Abstract
Several lines of evidence implicate the Cytotoxic T Lymphocyte Antigen 4 (CTLA4) gene in susceptibility to autoimmune disease. We have examined the association of systemic lupus erythematosus (SLE) with polymorhisms within the CTLA4 gene that were previously proposed to regulate CTLA-4 function: a single nucleotide polymorphism (SNP) in position +49 of exon 1 and a dinucleotide repeat in the 3′ untranslated region (3’UTR). The 3′UTR repeat showed a significant association with SLE, with one allele conferring susceptibility and another conferring protection to the disease. The associated alleles do not support previous suggestions of an allele size-dependent effect of the 3’ UTR polymorphism in autoimmunity development and instead suggest that it is in linkage disequilibrium with a true causative locus. No association of the exon 1 SNP with SLE was found in our population. Given the conflicting results obtained in different studies on the association of SLE with this polymorphism, we performed a meta-analysis including seven previously published studies and the present one. Significantly increased and decreased risks for SLE were found for carriers of the G allele and the A allele, respectively. The functional characterization of disease-associated CTLA4 gene variants is now required to elucidate their role in the pathogenesis of SLE and other autoimmune diseases.
Similar content being viewed by others
Introduction
Systemic lupus erythematosus (SLE) is a complex autoimmune disease of unknown etiology characterized by immunoglobulin G (IgG) autoantibody production against nuclear, cytoplasmic and cell-surface autoantigens.1 Twin and family studies provided evidence for the involvement of genetic factors, showing an increased concordance among monozygotic twins relative to dizygotic twins and a high degree of familial clustering of SLE.2 With the objective of identifying genes involved in SLE, multiple genome-wide scans and candidate gene studies have been performed. However, until now the genetic basis of SLE has not been elucidated, likely reflecting genetic heterogeneity and the complex nature of this disorder.
The gene region 2q33 has been identified as a susceptibility region for SLE in genome-wide scans, and is of particular interest because it harbors the genes encoding the CTLA4 and CD28 cell surface receptors expressed by T cells.3, 4 Inappropriate T-cell-dependent expansion of autoreactive B and T cells is thought to play an important role in SLE pathogenesis. For T-cell activation CD4+ T cells recognize antigen-presenting cells by the antigen bound to MHC class II molecules, but antigen recognition alone is not sufficient and costimulation by other receptor–ligand complexes is required. The main costimulatory molecules involved in this system are the CD28 and CTLA4 receptors and their ligands B7-1 (CD80) and B7-2 (CD86). CD28 is constitutively expressed on T cells and acts as a positive costimulator of T-cell activation. On the other hand, CTLA4 is only expressed on activated cells, and acts as a negative feedback regulator of T-cell activation by inhibiting IL2 transcription and cell cycle progression.5 Furthermore, it has been suggested that CTLA4 may play a role in the control of CD4+CD25+ regulatory T cells, which have been shown to downmodulate immune responses.6, 7
CTLA4 polymorphisms have been found to be associated with several autoimmune disorders, namely type I diabetes, autoimmune thyroid disease, celiac disease, Grave's disease, rheumatoid arthritis and multiple sclerosis.8 A number of studies have tested the association of CTLA4 exon 1 and promoter polymorphic markers with SLE, but report conflicting results.9, 10, 11, 12, 13, 14, 15 With the objective of further investigating the role of CTLA4 in the pathogenesis of SLE, we genotyped two polymorphic markers within the CTLA4 gene for which a genotype-dependent modulation of CTLA4 expression and function have been proposed: a SNP involving an A to G transition at position +49 exon 1 and a microsatelite in the 3′UTR. While the A>G SNP at position +49 in exon 1 leads to a Thr to Ala change in amino-acid 17, leading to a less effective export of CTLA4 to the membrane,16 and an enhanced T-cell proliferative response has been found in healthy donors homozygous for the G allele,17 the length of the 3’UTR dinucleotide repeat has been proposed to influence CTLA4 mRNA stability and turnover.18, 19, 20 Either polymorphism may therefore be of significance for the regulation of immune response and autoimmune pathology.
