et al (2004). Neuropsychological status of subjects at high risk for a first episode of psychosis. Schizophr Res 67: 115–122.
Hawkins KA, Wexler BE (1999). California verbal learning test practice effects in a schizophrenia sample. Schizophr Res 39: 73–78.
Heaton RK, Chelune GJ, Talley JL, Kay GG, Curtiss G (1993). The Wisconsin Card Sorting Test Manual-Revised and Expanded. Psychological Assessment Resources Inc.: Lutz, FL.
Heinrichs RW, Zakzanis KK (1998). Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology 12: 426–445.
Hershey T, Craft S, Glauser TA, Hale S (1998). Short-term and long-term memory in early temporal lobe dysfunction. Neuropsychology 12: 52–64.
Hughes JR, Hatsukami DK, Mitchell JE, Dahlgren LA (1986). Prevalence of smoking among psychiatric outpatients. Am J Psychiatry 143: 993–997.
Kay SR, Fiszbein A, Opler LA (1987). The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13: 261–276.
Keefe RS, Bilder RM, Davis SM, Harvey PD, Palmer BW, Gold JM et al (2007). Neurocognitive effects of antipsychotic medications in patients with chornic schizophrenia in the CATIE trial. Arch Gen Psychiatry 64: 633–647.
Keefe RS, Bilder RM, Harvey PD, Davis SM, Palmer BW, Gold JM et al (2006). Baseline neurocognitive deficits in the CATIE schizophrenia trial. Neuropsychopharmacology 31: 2033–2046.
Keefe RS, Goldberg TE, Harvey PD, Gold JM, Poe MP, Coughenour L (2004). The brief assessment of cognition in schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res 68: 283–297.
Keefe RS, Mohs RC, Bilder RM, Harvey PD, Green MF, Meltzer HY et al (2003). Neurocognitive assessment in the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) project schizophrenia trial: development, methodology, and rationale. Schizophr Bull 29: 45–55.
Keefe RS, Silva SG, Perkins DO, Lieberman JA (1999). The effects of atypical antipsychotic drugs on neurocognitive impairment in schizophrenia: a review and meta-analysis. Schizophr Bull 25: 201–222.
Kelly C, McCreadie RG (1999). Smoking habits, current symptoms, and premorbid characteristics of schizophrenic patients in Nithsdale, Scotland. Am J Psychiatry 156: 1751–1757.
Kumari V, Aasen I, Ffytche D, Williams SC, Sharma T (2006). Neural correlates of adjunctive rivastigmine treatment to antipsychotics in schizophrenia: a randomized, placebo-controlled, double-blind fMRI study. Neuroimage 29: 545–556.
Lenzi A, Maltinti E, Poggi E, Fabrizio L, Coli E (2003). Effects of rivastigmine on cognitive function and quality of life in patients with schizophrenia. Clin Neuropharmacol 26: 317–321.
MacEwan GW, Ehmann TS, Khanbhai I, Wrixon C (2001). Donepezil in schizophrenia—is it helpful? An experimental design case study. Acta Psychiatr Scand 104: 469–472.
Mandel RJ, Gage FH, Thal LJ (1989). Enhanced detection of nucleus basalis magnocellularis lesion-induced spatial learning deficit in rats by modification of training regimen. Behav Brain Res 31: 221–229.
Matthews CG, Klove H (1964). Instruction Manual for the Adult Neuropsychology Test Battery. University of Wisconsin Medical School: Madison (WI), USA.
McPheeters HL (1984). Statewide mental health outcome evaluation: a perspective of two southern states. Community Ment Health J 20: 44–55.
Meltzer HY (1976). Serum creatine phosphokinase in schizophrenia. Am J Psychiatry 133: 192–197.
Mendelsohn E, Rosenthal M, Bohiri Y, Werber E, Kotler M, Strous RD (2004). Rivastigmine augmentation in the management of chronic schizophrenia with comorbid dementia: an open-label study investigating effects on cognition, behaviour and activities of daily living. Int Clin Psychopharmacol 19: 319–324.
Montgomery SA, Asberg M (1979). A new depression scale designed to be sensitive to change. Br J Psychiatry 134: 382–389.
Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch D, Cohen J et al (2007). The MATRICS consensus cognitive battery: part 1. Test selection, reliability, and validity. Am J Psychiatry (in press).
Olincy A, Harris JG, Johnson LL, Pender V, Kongs S, Allensworth D et al (2006). Proof-of-concept trial of an alpha7 nicotinic agonist in schizophrenia. Arch Gen Psychiatry 63: 630–638.
