Abstract
Diabetic retinopathy (DR) is a common complication of diabetes and has been recognized as the leading cause of blindness in adults. Several interrelated molecular pathways are involved in the development of DR. Microvesicles (MVs) are cell membrane vesicles, which carry many biologic molecules, such as mRNAs, microRNAs, transcription factors, membrane lipids, membrane receptors, and other proteins. They may be involved in intercellular communication that can promote inflammation, angiogenesis, and coagulation. Recent studies have indicated that changes in the number and composition of MVs may reflect the pathologic conditions of DR. At present, MVs are well recognized as being involved in the pathophysiological conditions of tumors and cardio-metabolic diseases. However, the roles of MVs in DR have yet to be investigated. In this review, we provide an overview of DR-induced microvascular injury that is caused by MVs derived from endothelial and circulating cells, and discuss the possible mechanisms by which MVs can lead to endothelial dysfunction, coagulation and inflammation. In addition, the protective effects of preconditioned MVs and stem cell-derived MVs are also described . Understanding the involvement of MVs in the pathophysiological conditions of DR may provide insight into the disease mechanisms and may suggest novel therapeutic strategies for DR in the future.
Similar content being viewed by others
Introduction
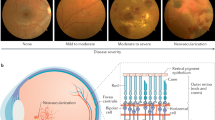
Diabetic retinopathy (DR) is a common complication of diabetes and is considered a microcirculatory disease of the retina that is caused by the deleterious metabolic effects of hyperglycemia1. The number of people at the risk of vision loss is predicted to double and the prevalence of DR is expected to increase by the year 20302. DR is staged into several levels of severity, including mild, moderate, and severe nonproliferative DR (NPDR), followed by advanced proliferative DR (PDR), which is defined by the presence of retinal neovascularization3. The early pathogenesis of DR may be due to the chronic degeneration of retinal nerve tissue, including reactive glial cell hyperplasia and neuronal apoptosis. In PDR, the proliferative neovasculature causes severe complications, such as vitreous hemorrhage and tractional retinal detachment, which may lead to irreversible vision loss4. The pathological mechanism of DR is still unclear.
The pathophysiology of DR development is highly complicated due to the involvement of multiple interlinked mechanisms that result in adaptive changes and cellular damage in the retina5. Thus, the underlying causes of DR have not been fully elucidated. In the past, retinopathy was largely characterized by its microvascular abnormalities, including vessel leakage, endothelial cell dysfunction, and vascular occlusion and degeneration6. However, recent studies have indicated that the retinal complications of diabetes are a composite of the structural and functional alterations in both the neuroglial and the microvascular compartments7. The exact mechanisms by which diabetic hyperglycemia induces neuronal and vascular alterations have not been completely defined in retinopathy. Retinal damage may be caused by a variety of mechanisms (Figure 1), including an increase in polyol pathway flux, the production of advanced glycation end products (AGEs), an increase in oxidative stress and protein kinase C (PKC) activation, but many of these hypotheses have not yet been verified in human studies8. DR also has similarities to chronic inflammatory diseases, namely: it can lead to increased vascular permeability, inflammatory cell infiltration, edema, angiogenesis, tissue destruction, and the expression of pro-inflammatory cytokines and chemokines in the retina. The increased expression of vasoactive factors and cytokines may play an important role in mediating functional and structural changes in the retina9. Recent studies have suggested that inflammation is also very important in the early onset of experimental DR, although human studies have not shown a consistent association between systemic inflammation markers and retinopathy10. Therefore, it remains uncertain whether inflammation also plays a crucial role in the occurrence and progression of DR in humans.
General pathological mechanism of DR. Hyperglycemia-induced biochemical pathways that contribute to DR pathophysiology. PKC: protein kinase C; AGE: advanced glycation end-product; DR: diabetic retinopathy; RAS: renin-angiotensin system; VEGF: vascular endothelial growth factor.
We recently reported that impaired proliferation, adhesion, and migratory activities were observed in cultured EPCs from the bone marrow of rats with DR, and this effect may contribute to prothrombotic conditions and atherothrombosis in the pathogenesis of DR11. Our previous publication further showed that EPCs may serve as a marker for DR progression and that simvastatin may be a promising candidate for the clinical management of DR; these EPCs decreased their mRNA expression levels of iNOS, Ang-1, and Ang-2 while increasing their eNOS mRNA expression in retinal tissue, suggesting a potential contribution to repairing endothelial dysfunction in rats with DR12. This study offers important insights and implications regarding the simvastatin increase in circulating EPCs, which consequently suppresses the formation and progression of DR12. In addition, the relationship between the C-reactive protein (CRP) level and DR remains controversial. Our recent meta-analysis study showed that the CRP level might be used as a biomarker for determining the severity of DR13. The in vitro studies by our group have shown that DR can be improved by an intravitreal injection of human umbilical mesenchymal stem cells14.
Microvesicles (MVs) are submicron membrane vesicles between 100 and 1000 nm that shed from the cell surface of both healthy and damaged cells15. By contrast, exosomes are smaller in diameter (between 40 and 100 nm) and are released during facultative or exocytosis16. The shedding of membrane MVs is a strictly regulated, cytoskeleton-dependent process that is enhanced by cytokines, the activation of apoptotic pathways, and reactive oxygen species17. Numerous studies now indicate that the transfer of information from MV-releasing cells to target cells via MVs that are circulating in the blood may be an important mechanism of intercellular communication18. MVs have biological activities and may be involved in thrombosis, inflammation, and angiogenesis, according to studies from our group and others19,20,21,22,23.
For example, MVs may communicate local inflammation, thus playing a key role in vascular diseases, such as DR24. DR is associated with increased local apoptosis or the activation of the retinal, vascular endothelial, and neural cells in the eye, both in humans and in animal models25. Reports indicate that MVs of different cellular origins might be locally generated in the eye of diabetic patients by the transfer of pro-inflammatory factors from the cells of origin26. Alternatively, the presence of MVs in the eye could also result from an increased vascular permeability that is associated with DR27. Thus, MVs are believed to serve as potential biomarkers for the diagnosis and prognosis of related vascular complications and the assessment of treatment response28. In the following sections, we summarize current knowledge of the role of MVs in the pathogenesis of DR, along with a projection of their importance in the screening and therapy of disease.
Biological properties of MVs
MVs are shed directly from the cell membrane by a “budding” process and typically range in size from approximately 100 to 1000 nm, although these values are somewhat arbitrary and subclass overlap may exist29. MVs are identified by the expression of phosphatidylserine (PS) on their surface, which is indicative of their release from apoptotic or activated cells30. In these cells, PS is externalized, whereas the membrane PS has a cytosolic orientation in quiescent cells31. As Annexin V binds preferentially to PS, it can be used to detect the exposed PS on the surface of apoptotic cells and the PS-positive MV subclass32. In addition, some researchers have found that a portion of circulating MVs are PS-negative, and it was suggested that the measurement of lactadherin may be a more sensitive alternative to Annexin V33,34. However, the number of other MV receptors is unknown; some MVs work in combination with Annexin I or are independent of Annexin I.
