Abstract
Pediatric T-cell acute lymphoblastic leukemia (T-ALL) is characterized by chromosomal rearrangements possibly enforcing arrest at specific development stages. We studied the relationship between molecular-cytogenetic abnormalities and T-cell development stage to investigate whether arrest at specific stages can explain the prognostic significance of specific abnormalities. We extensively studied 72 pediatric T-ALL cases for genetic abnormalities and expression of transcription factors, NOTCH1 mutations and expression of specific CD markers. HOX11 cases were CD1 positive consistent with a cortical stage, but as 4/5 cases lacked cytoplasmatic-β expression, developmental arrest may precede β-selection. HOX11L2 was especially confined to immature and pre-AB developmental stages, but 3/17 HOX11L2 mature cases were restricted to the γδ-lineage. TAL1 rearrangements were restricted to the αβ-lineage with most cases being TCR-αβ positive. NOTCH1 mutations were present in all molecular-cytogenetic subgroups without restriction to a specific developmental stage. CALM-AF10 was associated with early relapse. TAL1 or HOX11L2 rearrangements were associated with trends to good and poor outcomes, respectively. Also cases with high vs low TAL1 expression levels demonstrated a trend toward good outcome. Most cases with lower TAL1 levels were HOX11L2 or CALM-AF10 positive. NOTCH1 mutations did not predict for outcome. Classification into T-cell developmental subgroups was not predictive for outcome.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Pui CH, Relling MV, Downing JR . Acute lymphoblastic leukemia. N Engl J Med 2004; 350: 1535–1548.
Thiel E, Kranz BR, Raghavachar A, Bartram CR, Loffler H, Messerer D et al. Prethymic phenotype and genotype of pre-T (CD7+/ER−)-cell leukemia and its clinical significance within adult acute lymphoblastic leukemia. Blood 1989; 73: 1247–1258.
De Keersmaecker K, Marynen P, Cools J . Genetic insights in the pathogenesis of T-cell acute lymphoblastic leukemia. Haematologica 2005; 90: 1116–1127.
Raimondi SC . Current status of cytogenetic research in childhood acute lymphoblastic leukemia. Blood 1993; 81: 2237–2251.
Rubnitz JE, Look AT . Molecular genetics of childhood leukemias. J Pediatr Hematol Oncol 1998; 20: 1–11.
Cauwelier B, Dastugue N, Cools J, Poppe B, Herens C, De Paepe A et al. Molecular cytogenetic study of 126 unselected T-ALL cases reveals high incidence of TCRbeta locus rearrangements and putative new T-cell oncogenes. Leukemia 2006; 20: 1238–1244.
Clappier E, Cuccuini W, Kalota A, Crinquette A, Cayuela JM, Dik WA et al. The C-MYB locus is involved in chromosomal translocation and genomic duplications in human T-cell acute leukemia (T-ALL), the translocation defining a new T-ALL subtype in very young children. Blood 2007; 110: 1251–1261.
Asnafi V, Radford-Weiss I, Dastugue N, Bayle C, Leboeuf D, Charrin C et al. CALM-AF10 is a common fusion transcript in T-ALL and is specific to the TCRgammadelta lineage. Blood 2003; 102: 1000–1006.
Graux C, Cools J, Melotte C, Quentmeier H, Ferrando A, Levine R et al. Fusion of NUP214 to ABL1 on amplified episomes in T-cell acute lymphoblastic leukemia. Nat Genet 2004; 36: 1084–1089.
Lahortiga I, De Keersmaecker K, Van Vlierberghe P, Graux C, Cauwelier B, Lambert F et al. Duplication of the MYB oncogene in T cell acute lymphoblastic leukemia. Nat Genet 2007; 39: 593–595.