A case–control association study was conducted to test the involvement of these variants in SLE. While only one previous study tested the association of the 3’UTR marker with SLE, we found seven reports where the role of the exon 1 SNP marker in SLE was assessed, with contradictory results. To draw a firmer conclusion on the involvement of the exon 1 polymorphism in SLE pathogenesis, using the information gathered in the previous studies and our own, we conducted a meta-analysis. This method is frequently used to synthesize inconsistent results obtained in genetic studies of complex disorders, since it is likely that, because multiple genes are involved, the effects of individual loci will be relatively small and may go undetected. The increase in power inherent to the pooling of samples in a meta-analysis allows the combination of weak signals in individual studies into stronger evidence of a genetic effect for a particular trait. Greater accuracy in the estimation of a quantitative risk can therefore be achieved with this method, while taking into account the variability among studies.21
Materials and methods
SLE patients
A total of 125 SLE patients (11 males, 114 females) and 185 healthy controls were recruited from mainland Portugal. Informed consent was obtained from all participants in the study. All patients met the revised 1997 American College of Rheumatology criteria for SLE.22
Samples and genotyping
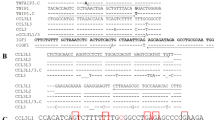
Genomic DNA was isolated from peripheral blood mononuclear cells by standard methods. The CTLA4 +49 exon 1 SNP was genotyped by PCR amplification followed by restriction enzyme analysis. The PCR reaction was performed in a total volume of 25 μl using 25 ng of genomic DNA, 3.0 mM MgCl2 (Promega), 2.5 μl 10 × PCR buffer (Promega), 10 pmol dNTPs (Promega) and 10 pmol of each of the primers (Forward primer: 5′ CTGCTGAAACAAATGAAACCC 3′ and reverse primer: 5′ AAGGCTCAGCTGAACCTGGT 3′). Optimal PCR conditions consisted of an initial 95°C denaturation for 5 min followed by 30 cycles of denaturation at 95°C for 30 s, annealing at 58°C for 30 s and elongation at 72°C for 30 s. The PCR products (152 bp) were subjected to BstEII (Roche) restriction with 1 U of enzyme for 5 h at 60°C in order to identify the base present in the position +49 of CTLA4 exon 1. The DNA fragments obtained were analyzed in a 3% agarose gel. The digested A allele yielded fragments of 130 and a 22 bp but the G allele fragment remained intact. The CTLA4 microsatelite marker on the 3′UTR was genotyped using the Applied Biosystems fluorescence based 377 DNA automated sequencer. The PCR reaction was performed in a total volume of 25 μl using 25 ng of genomic DNA, 3.0 mM MgCl2 (Promega), 2.5 μl 10 × PCR buffer (Promega), 10 pmol dNTPs (Promega), 10 pmol of each primer (labeled forward primer: Hex 5′ GCCAGTGATGCTTAAAGGTTG 3′ and reverse primer: 5′ AACATACGTGGCTCTATGCA 3′). PCR amplification was performed as described before. Semiautomated fragment sizing was performed using GENESCAN® 3.1 software.
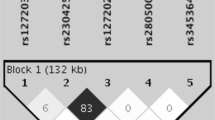
Statistical analysis
Distributions of alleles among patients and controls were assessed by direct counting and compared by χ2 test on contingency tables and odds ratio (OR). Values of P<0.05 were regarded as significant. Meta-analysis was performed according to the Mantel–Haenszel method.23 Haplotypes were estimated by use of the PHASE software.24 Linkage disequilibrium (LD) between the two polymorphic markers was quantified as D' using the HAPLOXT programe implemented in the GOLD software.25
Results
The results obtained in the case–control association study of the CTLA4 3′UTR microsatelite marker with SLE, involving a total of 125 SLE patients and 185 healthy controls, are presented in Table 1. A total of 21 alleles and 46 different genotypes were found for this marker, many of which are very rare. Those with a frequency lower than 1% were grouped for the analysis. A significant overall association of the CTLA4 3′UTR microsatelite marker with SLE was found (χ2=24.190, P=0.001), with a particular allele of 106 bp showing a protective effect (χ2=17.310, P<0.001) and another of 104 bp increasing susceptibility to SLE (χ2=4.636, P=0.031) (Table 1). The OR for each of the alleles confirms the protection conferred by the 106 bp allele (OR=0.28, 95% CI=0.15–0.53). The distribution of genotypes at this marker locus was also significantly different between patients and controls (χ2=21.028, P=0.002). As expected, the heterozygous genotypes 88/104 and 88/106 are, respectively, more frequent among patients (χ2=4.156, P=0.041) and more frequent among healthy individuals (χ2=11.182, P<0.001). The fact that we do not find the homozygous genotypes 104/104 and 106/106 associated with susceptibility or protection to SLE is likely due to a high frequency (approximately 65%) of a specific allele (88 bp) while all the other alleles are relatively rare.