MVs are released from almost all cell types, including blood cells (such as erythrocytes, leukocytes, platelets, and macrophages/monocytes), vascular endothelial cells, smooth muscle cells, and the cells of other tissues/organs, under both pathological and physiological conditions35. Thus, MVs can be found in the urine, blood, vitreous fluid, atherosclerotic plaques of the vascular wall, and the extracellular spaces of organs. There are two well-known cellular processes that can lead to the formation of MVs: chemical and physical cell activations and apoptosis36. Many chemical and physical stimuli, such as thrombin, endotoxins, cytokines, tobacco smoke extract, hypoxia, unesterified cholesterol, and shear stress, have been reported to trigger cellular MV release in studies from several groups36. Other chemical stimuli of MV shedding include LDL and pro-inflammatory cytokines, such as IL-1β and TNFα. All of the abovementioned stimuli and factors may be involved in the development of diabetic vascular complications. Accordingly, there is an increase in circulating MVs in various diseases, including diabetes, cardiovascular diseases, diabetic complications, and abdominal aortic aneurysm37.
MVs display a versatile spectrum of membrane-anchored receptors and adhesion molecules on their surface, allowing specific interactions and crosstalk among various target cells38. When they are incorporated into the membranes of target cells, these receptors regulate cellular adhesive functions, such as promoting immune cell adhesion to the vascular endothelium. In addition to a common series of proteins, MVs have been shown to possess a specific lipid organization and composition39. A recent finding indicates that MVs contain double-stranded DNA, mRNA and noncoding RNA (microRNA and lncRNA)40. It is important that the mRNAs and microRNAs of the MVs are functional in the recipient cells. This suggests that the exchange of MV medium contents between cells may represent an efficient and effective form of inter-cellular communication. In addition, it is now known that RNA and protein sorting into MVs is highly regulated by a variety of patho-physiological stress stimuli and diseases41. This allows the cells to produce different functional characteristics that are tailored to the MVs and are reflective of their parent cell status. In this regard, any stress or disease conditions may be mirrored in the contents of the MVs, which can be used to develop future biomarkers for the diagnosis and prognosis of DR42.
At present, MVs have been implicated in mediating cellular communication through different mechanisms of interaction with the recipient cells, including: 1) direct ligand receptor interaction, leading to the activation of downstream signaling pathways, 2) extracellular protease cleavage of the membrane proteins of the MV, releasing soluble ligands to bind the target receptors of the recipient cells, 3) direct membrane fusion, leading to release of the contents of the MV into the recipient cells, and 4) internalization of the MVs by endocytic mechanisms (phagocytosis, macropinocytosis or receptor-mediated endocytosis)43. Considering the multiple attributes of the MVs and the secretion of MVs from a variety of different cell types within the retina, it is reasonable to expect that MVs may be involved in DR44. Although there is clinical evidence of the involvement of MVs in physiological and pathophysiological processes, the role of MVs is not well established and the mechanisms regulating MV formation are still unclear; these topics are still extensively studied in vivo and in vitro.
Involvement of MVs in the initiation and development of DR
The MVs released by endothelial cells, platelets, leukocytes and tumor cells have been shown to be pro-angiogenic both in vivo and in vitro45. Studies with human subjects indicate that the circulating levels of endothelial-derived MVs increase in retinopathy, obesity, physical inactivity, type 2 diabetes mellitus, end-stage renal disease and ischemic left ventricular dysfunction46. Importantly, the plasma concentrations of endothelial-derived MVs in these studies correlated with the degree of impaired vasodilation in these individuals47. Similarly, studies of diabetic patients with DR have indicated that the plasma concentrations of erythrocyte-derived, endothelial-derived, or platelet-derived MVs correlate with the circulating endothelial markers of inflammation (vascular cell adhesion molecule [VCAM]) and a prothrombotic state (von Willebrand factor)40. The composition, formation, catabolism, and general functions of MVs have been the subject of recent studies. Here, we focus on the latest works that implicate MVs in the initiation and development of DR and suggest MVs as markers of retinopathy.
The clinical works discussed above suggest that the levels of circulating MVs may serve as a new biomarker for endothelial dysfunction in neovascular retinopathy48. Although there is extensive literature demonstrating the involvement of MVs in various diseases, little is known about their roles in retinopathy. Analyses of vitreous fluids from patients with proliferative retinopathy have revealed remarkably increased levels of MVs, suggesting their involvement in retinopathy49. In support of this concept, studies have shown that MV antagonists block both choroidal and retinal angiogenesis. MVs from several abnormal clinical states of retinopathy have been shown to adversely affect endothelial function. Circulating MVs isolated from patients with proliferative retinopathy, myocardial infarction, or metabolic syndrome impair endothelium-dependent vasodilation ex vivo50. Moreover, MVs isolated from vitreous fluids provoke the recruitment of leukocytes in cultured endothelial cells. In addition to their role in promoting abnormal cell growth, alterations in MV generation have been demonstrated to play a key role in the atrophy of the choroid and retina51. MVs have also been found to play a key role in retinal microvascular function37. Basic studies have shown that MVs obtained from rats with proliferative retinopathy, or MVs generated in vitro using different stimuli on endothelial cells or retinal capillaries, can inhibit nitric oxide production in cultured retinal endothelial cells37. Moreover, these MVs also induce endothelial dysfunction in vivo38. MVs produced by the stimulation of several cell types are able to induce retinal endothelial cells to recruit monocytes in vitro.
The potential pathogenic mechanisms of MVs in the functional and structural alterations in DR are summarized in Figure 2. Under hyperglycemia conditions, the platelet-derived MVs (pMVs) released from platelets can lead to the elevation of MMPs/ADAMs, while the activated MMPs/ADAMs damage the mitochondria and cause the release of cytochrome c from the damaged mitochondria. This process accelerates capillary cell apoptosis, ultimately resulting in acellular capillaries and pericyte ghosts. Over time, the capillaries become hypoxic, a condition that ultimately leads to neovascularization. The endothelial cell-derived MVs (eMVs) released from endothelial cells may lead to photoreceptor/glial cell dysfunction or even loss and may ultimately result in neuro-retinal degeneration or damage. The monocyte-derived MVs (mMVs) released from monocytes may cause RPE dysfunction, ultimately resulting in blood-retinal barrier breakdown. In addition, the pMVs, eMVs and mMVs released from their parental cells under hyperglycemic conditions may lead to angiogenesis, vascular dysfunction, an inflammatory response and a coagulation cascade in the retina (Figure 3). Evidence from the literature suggests an important role of the MVs in retinal vascular dysfunction, retinal inflammation, and pathological angiogenesis during the development of DR43. The following sections will present additional evidence for the specific involvement of MVs in models of DR.
Pathogenic mechanisms of MVs in functional and structural alterations in DR. Under hyperglycemic conditions, platelets secrete pMVs, which leads to the elevation of MMPs/ADAMs, the activation of MMP/ADAM damage to the mitochondria, and the release of cytochrome c from the mitochondria. This accelerates capillary cell apoptosis, ultimately resulting in acellular capillaries and pericyte ghosts. With time, the capillaries become hypoxic, ultimately leading to neovascularization. Endothelial cells secrete eMVs, which leads to photoreceptor/glial cell dysfunction or loss, ultimately resulting in neuro-retinal degeneration or damage. Monocytes secrete mMVs, which leads to retinal pigment epithelium (RPE) dysfunction, ultimately resulting in blood-retinal barrier breakdown.