Weng AP, Ferrando AA, Lee W, Morris JPt, Silverman LB, Sanchez-Irizarry C et al. Activating mutations of NOTCH1 in human T cell acute lymphoblastic leukemia. Science 2004; 306: 269–271.
van Grotel M, Meijerink JP, Beverloo HB, Langerak AW, Buys-Gladdines JG, Schneider P et al. The outcome of molecular-cytogenetic subgroups in pediatric T-cell acute lymphoblastic leukemia: a retrospective study of patients treated according to DCOG or COALL protocols. Haematologica 2006; 91: 1212–1221.
Ballerini P, Blaise A, Busson-Le Coniat M, Su XY, Zucman-Rossi J, Adam M et al. HOX11L2 expression defines a clinical subtype of pediatric T-ALL associated with poor prognosis. Blood 2002; 100: 991–997.
Cave H, Suciu S, Preudhomme C, Poppe B, Robert A, Uyttebroeck A et al. Clinical significance of HOX11L2 expression linked to t(5;14)(q35;q32), of HOX11 expression, and of SIL-TAL fusion in childhood T-cell malignancies: results of EORTC studies 58881 and 58951. Blood 2004; 103: 442–450.
Ferrando AA, Look AT . Gene expression profiling in T-cell acute lymphoblastic leukemia. Semin Hematol 2003; 40: 274–280.
Gottardo NG, Jacoby PA, Sather HN, Reaman GH, Baker DL, Kees UR . Significance of HOX11L2/TLX3 expression in children with T-cell acute lymphoblastic leukemia treated on children's cancer group protocols. Leukemia 2005; 19: 1705–1708.
Mauvieux L, Leymarie V, Helias C, Perrusson N, Falkenrodt A, Lioure B et al. High incidence of Hox11L2 expression in children with T-ALL. Leukemia 2002; 16: 2417–2422.
Ferrando AA, Neuberg DS, Dodge RK, Paietta E, Larson RA, Wiernik PH et al. Prognostic importance of TLX1 (HOX11) oncogene expression in adults with T-cell acute lymphoblastic leukaemia. Lancet 2004; 363: 535–536.
Kees UR, Heerema NA, Kumar R, Watt PM, Baker DL, La MK et al. Expression of HOX11 in childhood T-lineage acute lymphoblastic leukaemia can occur in the absence of cytogenetic aberration at 10q24: a study from the Children's Cancer Group (CCG). Leukemia 2003; 17: 887–893.
Schneider NR, Carroll AJ, Shuster JJ, Pullen DJ, Link MP, Borowitz MJ et al. New recurring cytogenetic abnormalities and association of blast cell karyotypes with prognosis in childhood T-cell acute lymphoblastic leukemia: a pediatric oncology group report of 343 cases. Blood 2000; 96: 2543–2549.
Breit S, Stanulla M, Flohr T, Schrappe M, Ludwig WD, Tolle G et al. Activating NOTCH1 mutations predict favorable early treatment response and long-term outcome in childhood precursor T-cell lymphoblastic leukemia. Blood 2006; 108: 1151–1157.
Greaves MF . Differentiation-linked leukemogenesis in lymphocytes. Science 1986; 234: 697–704.
Asnafi V, Beldjord K, Libura M, Villarese P, Millien C, Ballerini P et al. Age-related phenotypic and oncogenic differences in T-cell acute lymphoblastic leukemias may reflect thymic atrophy. Blood 2004; 104: 4173–4180.
Breit TM, Mol EJ, Wolvers-Tettero IL, Ludwig WD, van Wering ER, van Dongen JJ . Site-specific deletions involving the tal-1 and sil genes are restricted to cells of the T cell receptor alpha/beta lineage: T cell receptor delta gene deletion mechanism affects multiple genes. J Exp Med 1993; 177: 965–977.
Macintyre EA, Smit L, Ritz J, Kirsch IR, Strominger JL . Disruption of the SCL locus in T-lymphoid malignancies correlates with commitment to the T-cell receptor alpha beta lineage. Blood 1992; 80: 1511–1520.
