Abstract
Caspofungin is an echinocandin antifungal agent licensed as a first-line therapy for invasive candidiasis in patients with moderate to severe illness or recent exposure to azoles. In this study we developed a whole-body physiology-based pharmacokinetics (WB-PBPK) model to predict the pharmacokinetics (PK) of caspofungin, and combined with Monte Carlo simulation (MCS) to optimize clinical dosage regimens of caspofungin in different kinds of patients. A WB-PBPK model of caspofungin was built and validated with raw data from 4 previous trials of general patients, intensive care unit (ICU) patients with Child-Pugh B, ICU patients on continuous renal replacement therapy, mild and moderate hepatic insuffciency (HI) patients. MCS was used to optimize clinical dosage regimens of caspofungin in these patients. A cumulative fraction of response (CFR) value of ≥90% was considered to be the minimum for achieving optimal empirical therapy. The simulated results of the WB-PBPK model were in good agreement with observed values of all trials. For general and ICU patients with caspofungin 70/50 mg, AUC and Cmax were decreased with the increase of body weight (BW) and showed great variation. MCS showed all general patients achieved CFR≥90% regardless of BW. But not all ICU patients with higher BW (≥70 kg) could achieve CFR≥90%. Compared with standard dosage regimens in general patients, caspofungin 70/35 mg in ICU patients with Child-Pugh B achieved significantly decreased AUC and Cmax, but obtained similar AUC and Cmax in moderate HI patients with Child-Pugh B. The WB-PBPK model of caspofungin is able to predict PK of all populations correctly. The combined WB-PBPK model with MCS can successfully optimize clinical dosage regimens of caspofungin in all patient populations.
Similar content being viewed by others
Introduction
Caspofungin is an echinocandin antifungal agent licensed as a first-line therapy for invasive candidiasis in patients with moderate to severe illness or recent exposure to azoles1. The recommended dosage regimen of caspofungin is a loading dose of 70 mg followed by 50 mg daily (70/50 mg), administered intravenously over 1 h. Caspofungin is highly protein bound (96%) and metabolizes slowly in the liver2,3,4. Its liver uptake is a biphasic process and its binding to the surface of hepatocytes is fast and reversible. Studies demonstrated that the uptake of caspofungin by liver is related to the active organic anion transporting polypeptide 1B1 (OATP1B1)5. The plasma clearance (CL) of caspofungin is 10 to 12 mL/min2 It is eliminated mainly by hepatic, for only one to two percent of the antifungal agent is through renal clearance6. The elimination of caspofungin from plasma is slow and the half-life of caspofungin is 9–11 h2.
Clinically, pharmacokinetics (PK) parameters in intensive care unit (ICU) patients are often different from those in healthy subjects7. Factors associated with alterations in PK include changes in organ function, use of extracorporeal clearance techniques and drug interactions8,9. It was also reported that caspofungin plasma concentrations were influenced by hypoalbuminaemia and hepatic impairment (HI)7. One study demonstrated that caspofungin trough plasma concentrations (C min) ranges were relatively wide in surgical ICU patients and influenced by protein binding7. Another study showed that caspofungin area under the curve (AUC) was increased by 55% and 76% in patients with mild and moderate HI, respectively4,10. But at present, data are very limited and absent on these special patients, an increase in knowledge on these patients should be considered. Clinically, patients weighing >80 kg are advised to receive a dosage regimen of 70/70 mg11. But studies of general ICU population and hematopoietic stem cell transplantation patients found that body weight (BW) (range 50–99 kg) had no effect on caspofungin PK9,12. Whether age and race could influence the PK of caspofungin is not clear. On the other hand, one study demonstrated that the vast majority of fungal infections are caused by Candida spp9. In the critically ill, the infections of invasive Candida spp. are associated with high crude and attributable mortalities as high as 60% and 40%, respectively13. One multicentre observational study in Spain had carried out that mortality was associated with age, Candida spp., different from C. parapsilosis and inadequate treatment14. All of these ask for a model which could predict the PK of caspofungin in different populations (general patients, ICU patients and HI patients) with different physical conditions, BW, age, race, Candida spp. And based on the PK parameters, a Monte Carlo simulation (MCS) could be used to optimize the clinical dosage regimens of caspofungin in different patient populations.
Whole-body physiology-based PK (WB-PBPK) modellings consider the physical and chemical characteristics of a drug and it also give thorough consideration of physiological processes of drug absorption, distribution, metabolism and elimination accurately15. Based on a series of parameters, such as physiological and physicochemical properties, CL, distribution into tissues and metabolism or active transport, WB-PBPK could predicts PK of a drug15. Then based on a series of equations, we can develop a WB-PBPK model which could be applied to forecast disease dependencies7,9, BW, age, and race can also be used to investigate the variability expected in different patient populations6,12.