Pathogenic mechanisms of MVs contributing to DR pathophysiology. Under hyperglycemic conditions, platelets secrete pMVs, which leads to angiogenesis, vascular dysfunction, an inflammatory response and coagulation in the retina. Endothelial cells secrete eMVs, which leads to angiogenesis, vascular dysfunction, and an inflammatory response in the retina. Monocytes secrete mMVs, which leads to angiogenesis, vascular dysfunction, an inflammatory response and coagulation in retina.
Role of MVs in angiogenesis during DR
Proliferative DR is associated with a specific increase in endothelial MVs derived from new vessels52. Some studies suggest that the levels of endothelial-derived MVs, monocyte-derived MVs, and platelet-derived MVs are increased in patients with DR47. The increase in monocyte-derived MVs is most significant with the progression of DR from the nonproliferative stage to the proliferative stage, and monocyte-derived MVs are significantly higher in DR with areas of retinal neovascularization27. A recent study showed that MVs of endothelial, platelet, photoreceptor, and microglial origins can be identified in vitreous samples. Moreover, MVs of endothelial origin are the most abundant MV subpopulation in the vitreous samples from diabetic patients53.
The general consensus is that advanced glycation end products (AGE), hyperglycemia and ROS/NO imbalance can lead to retinal endothelial dysfunction and inflammation in the stage of DR. The circulating endothelial-derived MVs, monocyte-derived MVs, platelet-derived MVs, and MVs derived from retinal pigment epithelium cells may act as mediators and may influence endothelial function by simulating the expression of various adhesion molecules and the release of cytokines by endothelial cells, leading to morphological changes and angiogenesis induction in the microvascular endothelial cells51. The functional link between the endothelial-related pro-angiogenic response and erroneous local inflammation is proven by the recruitment of endogenous coagulation factor (FXII), which is observed on endothelial cell populations that present externalized PS by MV-delivery54.
Vitreous MVs stimulate endothelial cell proliferation in vitro and new vessel formation by a Matrigel plug model in vivo, which suggests that vitreous MVs may contribute to the progression of DR52. One of the suggested mechanisms of DR is increased MV release from endothelial cells and platelets, triggering TF in patients. In in vitro experiments, TF directly promotes ocular angiogenesis through MAPK activation and protein kinase C-dependent signaling55. Another mechanism is proposed for the transfer of secondary messenger molecules (lipids, receptors), mainly from immune cells (T lymphocytes), regulating vascular function. Moreover, the abnormal expression of miRNA in MVs may be involved in angiogenesis. Reduced expression of miRNA-200b decreases vascular endothelial growth factor (VEGF) expression, and increased expression of miR-29b regulates certain apoptotic genes and increases the expression of VEGF51; these miRNAs may be involved in uncontrolled cell proliferation in DR. However, the branch tube networks induced by MVs in DR are unstable and collapse over time31. Thus, elevated levels of monocyte-derived MVs and endothelial-derived MVs may serve as biomarkers of DR progression54,56.
Role of MVs with protease activities in DR
The diabetic environment stimulates the secretion of several MMPs that may participate in many diabetic complications, especially in DR57. Patients with DR and DR animal models have shown increased levels of MMP-9 and MMP-14 in their retina and vitreous fluid58. Retinal mRNA levels of MMP-2, MMP-9 and MMP-14 are elevated in diabetes, and the pro-forms of MMP-9 and MMP-14 are significantly elevated in the neovascular retinal membranes59. Our group recently reported that the production of MVs relies on a series of regulated steps that result in the induction and maturation of cellular MMP-14, leading to a remarkable accumulation of MMP-14 in nascent plasma membrane blebs and, finally, to caspase- and MAPK-dependent apoptosis and apoptotic MV generation60. This indicates that the proteolytically active MVs induced by tobacco smoke may be novel mediators of clinically important matrix destruction in smokers60. Therefore, MMPs could contribute to the disease process via MV-dependent pathways. MMPs play important roles in maintaining the integrity of the blood–retinal barrier (BRB) and in the development of DR61. The increased level of retinal MMPs in DR facilitates an increase in the BRB via the proteolytic degradation of tight junction proteins (ICAM, occluding) and the disruption of overall tight junction complexes62,63. We recently demonstrated persistent, enzymatically active a disintegrin and metalloprotease (ADAMs) on MVs in the intraluminal thrombus, adjacent to the aneurysmal wall64. The production of ADAM10- and ADAM17-positive MVs from smoke-exposed neutrophils provides a novel molecular mechanism for the vastly accelerated risk of abdominal aortic aneurysm64. Increased expression of ADAMs is observed in retinal pericytes incubated in high glucose and in the retina in DR, and increased ADAM-9 activity is considered to compromise the survival of retinal pericytes65. Glycated low-density lipoprotein (LDL) and heavily oxidized LDL, which is elevated in DR, increases ADAM-10 in retinal pericytes66. ADAM-15 is also up-regulated in retinal vascular cells cultured under high glucose conditions and in the human retina showing active neovascularization65,66.
Role of MVs in endothelial dysfunction and vascular inflammation during DR development
The function of endothelial cells is key to the formation and propagation of atherosclerotic plaques, and MVs are involved in the intercellular transfer of both pro-apoptotic and pro-angiogenic signals67. Studies in diabetic patients show that MVs can affect vascular endothelial function. When two consecutive fat-rich mixed meals were given to T2DM patients, the results showed that impaired endothelium-dependent vasodilatation is associated with increased levels of circulating endothelial-derived MVs and platelet-derived MVs68. An increased level of endothelial-derived MVs is positively correlated with the impairment of coronary endothelial function in patients with T2DM69. T2DM patients show reduced endothelium-dependent flow-mediated dilation (FMD) and increased brachial ankle pulse wave velocity. We previously reported that cholesterol enrichment of human macrophages/monocytes causes the generation of TF+ MVs with high procoagulant activity, which may contribute to endothelial dysfunction in hyperglucose conditions23. In addition, we further reported that exposure of human macrophages to tobacco smoke causes the release of proteolytic MMP-14+ MVs through the activation of JNK and p38 MAPK60. Moreover, MPs derived from human atherosclerotic plaques incorporate the ICAM-1 of endothelial cells to recruit inflammatory cells, which suggests that plaque-derived MPs promote inflammation progression70,71. MVs isolated from diabetic patients express more CD40L and were more potent in inducing endothelial proliferation when compared with non-diabetic MVs or circulating MVs72.