Given that SLE affects primarily women, the male:female ratio is not equal in the case and control samples. Matching for sex did not change the overall association (χ2=21.247, P=0.003) (Table 1). We confirmed the association of the 106 bp protective allele (χ2=12.716, P<0.001; OR=0.27, 95% CI=0.055–0.13) and of the 88/106 genotype (χ2=15.206, P<0.001; OR=0.14, 95% CI=0.050–0.39). In this matched sample, we find that allele 104 and genotype 88/104 are more frequent among patients, although the difference in frequencies among patients and controls is not significant, likely due to loss of power given the much lower number of controls used in this analysis (Table 1).
Allele and genotype distributions of the +49 exon 1 SNP did not differ significantly between patients and healthy control subjects (Table 1), even after matching the population for sex (data not shown). These results corroborate four previous reports of no association of this SNP with SLE,9, 10, 11, 12 although three other studies did find evidence for association.13, 14, 15 Given the conflicting results obtained in these case–control studies that have examined the association between SLE and the CTLA4 exon 1 SNP, and because this polymorphism is thought to regulate the levels of membrane-bound CTLA4, we have performed a meta-analysis to clarify the involvement of this SNP in the etiology of SLE. Results from the seven previous studies and the present one, involving 821 patients and 1329 control subjects, were included in this meta-analysis. We have found evidence for the involvement of CTLA4 exon 1 SNP in the etiology of SLE (Table 2). Under a fixed effects model, which assumes that all studies come from a common population with the same effect size and therefore the only source of between-study variation is random error, the OR for SLE in carriers of the G allele compared with carriers of the A allele was 1.23 (95% CI=1.08–1.41; P=0.002). In the patient population, 75.4% were carriers of this increased susceptibility allele, which is present in 70.2% of healthy controls. The summary OR for the GG genotype was 1.39 (95% CI=1.12–1.71), indicating that GG individuals were at significantly higher risk of developing the disease. Conversely, carriers of the A allele have significantly lower risk of developing disease, while the AA genotype acts as a protective genotype for SLE (Table 2). There is no variation in risk for carriers of the AG genotype, as expected for a heterozygous genotype of alleles with opposite effect in disease susceptibility. The results are corroborated by analysis under the random effects model, which assumes that the populations included in the analysis have different effect sizes due to variation in patient characteristics or methodological issues. Again, carriers of the G allele or GG genotype show increased risk of developing SLE, while carriers of the A allele or AA genotype have a decreased risk (Table 2). The effect found employing this model is slightly less pronounced, reflecting some degree of heterogeneity among studies.
To analyze the distribution of haplotypes of the exon 1 SNP and 3′UTR microsatelite markers in our sample of patients and controls, haplotypes were inferred using the PHASE program24 and are described in Table 3. Using the inferred haplotypes, the two markers were shown to be in LD (D′=0.615, χ2=159.0, P<0.00001). D′ was not significantly different in the patient (D′=0.625) and the control (D′=0.609) populations. The haplotype distribution differed significantly between patients and healthy individuals (χ2=31.290, P=0.008), with haplotype G/104 found more frequently among patients (χ2=4.252, P=0.039, OR=2.70, 95% CI= 1.15–6.53), and haplotype G/106 occurring more frequently in controls (χ2=8.553, P=0.003, OR=0.43, 95% CI=0.25–0.75).