Bene MC, Castoldi G, Knapp W, Ludwig WD, Matutes E, Orfao A et al. Proposals for the immunological classification of acute leukemias. European Group for the Immunological Characterization of Leukemias (EGIL). Leukemia 1995; 9: 1783–1786.
Crist WM, Shuster JJ, Falletta J, Pullen DJ, Berard CW, Vietti TJ et al. Clinical features and outcome in childhood T-cell leukemia-lymphoma according to stage of thymocyte differentiation: a pediatric oncology group study. Blood 1988; 72: 1891–1897.
Ludwig WD, Harbott J, Bartram CR, Komischke B, Sperling C, Teichmann JV et al. Incidence and prognostic significance of immunophenotypic subgroups in childhood acute lymphoblastic leukemia: experience of the BFM study 86. Recent Results Cancer Res 1993; 131: 269–282.
Garand R, Voisin S, Papin S, Praloran V, Lenormand B, Favre M et al. Characteristics of pro-T ALL subgroups: comparison with late T-ALL. The Groupe d'Etude Immunologique des Leucemies. Leukemia 1993; 7: 161–167.
Vitale A, Guarini A, Ariola C, Mancini M, Mecucci C, Cuneo A et al. Adult T-cell acute lymphoblastic leukemia: biologic profile at presentation and correlation with response to induction treatment in patients enrolled in the GIMEMA LAL 0496 protocol. Blood 2006; 107: 473–479.
Asnafi V, Buzyn A, Thomas X, Huguet F, Vey N, Boiron JM et al. Impact of TCR status and genotype on outcome in adult T-cell acute lymphoblastic leukemia: a LALA-94 study. Blood 2005; 105: 3072–3078.
Niehues T, Kapaun P, Harms DO, Burdach S, Kramm C, Korholz D et al. A classification based on T cell selection-related phenotypes identifies a subgroup of childhood T-ALL with favorable outcome in the COALL studies. Leukemia 1999; 13: 614–617.
Pui CH, Behm FG, Crist WM . Clinical and biologic relevance of immunologic marker studies in childhood acute lymphoblastic leukemia. Blood 1993; 82: 343–362.
Ferrando AA, Neuberg DS, Staunton J, Loh ML, Huard C, Raimondi SC et al. Gene expression signatures define novel oncogenic pathways in T cell acute lymphoblastic leukemia. Cancer Cell 2002; 1: 75–87.
Kamps WA, Bokkerink JP, Hahlen K, Hermans J, Riehm H, Gadner H et al. Intensive treatment of children with acute lymphoblastic leukemia according to ALL-BFM-86 without cranial radiotherapy: results of Dutch childhood leukemia study group protocol ALL-7 (1988–1991). Blood 1999; 94: 1226–1236.
Kamps WA, Bokkerink JP, Hakvoort-Cammel FG, Veerman AJ, Weening RS, van Wering ER et al. BFM-oriented treatment for children with acute lymphoblastic leukemia without cranial irradiation and treatment reduction for standard risk patients: results of DCLSG protocol ALL-8 (1991–1996). Leukemia 2002; 16: 1099–1111.
Stam RW, den Boer ML, Meijerink JP, Ebus ME, Peters GJ, Noordhuis P et al. Differential mRNA expression of Ara-C-metabolizing enzymes explains Ara-C sensitivity in MLL gene-rearranged infant acute lymphoblastic leukemia. Blood 2003; 101: 1270–1276.
Meijerink J, Mandigers C, van de Locht L, Tonnissen E, Goodsaid F, Raemaekers J . A novel method to compensate for different amplification efficiencies between patient DNA samples in quantitative real-time PCR. J Mol Diagn 2001; 3: 55–61.
Gabert J, Beillard E, van der Velden VH, Bi W, Grimwade D, Pallisgaard N et al. Standardization and quality control studies of ‘real-time’ quantitative reverse transcriptase polymerase chain reaction of fusion gene transcripts for residual disease detection in leukemia—a Europe against cancer program. Leukemia 2003; 17: 2318–2357.