In vitro and in vivo experiments have indicated that MVs might contribute to endothelial dysfunction by decreasing the production of nitric oxide (NO) and prostacyclin in endothelial cells73. Co-culture of endothelial-derived MVs with aortic rings and cultured endothelial cells leads to increased superoxide generation, reduced NO production, and impaired vascular relaxation induced by acetylcholine74. The T lymphocytes derived from the MVs of diabetic patients damage the shear stress-induced dilatation of mouse mesenteric arteries by affecting the production of prostacyclin and NO75. Our recent study showed that tobacco smoke exposure increases the release of procoagulant MVs22. Our latest publication further showed that tobacco smoke exposure in human macrophages causes the generation of MMP-14+ MVs with strong procoagulant activities; these MVs degrade a major component of the arterial wall matrix, suggesting their potential contribution to endothelial dysfunction in patients with cardiovascular disease76. In addition, a recent study reported that endothelial-derived MVs exposed to high glucose could significantly increase macrophage infiltration and could impair endothelial function and adhesion molecule expression, causing higher ROS levels and increased nicotinamide adenine dinucleotide phosphate oxidase (NOX) activity77. Therefore, MVs derived from endothelial cell-based methodologies could be used to study vascular inflammation in diabetic vascular diseases.
Leukocyte-endothelial interactions and the subsequent endothelial migration of leukocytes are important early stage events in the development of DR78. In vitro experiments have shown that MVs derived from activated platelets or apoptotic endothelial cells act as cellular effectors, disseminating pro-adhesive and pro-inflammatory potentials in the vasculature55. Activated platelets and the platelets derived from MVs that were isolated from DR patients facilitate the interaction between monocytes and endothelial cells74. Lee et al showed that MVs facilitate platelet string formation at the surface of human umbilical vein endothelial cells (HUVECs) before the MVs are internalized into the HUVECs in vitro79. This uptake induces ROS production, which is necessary for the expression of von Willebrand factor on the endothelial cell surface and the subsequent interaction between endothelial cells and platelets80. We recently demonstrated that unesterified cholesterol-induced MVs (UCMVs) from human endothelial cells robustly increased leukocyte recruitment to cultured human endothelial monolayers in vitro, aortic endothelium ex vivo, and microvascular endothelium in vivo20. The malondialdehyde-like epitopes on the UCMV surface intercede monocyte recruitment to the endothelial cells through lectin-like oxidized low-density lipoprotein receptor-1 (LOX1)81. As reviewed above, MVs derived from different conditions may contain different functional factors, which decide their harmful properties (Table 1). These studies indicate the potential importance of MVs in vascular inflammation, endothelial activation, and leukocyte recruitment, which may lead to vascular diseases and DR.
Prothrombotic MVs in DR
Diabetes is a procoagulant state and retinal microthromboses occur in DR. An increased prevalence of platelet-fibrin microthrombi has been observed in the retinal microvasculature in both experimental rodent models of diabetes and in human eyes from diabetic patients82,83. It is well established that diabetes induces endothelial dysfunction and injury, which can lead to increased leukocyte and platelet adhesion in the retinal microvasculature, suggesting that microthromboses are concomitant with or secondary to capillary damage84. Studies have found that the levels of procoagulant MVs are increased in patients with diabetes and DR; increases in the highly procoagulant TF-bearing MVs coincide with strongly elevated levels of coagulation activation markers85. Another study also showed that procoagulant endothelial-derived MVs, platelet-derived MVs, and monocyte-derived MVs are significantly increased in patients with diabetes, even in well-controlled DM without DR86. Blood platelet-derived MVs are more likely to adhere to the diabetic endothelium than healthy vessels, which may contribute to the occlusion of injured retinal capillaries87. In a cross-sectional study of patients with type II diabetes mellitus and nondiabetic subjects, it was demonstrated that procoagulant endothelial-derived MVs are an independent risk factor for retinopathy88. Therefore, elevated levels of MVs may be associated with an increased risk of thrombo-embolic DR.
Procoagulant MVs can initiate and propagate coagulation in diabetes, and the activated platelets release platelet-derived MVs that lead to further thrombin formation, which may explain the novel mechanisms of hypercoagulability in DR89. Razmara et al90 reported an increase in procoagulant MVs in DR that correlated with the degree of diabetic duration. In addition to the roles of MVs in thrombosis, these coagulation and fibrinolytic factors increase the inflammatory responses that have been implicated in DR. The administration of anti-platelet drugs can significantly decrease circulating procoagulant MVs and platelets in patients with DR91. Taken together, elevated levels of prothrombotic MVs adhered to the injured diabetic endothelium may contribute to both ischemia and inflammation in DR.
Therapeutic potential of MVs in DR
As reviewed above, MVs derived from disease conditions elicit adverse effects on DR. Recent research has also found that the MVs collected from various stem cells or ischemic preconditioning provide vascular-protection, which may have therapeutic potential in the treatment of DR92. We will summarize the recent reports of the role of stem cell-derived, gene-modified cell-derived, and stress-preconditioned MVs in retinal protection, including inhibited endothelial dysfunction, reduced oxidative stress, and limited inflammatory response.
Various types of stem cells (adult stem cells, embryonic stem cells, and induced pluripotent stem cells) have been extensively studied for therapeutic potential in microvascular disease93. It was previously thought that stem cell therapy appeared to regenerate tissue through reproduction and then differentiation, but recent studies have proven that the advantageous effects of stem cells in the repair of ischemic tissue is through the release of autocrine and paracrine factors94. Stem cells can secrete numerous types of molecules/factors, including microRNAs, proteins, growth factors, proteasomes, antioxidants and MVs. In particular, MVs have gained specific attention in cell-free-based stem cell therapy for microvascular disease. He et al reported that human ESC-derived MSCs secreted MVs. By using an ex vivo model of ischemia/reperfusion injury, they observed that these purified MVs were able to decrease injury size in mouse retinas. A recent study showed that MV treatment restored the redox state and energy depletion in mouse retinas within 30 min after I/R, which was evidenced by a reduction in oxidative stress and an elevation in ATP and NADH levels95. Moreover, phosphorylated PFKFB3 and active CD73 are also wrapped in MSC-derived MVs. In addition, MV treatment could decrease systemic inflammation in diabetic mice96. Thus, MSC-derived MVs may have significant therapeutic potential for patients suffering from DR.
Recently, a study by Bauchl et al97 found that human CD34+ stem cells had the ability to secrete MVs. In vitro, it was shown that MVs replicated angiogenic activity by increasing endothelial cell proliferation, viability and tube-like formation on Matrigel. In vivo, it was shown that both stem cells and MVs decreased the formation of endothelial vessel-like structures, which was accompanied by a greatly raised proportion of endothelial cells in the Matrigel plug. In the angiogenesis assay, pellets containing stem cell-derived MVs were associated with greater vessel formation98. Thus, these findings demonstrate that MVs are the key paracrine component of CD34+-cell-induced vessel growth. However, the mechanisms underlying CD34+-MV-mediated angiogenesis could be ascribed to the overall transfer of exosomal contents (proteins/RNAs) into the cytosol of endothelial cells or MV receptor-induced activation of angiogenic signaling cascades54. Indeed, Ju et al99 have shown data demonstrating that CD34+-MVs are significantly enriched with pro-angiogenic miR-130a and miR-126 compared with CD34-MVs. Therefore, the MV-mediated delivery of miR-130a and miR-126 to an ischemic area may represent a major mechanism that explains the preservation of vascular function in DR mice treated with CD34+ cells.