Discussion
Given its role in the activation of T cells and in immune tolerance, CTLA4 has long been implicated in autoimmune disease.26, 27 In this study, we have focused on two polymorphisms within the CTLA4 gene that were hypothesized to influence directly the levels of functional CTLA4 and therefore more likely to play a direct role in immune response modulation defects in autoimmune disorders.
In the present analysis, we obtained suggestive evidence for the involvement of the CTLA4 gene in the pathogenesis of SLE in a Portuguese population. The association found with the microsatelite 3′UTR marker corroborates a previous study in a Japanese population sample,13 and provides further evidence for an association of CTLA4 gene variants in SLE. The location of this polymorphism in the 3′UTR has suggested that it may be important for the control of nuclear export, polyadenylation status, subcellular targeting and rates of translation and degradation of mRNA, by regulating binding of proteins involved in mRNA turnover.18, 19 Lowe et al20 have suggested that the length of the dinucleotide repeat at the CTLA4 3′UTR directly influences CTLA4 expression and function, and provided circumstantial evidence for this hypothesis by showing that the odds of type I diabetes for subjects with longer alleles was higher than for subjects with shorter alleles. The present results, however, do not support a functional role of this polymorphism. Unlike Lowe et al,20 we have not found any correlation between the length of the CTLA4 (AT)n alleles and SLE, and neither have Ahmed et al.13 Furthermore, the 2 bp difference found between the protective allele (106 bp) and the susceptibility allele (104 bp) strongly argues against an allele size-dependent effect of the 3′UTR polymorphism on CTLA4 expression. The 3′UTR alleles found to increase or decrease risk in our population and in the Japanese population are also not the same. Taken together, these observations suggest the occurrence of allelic heterogeneity between populations, indicating that the associated locus is not in itself functionally involved in phenotype determination, but its alleles are in linkage disequilibrium with alleles at a locus in the vicinity that is truly responsible for the pathogenic effect in SLE. The fact that all three studies did find association with this locus, however, strengthens the hypothesis of a true genetic association with a disease susceptibility locus in the vicinity, mediated by different variants in different populations.
We have found no evidence for an association between +49 exon 1 variants and SLE. Because of its possible functional relevance, a number of previous studies have tested this polymorphism for association with several autoimmune disorders and specifically with SLE, with negative9, 10, 11, 12 and positive results.13, 14, 15 Meta-analysis of published studies is a powerful tool to summarize often-conflicting results of separate analysis, estimating an overall effect of a particular locus in the phenotype studied. It is important, however, that the statistical method used allows the pooling of individual statistical estimates while taking into account the sample variability between studies. Using the Mantel–Haenszel method,22 which allows both fixed- and random-effects models of sample heterogeneity, meta-analysis yielded a significant difference in risk between the two exon 1 alleles in SLE patients. The genetic heterogeneity among the populations studied, limited individual study power and other methodological issues likely account for the discrepancies in results among the individual studies, including our own. In fact, although we find that the two polymorphisms are in linkage disequilibrium in our population sample, we could not find an association of exon1 SNP with SLE, possibly due to limitations of the population studied and the lower PIC of the SNP marker.
Ueda et al28 have found a correlation between allelic variation at a polymorphic marker in the 3′ region of CTLA4 and mRNA levels of a soluble CTLA-4 form (sCTLA-4) generated by alternative splicing, in healthy individuals. These authors also report the association of a susceptibility variant to Graves disease with decreased levels of sCTLA-4, and suggest that in this region lies a locus determining the efficiency of splicing and production of sCTLA-4, and autoimmune disease susceptibility. However, the inverse correlation was found in studies of patients with autoimmune thyroid disease and SLE,29, 30 with increased sCTLA protein and mRNA levels associated with these disorders. An hypothesis to explain these conflicting findings is that the soluble form of CTLA-4 may play a dual role in the immune response: it can bind B7 on APCs and prevent B7/CD28-mediated costimulation of T-cell activation but it can also interfere with B7/CTLA-4 interaction and consequently block the negative signal to T cells.29, 30 It is therefore plausible that the effects of CTLA-4 in autoimmunity are mediated not only by the membrane-bound form, but also by an additional mechanism involving the soluble form of CTLA-4, which originates from alternative splicing of the gene. The genotype/phenotype correlations proposed for either mechanism have been established in healthy individuals, and showed that common allelic variants may, in combination with particular genetic and/or environmental factors, become risk factors for complex disorders.28 While our results provide further evidence for the involvement of the CTLA4 gene in the etiology of SLE, in subsequent studies levels of soluble and membrane-bound CTLA4 mRNA expression, and the trafficking of CTLA-4 to the cell surface upon stimulation, must be assessed directly in a population of SLE patients, and correlated with CTLA4 genotypes. We will then be able to further clarify the contribution of either mechanism and the role of CTLA4 genetic variants in SLE susceptibility.