Powchik P, Davidson M, Haroutunian V, Gabriel SM, Purohit DP, Perl DP et al (1998). Postmortem studies in schizophrenia. Schizophr Bull 24: 325–341.
Pratt RD, Perdomo CA, Surick IW, Ieni JR (2002). Donepezil: tolerability and safety in Alzheimer's disease. Int J Clin Pract 56: 710–717.
Raedler TJ, Knable MB, Jones DW, Urbina RA, Gorey JG, Lee KS et al (2003). In vivo determination of muscarinic acetylcholine receptor availability in schizophrenia. Am J Psychiatry 160: 118–127.
Risch SC, McGurk S, Horner MD, Nahas Z, Owens SD, Molloy M et al (2001). A double-blind placebo-controlled case study of the use of donepezil to improve cognition in a schizoaffective disorder patient: functional MRI correlates. Neurocase 7: 105–110.
Rogers SL, Doody RS, Mohs RC, Friedhoff LT (1998a). Donepezil improves cognition and global function in Alzheimer disease: a 15-week, double-blind, placebo-controlled study. Donepezil Study Group. Arch Intern Med 158: 1021–1031.
Rogers SL, Farlow MR, Doody RS, Mohs R, Friedhoff LT (1998b). A 24-week, double-blind, placebo-controlled trial of donepezil in patients with Alzheimer's disease. Donepezil Study Group. Neurology 50: 136–145.
Saykin AJ, Shtasel DL, Gur RE, Kester DB, Mozley LH, Stafiniak P et al (1994). Neuropsychological deficits in neuroleptic naive patients with first-episode schizophrenia. Arch Gen Psychiatry 51: 124–131.
Simpson GM, Angus JW (1970). A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl 212: 11–19.
Sitaram N, Weingartner H, Gillin JC (1978). Human serial learning: enhancement with arecholine and choline impairment with scopolamine. Science 201: 274–276.
Stip E, Chouinard S, Boulay LJ (2005). On the trail of a cognitive enhancer for the treatment of schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 29: 219–232.
Terao T, Matsuda S, Kojima H, Okuno K, Hori H, Kaku A et al (1999). Incidence and risk factors of benign creatine phosphokinase elevations in chronic psychiatric patients. Neuropsychobiology 39: 173–180.
Tugal O, Yazici KM, Anil Yagcioglu AE, Gogus A (2004). A double-blind, placebo controlled, cross-over trial of adjunctive donepezil for cognitive impairment in schizophrenia. Int J Neuropsychopharmacol 7: 117–123.
US Dept of Health EaW (1976a). CGI: Clinical Global Impressions. ECDEU Assessment Manual for Psychopharmacology. US Dept of Health, Education, and Welfare publication ADM 76-338: Rockville, MD.
US Dept of Health EaW (1976b). The Abnormal Involuntary Movement Scale. US Dept of Health, Education, and Welfare publication ADM 76-338: Rockville, MD.
Wechsler D (1981). Wechsler Adult Intelligence Scale-Revised. Psychological Corporation: New York, NY, USA.
Wechsler D (1991). Wechsler Intelligence Scale for Children. The Psychological Corporation: San Antonio, TX.
Whitehead A, Perdomo C, Pratt RD, Birks J, Wilcock GK, Evans JG (2004). Donepezil for the symptomatic treatment of patients with mild to moderate Alzheimer's disease: a meta-analysis of individual patient data from randomised controlled trials. Int J Geriatr Psychiatry 19: 624–633.
Winblad B, Engedal K, Soininen H, Verhey F, Waldemar G, Wimo A et al (2001). A 1-year, randomized, placebo-controlled study of donepezil in patients with mild to moderate AD. Neurology 57: 489–495.
Winkler J, Suhr ST, Gage FH, Thal LJ, Fisher LJ (1995). Essential role of neocortical acetylcholine in spatial memory. Nature 375: 484–487.
Woodward ND, Purdon SE, Meltzer HY, Zald DH (2005). A meta-analysis of neuropsychological change to clozapine, olanzapine, quetiapine, and risperidone in schizophrenia. Int J Neuropsychopharmacol 8: 457–472.
World Medical Association declaration of Helsinki (1997). Recommendations guiding physicians in biomedical research involving human subjects. JAMA 277: 925–926.