Recently, Choi et al100 performed a microRNA array for profiling the miRNAs in MSC-derived MVs. These MSCs were isolated from mouse bone marrow and subjected to cycles of anoxia-reoxygenation as ischemic preconditioning (IPC). Lozito et al101 showed that the levels of miR-22 were higher and were accompanied by miR-210, miR-21, miR-24, and miR-199a-3p, in MVs collected from IPC-MSCs than in control MVs. In particular, an in vivo treatment of mice with MVs from IPC-MSCs resulted in a significant reduction of ischemia and apoptosis by direct injection into the retina102. In addition, these authors identified that MV-IPC-mediated protective effects are highly associated with the transfer of miR-22 to the surrounding cells. Nonetheless, whether these preconditioned MVs contain ligands/receptors or other beneficial proteins remains unclear. As reviewed above, stem cell-derived, gene-modified cell-derived, and stress-preconditioned MVs may contain different functional factors that may decide their beneficial properties (Table 2).
Conclusion
Circulating MVs show great promise not only as biomarkers in vascular disease diagnosis but also as potential targets for treatment in DR in the future. The evaluation of MVs could provide value in the clinical setting of DR patients. Moreover, monitoring of the process leading to MV formation may be relevant in controlling DR progression. Despite the fact that the mechanisms that regulate MV formation are barely understood, it has been documented that the cellular machinery leading to MV shedding involves plasma membrane remodeling and PS externalization. From the research data, it seems reasonable to assume that the variable expression and profiles of MVs and microRNAs might be involved in a variety of inflammatory and neoangiogenic processes. This clearly suggests that the pharmacological regulation and control of MV shedding remains a challenge in DR.
References
Taylor-Phillips S, Mistry H, Leslie R, Todkill D, Tsertsvadze A, Connock M, et al. Extending the diabetic retinopathy screening interval beyond 1 year: systematic review. Br J Ophthalmol 2016; 100: 105–14.
Martinell M, Dorkhan M, Stalhammar J, Storm P, Groop L, Gustavsson C . Prevalence and risk factors for diabetic retinopathy at diagnosis (DRAD) in patients recently diagnosed with type 2 diabetes (T2D) or latent autoimmune diabetes in the adult (LADA). J Diabetes Complications 2016; 30: 1456–61.
Hu W, Wang R, Li J, Zhang J, Wang W . Association of irisin concentrations with the presence of diabetic nephropathy and retinopathy. Ann Clin Biochem 2016; 53: 67–74.
de Carlo TE, Bonini Filho MA, Baumal CR, Reichel E, Rogers A, Witkin AJ, et al. Evaluation of preretinal neovascularization in proliferative diabetic retinopathy using optical coherence tomography angiography. Ophthalmic Surg Lasers Imaging Retina 2016; 47: 115–9.
Xu G, Kang D, Zhang C, Lou H, Sun C, Yang Q, et al. Erythropoietin protects retinal cells in diabetic rats through upregulating ZnT8 via activating ERK pathway and inhibiting HIF-1alpha expression. Invest Ophthalmol Vis Sci 2015; 56: 8166–78.
Ahmadi Majd S, Rabbani Khorasgani M, Moshtaghian SJ, Talebi A, Khezri M . Application of Chitosan/PVA Nano fiber as a potential wound dressing for streptozotocin-induced diabetic rats. Int J Biol Macromol 2016; 92: 1162–8.
Du MR, Ju GX, Li NS, Jiang JL . Role of asymmetrical dimethylarginine in diabetic microvascular complications. J Cardiovasc Pharmacol 2016; 68: 322–6.
Duarte DA, Papadimitriou A, Gilbert RE, Thai K, Zhang Y, Rosales MA, et al. Conditioned medium from early-outgrowth bone marrow cells is retinal protective in experimental model of diabetes. PLoS One 2016; 11: e0147978.
Ezquer M, Urzua CA, Montecino S, Leal K, Conget P, Ezquer F . Intravitreal administration of multipotent mesenchymal stromal cells triggers a cytoprotective microenvironment in the retina of diabetic mice. Stem Cell Res Ther 2016; 7: 42.
Jiang T, Chang Q . Protective effects of melatonin on retinal inflammation and oxidative stress in experimental diabetic retinopathy. Oxid Med Cell Longev 2016; 2016: 3528274.
Zhang W, Yan H . Dysfunction of circulating endothelial progenitor cells in type 1 diabetic rats with diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol 2013; 251: 1123–31.
Zhang W, Yan H . Simvastatin increases circulating endothelial progenitor cells and reduces the formation and progression of diabetic retinopathy in rats. Exp Eye Res 2012; 105: 1–8.
Song J, Chen S, Liu X, Duan H, Kong J, Li Z . Relationship between C-reactive protein level and diabetic retinopathy: a systematic review and meta-analysis. PLoS One 2015; 10: e0144406.
Kong JH, Zheng D, Chen S, Duan HT, Wang YX, Dong M, et al. A comparative study on the transplantation of different concentrations of human umbilical mesenchymal cells into diabetic rats. Int J Ophthalmol 2015; 8: 257–62.
Boysen J, Nelson M, Magzoub G, Maiti GP, Sinha S, Goswami M, et al. Dynamics of microvesicle generation in B-cell chronic lymphocytic leukemia: implication in disease progression. Leukemia 2017; 31: 350–60.
Zhang HG, Cao P, Teng Y, Hu X, Wang Q, Yeri AS, et al. Isolation, identification, and characterization of novel nanovesicles. Oncotarget 2016; 7: 41346–62.
Kang T, Jones TM, Naddell C, Bacanamwo M, Calvert JW, Thompson WE, et al. Adipose-derived stem cells induce angiogenesis via microvesicle transport of miRNA-31. Stem Cells Transl Med 2016; 5: 440–50.
Kreger BT, Dougherty AL, Greene KS, Cerione RA, Antonyak MA . Microvesicle cargo and function changes upon induction of cellular transformation. J Biol Chem 2016; 291: 19774–85.
Liu ML, Williams KJ, Werth VP . Microvesicles in autoimmune diseases. Adv Clin Chem 2016; 77: 125–75.
Liu ML, Williams KJ . Microvesicles: potential markers and mediators of endothelial dysfunction. Curr Opin Endocrinol Diabetes Obes 2012; 19: 121–7.
Liu ML, Scalia R, Mehta JL, Williams KJ . Cholesterol-induced membrane microvesicles as novel carriers of damage-associated molecular patterns: mechanisms of formation, action, and detoxification. Arterioscler Thromb Vasc Biol 2012; 32: 2113–21.
Li M, Yu D, Williams KJ, Liu ML . Tobacco smoke induces the generation of procoagulant microvesicles from human monocytes/macrophages. Arterioscler Thromb Vasc Biol 2010; 30: 1818–24.
Liu ML, Reilly MP, Casasanto P, McKenzie SE, Williams KJ . Cholesterol enrichment of human monocyte/macrophages induces surface exposure of phosphatidylserine and the release of biologically-active tissue factor-positive microvesicles. Arterioscler Thromb Vasc Biol 2007; 27: 430–5.