References
Kotzin B : Systemic lupus erythematosus. Cell 1996; 85: 303–306.
Lindqvist AK, Alarcon-Riquelme M : The genetics of systemic lupus erythematosus. Scand J Immunol 1999; 50: 562–571.
Gaffney P, Kearns G, Shark K et al: A genome-wide search for susceptibility genes in systemic lupus erythematosus sib-pair families. Proc Natl Acad Sci USA 1998; 95: 14875–14879.
Moser K, Neas B, Salmon J et al: Genome scan of human systemic lupus erythematosus: evidence for linkage on chromosome 1q in African-American pedigrees. Proc Natl Acad Sci USA 1998; 95: 14869–14874.
Oosterwegel M, Greenwald R, Mandelbrot D, Lorsbach R, Sharpe A : CTLA-4 and T cell activation. Curr Opin Immunol 1999; 11: 294–300.
Read S, Malmstrom V, Powrie F : Cytotoxic T lymphocyte-associated antigen 4 plays an essential role in the function of CD25(+)CD4(+) regulatory cells that control intestinal inflammation. J Exp Med 2000; 192: 295–302.
Takahashi T, Tagami T, Yamazaki S et al: Immunologic self-tolerance maintained by CD25(+)CD4(+) regulatory T cells constitutively expressing cytotoxic T lymphocyte-associated antigen 4. J Exp Med 2000; 192: 303–310.
Kristiansen OP, Larsen ZM, Pociot F : CTLA-4 in autoimmune diseases – a general susceptibility gene to autoimmunity? Genes Immun 2000; 1: 170–184.
Heward J, Gordon C, Allahabadia A, Barnett AH, Franklyn JA, Gough SC : The A–G polymorphism in exon 1 of the CTLA-4 gene is not associated with systemic lupus erythematosus. Ann Rheum Dis 1999; 58: 193–195.
Hudson LL, Rocca K, Song YW, Pandey JP : CTLA-4 gene polymorphisms in systemic lupus erythematosus: a highly significant association with a determinant in the promoter region. Hum Genet 2002; 111: 452–455.
Liu MF, Wang CR, Lin LC, Wu CR : CTLA-4 gene polymorphism in promoter and exon-1 regions in Chinese patients with systemic lupus erythematosus. Lupus 2001; 10: 647–649.
Matsushita M, Tsuchiya N, Shiota M et al: Lack of a strong association of CTLA-4 exon 1 polymorphism with the susceptibility to rheumatoid arthritis and systemic lupus erythematosus in Japanese: an association study using a novel variation screening method. Tissue Antigens 1999; 54: 578–584.
Ahmed S, Ihara K, Kanemitsu S et al: Association of CTLA-4 but not CD28 gene polymorphisms with systemic lupus erythematosus in the Japanese population. Rheumatology (Oxford) 2001; 40: 662–667.
Lee YH, Kim YR, Ji JD, Sohn J, Song GG : Polymorphisms of the CTLA-4 exon 1 and promoter gene in systemic lupus erythematosus. Lupus 2001; 10: 601–605.
Pullmann Jr R, Lukak J, Skerenova M et al: Cytotoxic T lymphocyte antigen 4 (CTLA-4) dimorphism in patients with systemic lupus erythematosus. Clin Exp Rheumatol 1999; 17: 725–729.
Anjos S, Nguyen A, Ounissi-Benkalha H, Tessier MC, Polychronakos C : A common autoimmunity predisposing signal peptide variant of the cytotoxic T-lymphocyte antigen 4. J Biol Chem 2002; 277: 46478–46486.