The aim of the present study was to build and verify a WB-PBPK model which could predict the PK of caspofungin in general patients, ICU patients with Child-Pugh B, ICU patients on continuous renal replacement therapy (CRRT) and HI patients, then to evaluate the impact on the PK of caspofungin between different individuals through stochastic simulations of different body weight, age and race using the validated WB-PBPK model. Finally, combined with MCS technique to help in the selection of a safe and effective administration scheme after simulation of the potential exposure and disposition in different patient populations.
Materials and methods
PK data
Clinical PK data for intravenous administration of caspofungin in healthy adults and all patients were obtained from the literature4,9,10,16,17. Raw data of 20 healthy subjects, receiving single intravenous doses of 20 mg, 40 mg, 70 mg, 100 mg, respectively, were used for model development. The mean age was 29 years (range, 21–39 years) and the mean weight was 75 kg (range, 60–88 kg). The observed mean concentrations of caspofungin over time were from the literature4. Mean concentrations of caspofungin over time from a double-blind, placebo-controlled, serial-panel study of 24 healthy male subjects to investigate the pharmacokinetics of caspofungin following daily doses of 15, 35, or 70 mg were used to validate the model4. Another trial of caspofungin in healthy subjects studied the standard dosage regimen of 70/50 mg10. Plasma drug profiles defined by concentrations at 0 h (predose) and at 0.5, 0.75, 1, 1.25, 1.5, 2, 4, 8, 12, and 24 h postdose were obtained on days 1 and 14. Intervening trough (24-h postdose) concentrations (C min) were obtained prior to dosing on d 3, 4, 7, and 104. The relevant data are shown in Table 1.
To develop and qualify the WB-PBPK model in general patients16, ICU patients with Child-Pugh B9 and ICU patients on CRRT17, HI patients10, raw data from 4 clinical trials were used. The study description, population included, treatment schedule, doses and sampling scheme are shown in Table 1. The study of general patients was a formal phase II dose escalation trial in patients with invasive aspergillosis. Caspofungin was administered once daily as an iv infusion over 120 min at 70 mg (9 patients), 100 mg (8 patients), 150 mg (9 patients) and 200 mg (20 patients). Pharmacokinetic sampling was performed serially on d 1 (2, 3, 5–7 and 24 h after the infusion started) and peak (at the end of infusion) and trough levels (immediately before the next infusion started) were collected on d 4, 7, 14 and 28. All observed data from pharmacokinetic sampling were pooled as mean±standard deviation16. Depending on the WB-PBPK model, we studied the recommended dosage regimens (70/50 mg in ICU patients, mild HI; 70/35 mg in moderate HI patients) of caspofungin9,10,17. To evaluate the model, we collected 508 trough concentrations from 161 patients (39 ICU patients with Child-Pugh B, 16 ICU patients on CRRT, 47 moderate HI patients and 68 mild HI patients) of the First Affiliated Hospital of Xi'an Jiaotong University. The pharmacokinetic sampling were pooled as mean± standard deviation in ICU patients and HI patients. The study was approved by the Ethics Committee of the First Affiliated Hospital of Xi'an Jiaotong University. All subjects signed the informed consent before any screening item being performed.
Model development
The WB-PBPK model of caspofungin, which was built by GastroPlus version 9.0 (Simulations Plus, USA), was used for all of the simulations in healthy subjects. The WB-PBPK (disposition) model was composed of a number of tissue compartments which were linked together by venous and arterial blood circulation. These compartments include the heart, lung, brain, adipose, muscle, skin, liver, kidney, and so on. The drug distribution into different compartments was driven by perfusion-limited kinetics for all of the tissues were considered to be well-stirred compartments. Each compartment was defined by an associated tissue blood flow rate, volume and a tissue to-plasma partition coefficient. We used the built-in mass balance differential equations to develop the model18.
Vital physicochemical parameters and the key vitro data for caspofungin are depicted in Table 2. The pK a, Rbp, solubility-pH, effective permeability and particle size were obtained using the ADMET PredictorTM module of GastroPlus. Human logP, fup (plasma unbound drug) was obtained from the related literature19,20. The tissue-to-plasma partition coefficients of caspofungin were calculated using established tissue-composition based models. Total plasma CL of caspofungin was calculated by the PKplus model of the GastroPlus version 9.0 (Table 3). The results of non-compartment model will be used to develop the WB-PBPK model. The main elimination route of caspofungin is hepatic (98%) and only two percent of caspofungin is through renal clearance. So the CL data of liver and renal used in the model will based on this. The simulation time was 144 h and the volume of dosage administration was 250 mL.
PK simulations
Based on the raw data from 4 clinical trials, we developed and qualified the WB-PBPK model in general patients, ICU patients with Child-Pugh B and ICU patients on CRRT and HI patients. The study description, population included, treatment schedule, doses and sampling scheme were recorded and used in the development and verification of the WB-PBPK models. Total plasma CL from different populations were calculated by the PKplus model of the GastroPlus version 9.0 (Table 3). The results of non-compartment model were used to develop the WB-PBPK model. The simulation time were 14 d and the volume of dosage administration were 250 mL.