Wang Y, Chen LM, Liu ML . Microvesicles and diabetic complications--novel mediators, potential biomarkers and therapeutic targets. Acta Pharmacol Sin 2014; 35: 433–43.
Mata-Cases M, Mauricio D, Franch-Nadal J . Clinical characteristics of type 2 diabetic patients on basal insulin therapy with adequate fasting glucose control who do not achieve HbA1c targets. J Diabetes 2017; 9: 34–44.
Rondina MT, Tatsumi K, Bastarache JA, Mackman N . Microvesicle tissue factor activity and interleukin-8 levels are associated with mortality in patients with influenza A/H1N1 infection. Crit Care Med 2016; 44: e574–8.
Stepien E, Kablak-Ziembicka A, Czyz J, Przewlocki T, Malecki M . Microparticles, not only markers but also a therapeutic target in the early stage of diabetic retinopathy and vascular aging. Expert Opin Ther Targets 2012; 16: 677–88.
Salem MA, Adly AA, Ismail EA, Darwish YW, Kamel HA . Platelets microparticles as a link between micro- and macro-angiopathy in young patients with type 1 diabetes. Platelets 2015; 26: 682–8.
Kumar S, Milani G, Takatsuki H, Lana T, Persson M, Frasson C, et al. Sensing protein antigen and microvesicle analytes using high-capacity biopolymer nano-carriers. Analyst 2016; 141: 836–46.
Bussche L, Rauner G, Antonyak M, Syracuse B, McDowell M, Brown AM, et al. Microvesicle-mediated Wnt/β-catenin signaling promotes interspecies mammary stem/progenitor cell growth. J Biol Chem 2016; 291: 24390–405.
Nielsen TB, Nielsen MH, Handberg A . In vitro incubation of platelets with oxLDL does not induce microvesicle release when measured by sensitive flow cytometry. Front Cardiovasc Med 2015; 2: 37.
Saari H, Lazaro-Ibanez E, Viitala T, Vuorimaa-Laukkanen E, Siljander P, Yliperttula M . Microvesicle- and exosome-mediated drug delivery enhances the cytotoxicity of Paclitaxel in autologous prostate cancer cells. J Control Release 2015; 220: 727–37.
Musunuri S, Khoonsari PE, Mikus M, Wetterhall M, Haggmark-Manberg A, Lannfelt L, et al. Increased levels of extracellular microvesicle markers and decreased levels of endocytic/exocytic proteins in the Alzheimer's disease brain. J Alzheimers Dis 2016; 54: 1671–86.
Lopes-Rodrigues V, Di Luca A, Sousa D, Seca H, Meleady P, Henry M, et al. Multidrug resistant tumour cells shed more microvesicle-like EVs and less exosomes than their drug-sensitive counterpart cells. Biochim Biophys Acta 2016; 1860: 618–27.
Wu YW, Goubran H, Seghatchian J, Burnouf T . Smart blood cell and microvesicle-based Trojan horse drug delivery: Merging expertise in blood transfusion and biomedical engineering in the field of nanomedicine. Transfus Apher Sci 2016; 54: 309–18.
Nielsen MH, Irvine H, Vedel S, Raungaard B, Beck-Nielsen H, Handberg A . The impact of lipoprotein-associated oxidative stress on cell-specific microvesicle release in patients with familial hypercholesterolemia. Oxid Med Cell Longev 2016; 2016: 2492858.
Jansen F, Yang X, Franklin BS, Hoelscher M, Schmitz T, Bedorf J, et al. High glucose condition increases NADPH oxidase activity in endothelial microparticles that promote vascular inflammation. Cardiovasc Res 2013; 98: 94–106.
Balabushevich NG, Pechenkin MA, Shibanova ED, Volodkin DV, Mikhalchik EV . Multifunctional polyelectrolyte microparticles for oral insulin delivery. Macromol Biosci 2013; 13: 1379–88.
Ryu JH, Lim SY, Ryu DR, Kang DH, Choi KB, Kim SJ . Association between vascular access failure and microparticles in hemodialysis patients. Kidney Res Clin Pract 2012; 31: 38–47.
Müller G, Schneider M, Biemer-Daub G, Wied S . Microvesicles released from rat adipocytes and harboring glycosylphosphatidylinositol-anchored proteins transfer RNA stimulating lipid synthesis. Cell Signal 2011; 23: 1207–23.
Andrews AM, Lutton EM, Merkel SF, Razmpour R, Ramirez SH . Mechanical injury induces brain endothelial-derived microvesicle release: implications for cerebral vascular injury during traumatic brain injury. Front Cell Neurosci 2016; 10: 43.
Chen Y, Li G, Liu Y, Werth VP, Williams KJ, Liu ML . Translocation of endogenous danger signal HMGB1 from nucleus to membrane microvesicles in macrophages. J Cell Physiol 2016; 231: 2319–26.
Berezin AE, Kremzer AA, Berezina TA, Martovitskaya YV . The pattern of circulating microparticles in patients with diabetes mellitus with asymptomatic atherosclerosis. Acta Clin Belg 2016; 71: 38–45.
Ben-Dov IZ, Whalen VM, Goilav B, Max KE, Tuschl T . Cell and microvesicle urine microRNA deep sequencing profiles from healthy individuals: observations with potential impact on biomarker studies. PLoS One 2016; 11: e0147249.
Wang Z, Emond ZM, Flynn ME, Swaminathan S, Kibbe MR . Microparticle levels after arterial injury and NO therapy in diabetes. J Surg Res 2016; 200: 722–31.
Chronopoulos A, Trudeau K, Roy S, Huang H, Vinores SA, Roy S . High glucose-induced altered basement membrane composition and structure increases trans-endothelial permeability: implications for diabetic retinopathy. Curr Eye Res 2011; 36: 747–53.
Jung KH, Chu K, Lee ST, Bahn JJ, Kim JH, Kim M, et al. Risk of macrovascular complications in type 2 diabetes mellitus: endothelial microparticle profiles. Cerebrovasc Dis 2011; 31: 485–93.
Randriamboavonjy V, Fleming I . Platelet function and signaling in diabetes mellitus. Curr Vasc Pharmacol 2012; 10: 532–8.
Sun AL, Deng JT, Guan GJ, Chen SH, Liu YT, Cheng J, et al. Dipeptidyl peptidase-IV is a potential molecular biomarker in diabetic kidney disease. Diab Vasc Dis Res 2012; 9: 301–8.
Barutta F, Tricarico M, Corbelli A, Annaratone L, Pinach S, Grimaldi S, et al. Urinary exosomal microRNAs in incipient diabetic nephropathy. PLoS One 2013; 8: e73798.
Condorelli RA, Calogero AE, Favilla V, Morgia G, Johnson EO, Castiglione R, et al. Arterial erectile dysfunction: different severities of endothelial apoptosis between diabetic patients "responders" and "non responders" to sildenafil. Eur J Intern Med 2013; 24: 234–40.
Tsimerman G, Roguin A, Bachar A, Melamed E, Brenner B, Aharon A . Involvement of microparticles in diabetic vascular complications. Thromb Haemost 2011; 106: 310–21.