Mäurer M, Loserth S, Kolb- Mäurer A et al: A polymorphism in the human cytotoxic T-lymphocyte antigen 4 (CTLA4) gene (exon 1 +49) alters T cell activation. Immunogenetics 2002; 54: 1–8.
Conne B, Stutz A, Vassali J : The 3′ untranslated region of messenger RNA: a molecular ‘hotspot’ for pathology? Nat Med 2000; 6: 637–641.
Kuersten S, Goodwin E : The power of the 3′ UTR: translational control and development. Nat Rev Genet 2003; 4: 626–637.
Lowe RM, Graham J, Sund G et al: The length of the CTLA-4 microsatellite (AT)n-repeat affects the risk for type 1 diabetes. Diabetes Incidence in Sweden Study Group. Autoimmunity 2000; 32: 173–180.
Gu C, Province MA, Rao DC : Genetic dissection of complex traits; in Rao DC, Province MA (eds): Advances in genetics. Academic Press: San Diego; 2001, vol 42: pp 255–272.
Hochberg MC : Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 1997; 40: 1725.
Mantel N, Haenszel : Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 1959; 22: 719–748.
Stephens M, Donnely P : A comparison of bayesian methods for haplotype reconstruction from population genotype data. Am J Hum Genet 2003; 73: 1162–1169.
Abecasis GR, Cookson WO : GOLD – graphical overview of linkage disequilibrium. Bioinformatics 2000; 16: 182–183.
Eagar T, Karandikar N, Bluestone J, Miller S : The role of CTLA-4 in induction and maintenance of peripheral T cell tolerance. Eur J Immunol 2002; 32: 972–981.
Perez V, Parijs L, Biuckians A, Zheng X, Strom T, Abbbas A : Induction of peripheral T cell tolerance in vivo requires CTLA-4 engagement. Immunity 1997; 6: 411–417.
Ueda H, Howson J, Esposito L et al: Association of the T-cell regulatory gene CTLA4 with susceptibility to autoimmune disease. Nature 2003; 423: 506–511.
Oaks MK, Hallett KM : Cutting edge: a soluble form of CTLA-4 in patients with autoimmune thyroid disease. J Immunol 2000; 164: 5015–5018.
Liu MF, Wang CR, Chen PC, Fung LL : Increased expression of soluble cytotoxic T-lymphocyte-associated antigen-4 molecule in patients with systemic lupus erythematosus. Scand J Immunol 2003; 57: 568–572.
Acknowledgements
We thank Isabel Reis, Ana Tam, Maria João Antunes, the Associação dos Doentes com Lupus, and also Leonor Miranda, for their precious help in the recruitment of patients and collection of blood samples. We also thank the Serviço de Imunohemoterapia, Hospital Egas Moniz, as well as all the blood donors for their participation in this study. We thank António Coutinho, Werner Haas and Jocelyne Demengeot for advice and critical reading of the manuscript. M. Barreto was supported by Fundação para a Ciência e Tecnologia, SFRH/BD/1199/2000.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barreto, M., Santos, E., Ferreira, R. et al. Evidence for CTLA4 as a susceptibility gene for systemic lupus erythematosus. Eur J Hum Genet 12, 620–626 (2004). https://doi.org/10.1038/sj.ejhg.5201214
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejhg.5201214
Keywords
This article is cited by
-
Diagnosis and management of immune checkpoint inhibitor-associated acute kidney injury
Nature Reviews Nephrology (2022)
-
Novel human immunomodulatory T cell receptors and their double-edged potential in autoimmunity, cardiovascular disease and cancer
Cellular & Molecular Immunology (2021)
-
Genetic determinants of immune-related adverse events in patients with melanoma receiving immune checkpoint inhibitors
Cancer Immunology, Immunotherapy (2021)
-
Cardiorenal complications of immune checkpoint inhibitors
Nature Reviews Nephrology (2018)
-
Association of Hashimoto’s thyroiditis with cytotoxic T lymphocyte-associated antigen-4 (CTLA-4) and inducible co-stimulator (ICOS) genes in a Kuwaiti population
Endocrine (2013)