Hagemeijer A, Buijs A, Smit E, Janssen B, Creemers GJ, Van der Plas D et al. Translocation of BCR to chromosome 9: a new cytogenetic variant detected by FISH in two Ph-negative, BCR-positive patients with chronic myeloid leukemia. Genes Chromosomes Cancer 1993; 8: 237–245.
van der Burg M, Poulsen TS, Hunger SP, Beverloo HB, Smit EM, Vang-Nielsen K et al. Split-signal FISH for detection of chromosome aberrations in acute lymphoblastic leukemia. Leukemia 2004; 18: 895–908.
van Wering ER, van der Linden-Schrever BE, Szczepanski T, Willemse MJ, Baars EA, van Wijngaarde-Schmitz HM et al. Regenerating normal B-cell precursors during and after treatment of acute lymphoblastic leukaemia: implications for monitoring of minimal residual disease. Br J Haematol 2000; 110: 139–146.
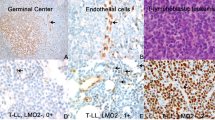
Van Vlierberghe P, van Grotel M, Beverloo HB, Lee C, Helgason T, Buijs-Gladdines J et al. The cryptic chromosomal deletion del(11)(p12p13) as a new activation mechanism of LMO2 in pediatric T-cell acute lymphoblastic leukemia. Blood 2006; 108: 3520–3529.
Ferrando AA, Herblot S, Palomero T, Hansen M, Hoang T, Fox EA et al. Biallelic transcriptional activation of oncogenic transcription factors in T-cell acute lymphoblastic leukemia. Blood 2004; 103: 1909–1911.
Herblot S, Steff AM, Hugo P, Aplan PD, Hoang T . SCL and LMO1 alter thymocyte differentiation: inhibition of E2A-HEB function and pre-T alpha chain expression. Nat Immunol 2000; 1: 138–144.
Grutz GG, Bucher K, Lavenir I, Larson T, Larson R, Rabbitts TH . The oncogenic T cell LIM-protein Lmo2 forms part of a DNA-binding complex specifically in immature T cells. EMBO J 1998; 17: 4594–4605.
Hsu HL, Wadman I, Baer R . Formation of in vivo complexes between the TAL1 and E2A polypeptides of leukemic T cells. Proc Natl Acad Sci USA 1994; 91: 3181–3185.
Wadman IA, Osada H, Grutz GG, Agulnick AD, Westphal H, Forster A et al. The LIM-only protein Lmo2 is a bridging molecule assembling an erythroid, DNA-binding complex which includes the TAL1, E47, GATA-1 and Ldb1/NLI proteins. EMBO J 1997; 16: 3145–3157.
Acknowledgements
This study was sponsored by the Quality of Life and KOCR foundations.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on the Leukemia website (http://www.nature.com/leu)
Supplementary information
Rights and permissions
About this article
Cite this article
van Grotel, M., Meijerink, J., van Wering, E. et al. Prognostic significance of molecular-cytogenetic abnormalities in pediatric T-ALL is not explained by immunophenotypic differences. Leukemia 22, 124–131 (2008). https://doi.org/10.1038/sj.leu.2404957
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2404957
Keywords
This article is cited by
-
CAR-T cell therapy in T-cell malignancies: Is success a low-hanging fruit?
Stem Cell Research & Therapy (2021)
-
Targeted sequencing to identify genetic alterations and prognostic markers in pediatric T-cell acute lymphoblastic leukemia
Scientific Reports (2021)
-
Targeting T cell malignancies using CAR-based immunotherapy: challenges and potential solutions
Journal of Hematology & Oncology (2019)
-
Casein kinase 2 controls the survival of normal thymic and leukemic γδ T cells via promotion of AKT signaling
Leukemia (2017)
-
The effect of TLX3 expression on the prognosis of pediatric T cell acute lymphocytic leukemia—a systematic review
Tumor Biology (2014)