Alexandru N, Badila E, Weiss E, Cochior D, Stepien E, Georgescu A . Vascular complications in diabetes: Microparticles and microparticle associated microRNAs as active players. Biochem Biophys Res Commun 2016; 472: 1–10.
Beltramo E, Lopatina T, Berrone E, Mazzeo A, Iavello A, Camussi G, et al. Extracellular vesicles derived from mesenchymal stem cells induce features of diabetic retinopathy in vitro. Acta Diabetol 2014; 51: 1055–64.
Chiva-Blanch G, Suades R, Padro T, Vilahur G, Pena E, Ybarra J, et al. Microparticle shedding by erythrocytes, monocytes and vascular smooth muscular cells is reduced by aspirin in diabetic patients. Rev Esp Cardiol (Engl Ed) 2016; 69: 672–80.
Ogata N, Imaizumi M, Nomura S, Shozu A, Arichi M, Matsuoka M, et al. Increased levels of platelet-derived microparticles in patients with diabetic retinopathy. Diabetes Res Clin Pract 2005; 68: 193–201.
Mishra M, Kowluru RA . The role of DNA methylation in the metabolic memory phenomenon associated with the continued progression of diabetic retinopathy. Invest Ophthalmol Vis Sci 2016; 57: 5748–57.
Mishra M, Flaga J, Kowluru RA . Molecular mechanism of transcriptional regulation of matrix metalloproteinase-9 in diabetic retinopathy. J Cell Physiol 2016; 231: 1709–18.
Kwon JW, Choi JA, Jee D . Matrix metalloproteinase-1 and matrix metalloproteinase-9 in the aqueous humor of diabetic macular edema patients. PLoS One 2016; 11: e0159720.
Li CJ, Liu Y, Chen Y, Yu D, Williams KJ, Liu ML . Novel proteolytic microvesicles released from human macrophages after exposure to tobacco smoke. Am J Pathol 2013; 182: 1552–62.
Abu El-Asrar AM, Alam K, Nawaz MI, Mohammad G, Van den Eynde K, Siddiquei MM, et al. Upregulation of thrombin/matrix metalloproteinase-1/protease-activated receptor-1 chain in proliferative diabetic retinopathy. Curr Eye Res 2016; 41: 1590–600.
De Groef L, Andries L, Lemmens K, Van Hove I, Moons L . Matrix metalloproteinases in the mouse retina: a comparative study of expression patterns and MMP antibodies. BMC Ophthalmol 2015; 15: 187.
Chen Y, Wang W, Liu F, Tang L, Tang R, Li W . Apoptotic effect of mtrix metalloproteinases 9 in the development of diabetic retinopathy. Int J Clin Exp Pathol 2015; 8: 10452–9.
Folkesson M, Li C, Frebelius S, Swedenborg J, Wagsater D, Williams KJ, et al. Proteolytically active ADAM10 and ADAM17 carried on membrane microvesicles in human abdominal aortic aneurysms. Thromb Haemost 2015; 114: 1165–74.
Guaiquil V, Swendeman S, Yoshida T, Chavala S, Campochiaro PA, Blobel CP . ADAM9 is involved in pathological retinal neovascularization. Mol Cell Biol 2009; 29: 2694–703.
Maretzky T, Blobel CP, Guaiquil V . Characterization of oxygen-induced retinopathy in mice carrying an inactivating point mutation in the catalytic site of ADAM15. Invest Ophthalmol Vis Sci 2014; 55: 6774–82.
Ayers L, Nieuwland R, Kohler M, Kraenkel N, Ferry B, Leeson P . Dynamic microvesicle release and clearance within the cardiovascular system: triggers and mechanisms. Clin Sci (Lond) 2015; 129: 915–31.
Yang F, Li M, Liu Y, Wang T, Feng Z, Cui H, et al. Glucose and magnetic-responsive approach toward in situ nitric oxide bubbles controlled generation for hyperglycemia theranostics. J Control Release 2016; 228: 87–95.
Ousmaal Mel F, Martinez MC, Andriantsitohaina R, Chabane K, Gaceb A, Mameri S, et al. Increased monocyte/neutrophil and pro-coagulant microparticle levels and overexpression of aortic endothelial caveolin-1beta in dyslipidemic sand rat, Psammomys obesus. J Diabetes Complications 2016; 30: 21–9.
Chahed S, Leroyer AS, Benzerroug M, Gaucher D, Georgescu A, Picaud S, et al. Increased vitreous shedding of microparticles in proliferative diabetic retinopathy stimulates endothelial proliferation. Diabetes 2010; 59: 694–701.
Bergeron A, Pucci L, Bezzi P, Regazzi R . Analysis of synaptic-like microvesicle exocytosis of B-cells using a live imaging technique. PLoS One 2014; 9: e87758.
Jansen F, Yang X, Hoelscher M, Cattelan A, Schmitz T, Proebsting S, et al. Endothelial microparticle-mediated transfer of microRNA-126 promotes vascular endothelial cell repair via SPRED1 and is abrogated in glucose-damaged endothelial microparticles. Circulation 2013; 128: 2026–38.
Kurtzman N, Zhang L, French B, Jonas R, Bantly A, Rogers WT, et al. Personalized cytomic assessment of vascular health: Evaluation of the vascular health profile in diabetes mellitus. Cytometry B Clin Cytom 2013; 84: 255–66.
Jansen F, Wang H, Przybilla D, Franklin BS, Dolf A, Pfeifer P, et al. Vascular endothelial microparticles-incorporated microRNAs are altered in patients with diabetes mellitus. Cardiovasc Diabetol 2016; 15: 49.
Gleizes C, Kreutter G, Abbas M, Kassem M, Constantinescu AA, Boisrame-Helms J, et al. β Cell membrane remodelling and procoagulant events occur in inflammation-driven insulin impairment: a GLP-1 receptor dependent and independent control. J Cell Mol Med 2016; 20: 231–42.
Zhou L, Qi XL, Xu MX, Mao Y, Liu ML, Song HM . Microparticles: new light shed on the understanding of venous thromboembolism. Acta Pharmacol Sin 2014; 35: 1103–10.
Jansen F, Yang X, Baumann K, Przybilla D, Schmitz T, Flender A, et al. Endothelial microparticles reduce ICAM-1 expression in a microRNA-222-dependent mechanism. J Cell Mol Med 2015; 19: 2202–14.
Heinrich LF, Andersen DK, Cleasby ME, Lawson C . Long-term high fat feeding of rats results in increased numbers of circulating microvesicles with pro-inflammatory effects on endothelial cells. Br J Nutr 2015; 113: 1704–11.
Lee H, Zhang D, Zhu Z, Dela Cruz CS, Jin Y . Epithelial cell-derived microvesicles activate macrophages and promote inflammation via microvesicle-containing microRNAs. Sci Rep 2016; 6: 35250.
Khalyfa A, Khalyfa AA, Akbarpour M, Connes P, Romana M, Lapping-Carr G, et al. Extracellular microvesicle microRNAs in children with sickle cell anaemia with divergent clinical phenotypes. Br J Haematol 2016; 174: 786–98.