Acknowledgements
This study was supported by Eisai Inc. and Pfizer Inc. Editorial support was provided by Lisa Thomas at PAREXEL and was funded by Eisai Inc. and Pfizer Inc.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure/Conflict of Interest
Richard Keefe has received grant/research support from Astra-Zeneca, Eli Lilly, Johnson & Johnson, Pfizer, and NIMH, as well as providing educational services to Astra-Zeneca, Eli Lilly, Forest Labs, GlaxoSmithKline, Johnson & Johnson, Pfizer, and Repligen. He has also served as a consultant and on advisory boards for various pharmaceutical companies as follows: Abbott Pharmaceuticals (advisory board), Astra-Zeneca (advisory board, consultant), Bristol Myers Squibb (advisory board), Dainippon Sumitomo Pharma. (consultant), Eli Lilly (advisory board, consultant), Forest Labs (consultant), GlaxoSmithKline (consultant), Johnson & Johnson (advisory board, consultant), Lundbeck/Solvay/Wyeth (advisory board), Memory Pharmaceuticals (advisory board), Merck (advisory board, consultant), Orexigen (advisory board, consultant), Otsuka (consultant), Pfizer (advisory board, consultant), Repligen (consultant), Saegis (advisory board, consultant), Sanofi/Aventis (advisory board, consultant), and Xenoport (consultant). In addition, Dr Keefe receives royalties from the Brief Assessment of Cognition testing battery and the MATRICS Battery (BACS Symbol Coding). Anil K Malhotra has received grant/research support, has served as a consultant and on speakers bureau for Pfizer Inc. Herbert Meltzer has served as a consultant for and been awarded grants from ARYx Therapeutics, Bristol Myers Squibb, Eli Lilly and Company, Janssen, Memory, Pfizer Inc., and in addition has also served as a lecturer for Solvay Pharmaceuticals. He has also served as a consultant for CogTest. John M Kane has served as a consultant for Abbott, Astra-Zeneca, Bristol-Myers Squibb, Janssen, Eli Lilly and Company, Pfizer Inc., and Wyeth Pharmaceticals and on Speakers Bureau for Bristol-Myers Squibb, Janssen, and Astra-Zeneca. Robert W Buchanan received no funds for his involvement in the current project. Dr Buchanan has received grant/research support from Ortho-McNeil who supplied study medications for a foundation supported clinical trial of galantamine, an acetylcholinesterase inhibitor and Janssen who supplied study medications for a NIMH-supported clinical trial of risperidone, an antipsychotic used in the treatment of schizophrenia. Dr Buchanan has also served as a consultant and on advisory boards for various pharmaceutical companies as follows: Pfizer (advisory board), Pfizer is a sponsor of the current study; Organon (consultant), Organon is developing drugs for the treatment of schizophrenia; Merck (Advisory Board), Merck is developing a drug for the treatment of schizophrenia; Glaxo-Smith-Kline (consultant), Glaxo-Smith-Kline is developing a drug for the treatment of schizophrenia; Astra-Zeneca (Advisory Board), Astra-Zeneca is developing a drug for the treatment of schizophrenia; Solvay Pharmaceuticals, Inc. (Advisory Board), Solvay is developing a drug for the treatment of schizophrenia; Roche (consultant), Roche is developing a drug for the treatment of schizophrenia. Dr Buchanan works with Pfizer as a DSMB member for two studies of ziprasidone, an antipsychotic used in the treatment of schizophrenia and with Wyeth as a DSMB member for study examining experimental drug for the treatment of schizophrenia. Dr Buchanan has not been involved in Speakers Bureaus and is not a major stock holder. Anita Murthy is an employee of Eisai Inc., and Mindy Sovel, Chunming Li, and Robert Goldman are employees of Pfizer Inc., the Pharmaceutical companies that manufacture and market donepezil.
Rights and permissions
About this article
Cite this article
Keefe, R., Malhotra, A., Meltzer, H. et al. Efficacy and Safety of Donepezil in Patients with Schizophrenia or Schizoaffective Disorder: Significant Placebo/Practice Effects in a 12-Week, Randomized, Double-Blind, Placebo-Controlled Trial. Neuropsychopharmacol 33, 1217–1228 (2008). https://doi.org/10.1038/sj.npp.1301499
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1301499
Keywords
This article is cited by
-
Cross-diagnostic determinants of cognitive functioning: the muscarinic cholinergic receptor as a model system
Translational Psychiatry (2023)
-
Beyond antipsychotics: a twenty-first century update for preclinical development of schizophrenia therapeutics
Translational Psychiatry (2022)
-
An integrative framework for perceptual disturbances in psychosis
Nature Reviews Neuroscience (2019)
-
Efficacy of different types of cognitive enhancers for patients with schizophrenia: a meta-analysis
npj Schizophrenia (2018)
-
Neurocognitive performance, subjective well-being, and psychosocial functioning after benzodiazepine withdrawal in patients with schizophrenia or bipolar disorder: a randomized clinical trial of add-on melatonin versus placebo
European Archives of Psychiatry and Clinical Neuroscience (2017)