Ay L, Thaler J, Brix JM, Schernthaner GH, Ay C, Pabinger I, et al. Decrease in microvesicle-associated tissue factor activity in morbidly obese patients after bariatric surgery. Int J Obes (Lond) 2016; 40: 768–72.
Ponto KA, Koenig J, Peto T, Lamparter J, Raum P, Wild PS, et al. Prevalence of diabetic retinopathy in screening-detected diabetes mellitus: results from the Gutenberg Health Study (GHS). Diabetologia 2016; 59: 1913–9.
Walsh TG, Metharom P, Berndt MC . The functional role of platelets in the regulation of angiogenesis. Platelets 2015; 26: 199–211.
Achiron A, Lagstein O, Glick M, Gur Z, Bartov E, Burgansky-Eliash Z . Quantifying metamorphopsia in patients with diabetic macular oedema and other macular abnormalities. Acta Ophthalmol 2015; 93: e649–53.
Nomura S, Shouzu A, Taomoto K, Togane Y, Goto S, Ozaki Y, et al. Assessment of an ELISA kit for platelet-derived microparticles by joint research at many institutes in Japan. J Atheroscler Thromb 2009; 16: 878–87.
Nomura S, Omoto S, Yokoi T, Fujita S, Ozasa R, Eguchi N, et al. Effects of miglitol in platelet-derived microparticle, adiponectin, and selectin level in patients with type 2 diabetes mellitus. Int J Gen Med 2011; 4: 539–45.
Shimazu T, Inami N, Satoh D, Kajiura T, Yamada K, Iwasaka T, et al. Effect of acarbose on platelet-derived microparticles, soluble selectins, and adiponectin in diabetic patients. J Thromb Thrombolysis 2009; 28: 429–35.
Zhang X, McGeoch SC, Johnstone AM, Holtrop G, Sneddon AA, MacRury SM, et al. Platelet-derived microparticle count and surface molecule expression differ between subjects with and without type 2 diabetes, independently of obesity status. J Thromb Thrombolysis 2014; 37: 455–63.
Raturi A, Miersch S, Hudson JW, Mutus B . Platelet microparticle-associated protein disulfide isomerase promotes platelet aggregation and inactivates insulin. Biochim Biophys Acta 2008; 1778: 2790–6.
Razmara M, Hjemdahl P, Ostenson CG, Li N . Platelet hyperprocoagulant activity in Type 2 diabetes mellitus: attenuation by glycoprotein IIb/IIIa inhibition. J Thromb Haemost 2008; 6: 2186–92.
Nomura S, Inami N, Shouzu A, Omoto S, Kimura Y, Takahashi N, et al. The effects of pitavastatin, eicosapentaenoic acid and combined therapy on platelet-derived microparticles and adiponectin in hyperlipidemic, diabetic patients. Platelets 2009; 20: 16–22.
Xie L, Mao M, Zhou L, Jiang B . Spheroid mesenchymal stem cells and mesenchymal stem cell-derived microvesicles: two potential therapeutic strategies. Stem Cells Dev 2016; 25: 203–13.
Bobis-Wozowicz S, Kmiotek K, Sekula M, Kedracka-Krok S, Kamycka E, Adamiak M, et al. Human induced pluripotent stem cell-derived microvesicles transmit RNAs and proteins to recipient mature heart cells modulating cell fate and behavior. Stem Cells 2015; 33: 2748–61.
Boregowda SV, McKenna DH, Ortiz LA, Wang Y, Fu B, Sun X, et al. Differentially expressed microRNAs in bone marrow mesenchymal stem cell-derived microvesicles in young and older rats and their effect on tumor growth factor-beta1-mediated epithelial-mesenchymal transition in HK2 cells. Stem Cell Res Ther 2015; 6: 185.
Solorio LD, Phillips LM, McMillan A, Cheng CW, Dang PN, Samorezov JE, et al. Spatially organized differentiation of mesenchymal stem cells within biphasic microparticle-incorporated high cell density osteochondral tissues. Adv Healthc Mater 2015; 4: 2306–13.
Chiva-Blanch G, Suades R, Crespo J, Pena E, Padro T, Jimenez-Xarrie E, et al. Microparticle shedding from neural progenitor cells and vascular compartment cells is increased in ischemic stroke. PLoS One 2016; 11: e0148176.
Baulch JE, Acharya MM, Allen BD, Ru N, Chmielewski NN, Martirosian V, et al. Cranial grafting of stem cell-derived microvesicles improves cognition and reduces neuropathology in the irradiated brain. Proc Natl Acad Sci U S A 2016; 113: 4836–41.
Jarmalaviciute A, Tunaitis V, Pivoraite U, Venalis A, Pivoriunas A . Exosomes from dental pulp stem cells rescue human dopaminergic neurons from 6-hydroxy-dopamine-induced apoptosis. Cytotherapy 2015; 17: 932–9.
Ju GQ, Cheng J, Zhong L, Wu S, Zou XY, Zhang GY, et al. Microvesicles derived from human umbilical cord mesenchymal stem cells facilitate tubular epithelial cell dedifferentiation and growth via hepatocyte growth factor induction. PLoS One 2015; 10: e0121534.
Choi HY, Lee HG, Kim BS, Ahn SH, Jung A, Lee M, et al. Mesenchymal stem cell-derived microparticles ameliorate peritubular capillary rarefaction via inhibition of endothelial-mesenchymal transition and decrease tubulointerstitial fibrosis in unilateral ureteral obstruction. Stem Cell Res Ther 2015; 6: 18.
Lozito TP, Tuan RS . Endothelial and cancer cells interact with mesenchymal stem cells via both microparticles and secreted factors. J Cell Mol Med 2014; 18: 2372–84.
Berezin AE, Kremzer AA, Samura TA, Martovitskaya YV, Malinovskiy YV, Oleshko SV, et al. Predictive value of apoptotic microparticles to mononuclear progenitor cells ratio in advanced chronic heart failure patients. J Cardiol 2015; 65: 403–11.
Acknowledgements
This work was supported by the Tianjin Science and Technology Project of China (No 13ZCZDSY01500) and the National Natural Science Foundation of China (No 81370422 and No 81700846).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Zhang, W., Chen, S. & Liu, ML. Pathogenic roles of microvesicles in diabetic retinopathy. Acta Pharmacol Sin 39, 1–11 (2018). https://doi.org/10.1038/aps.2017.77
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2017.77
Keywords
This article is cited by
-
Petrogenesis of Early Cretaceous volcanic rocks in the southeastern margin of the Songliao Basin, NE China: implications for the geodynamic evolution of Paleo-Pacific Ocean
International Journal of Earth Sciences (2024)
-
Endothelial progenitor cells as biomarkers of diabetes-related cardiovascular complications
Stem Cell Research & Therapy (2023)
-
Therapeutic effects of mesenchymal stem cells-derived extracellular vesicles’ miRNAs on retinal regeneration: a review
Stem Cell Research & Therapy (2021)
-
Hepatitis C virus nonstructural protein 5A perturbs lipid metabolism by modulating AMPK/SREBP-1c signaling
Lipids in Health and Disease (2019)
-
Prostaglandin E2/EP2 receptor signalling pathway promotes diabetic retinopathy in a rat model of diabetes
Diabetologia (2019)