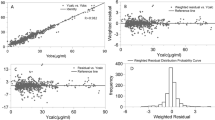
Model evaluation
To evaluate the WB-PBPK models, a visual comparison between the predicted data of GastroPlus version 9.0 and the observed data (literature resources and our research data) of the different trials from different populations was carried out. Goodness of fit (GOF) plots were performed to analyze the accuracy between simulated and observed data. The prediction error (PE) was estimated according to Eq. 119.
PE=(simulated-observed)/observed×100 (Eq.1)
The fold-error, which represents the difference between observed and predicted in vivo values, was used to assess the accuracy of the predicted PK parameters, and if the fold-error was less than two, the prediction was considered successful21,22.
Fold-error=observed/predicted (observed value > predicted value) (Eq.2)
Fold-error=predicted/observed (observed value < predicted value) (Eq.3)
Model application
Virtual trial simulations
For general and ICU patients, we simulated the recommended dosage regimens (70/50 mg) of caspofungin. On the other hand, other two multiple dosage regimens (70/35 mg, 70/70 mg, 100/100 mg) of caspofungin were simulated to investigate the effects of different dosage regimens of caspofungin in these patients.
For HI patients, except the recommended dosage regimens (70/35 mg for moderate HI patients, 70/50 mg for mild HI patients), dose reduction of 50/25 mg and dose escalating of 70/70 mg, 100/100 mg were simulated using the WB-PBPK model.
PK variability of varying body size of the recommended dosage regimens of caspofungin in general patients, ICU and HI patients were assessed by creating virtual populations weighing 40–100 kg. Virtual ages of 18–95 years were simulated in these patients, too. What's more, different race groups, representatives of Asian and Westerner were simulated. Based on the WB-PBPK model, we could obtain the PK parameters including peak plasma concentrations (C max), C min, AUC and CL of these patients under different weight conditions.
Dosage optimization
To describe caspofungin pharmacokinetic/pharmacodynamics (PK/PD) adequacy for the treatment of invasive Candida spp. and determine whether the different dosage regimens of caspofungin could achieve PK/PD targets in the general patient populations, ICU and HI patients. A MCS method was performed using the simulated data of WB-PBPK model. Through virtual simulation of Gastroplus, we obtained the AUC of different dosage regimens of these special patients. The MCS methods, the pharmacodynamic targets for Candida species (fAUC0-24/MIC ratio for C. albicans, C. glabrata and C. parapsilosis) and the minimum inhibitory concentration distributions for Candida species have been described previously23. The optimal dosage regimens were evaluated to compare the simulated probability of target attainment (PTA) and cumulative fraction of response (CFR) in these subjects. A CFR value of ≥ 90% was considered to be an appropriate empirical dosage regimen.
Results
Caspofungin PK
The WB-PBPK model for caspofungin was established according to the scheme of relevant tissue compartments of the disposition model. Simulations were conducted based on the physicochemical and in vitro data of caspofungin (Table 2). Hepatic and renal caspofungin CL (Table 3) were calculated by the PKplus model, as described in the method section.
The observed (literate resources data) and mean simulated plasma concentration-time profiles of caspofungin in healthy subjects are vividly presented in Figure 1. The accuracy of the predictions are summarized in Table 3. The predicted PK parameters were nearly consistent (<2-fold error) with the observed values (literate resources data). Accurately, using the in silico data, in vitro data, WB-PBPK model could simulate the plasma concentration-time profile following intravenous administration and predicted CL as inputs to the model, as shown in Figure 1 and Table 3.
Simulated (line) and observed4(square) plasma concentration-time profiles of caspofungin after 20 mg (A), 40 mg (B), 70 mg (C) and 100 mg (D) single dose intravenous administration in healthy subjects.
Data verification
The established WB-PBPK model of caspofungin could predict the observed concentration-time profile (literate resources data) for all dose groups of different populations accurately (Figures 1, 2, 3, Supplementary Figure 1). For all doses levels, the simulated peak concentrations seem to be underrated by 20% but they were within the error range. As shown in Supplementary Figure 1, the predicted concentration-time-curve was in accordance with the observed mean values (literate resources data) of healthy subjects with the multiple doses administration of 15/15 mg, 35/35 mg, 70/50 mg and 70/70 mg, which is the same to general patients with the dosage regimens of 70/70 mg, 100/100 mg, 150/150 mg and 200/200 mg (Figure 2). According to the GOF plot, we could see a good accuracy between predicted and observed data (literate resources data, Supplementary Figure 2A–B). Only the simulated peak concentrations were undervalued in Gastroplus. For ICU patients with Child-Pugh B, ICU patients on CRRT and HI patients, when using the WB-PBPK distribution model to simulate plasma concentrations, a reasonable match to the measured concentration range was observed (Figure 3). The GOF plot showed a good accuracy between predicted and observed data (literate resources data, Supplementary Figure 2C–D). The simulated peak levels seemed to be underestimated by 10%, which were within the error range. The simulated trough levels seemed to be underestimated by 10% in ICU patients with Child Pugh B and 5% in ICU patients on CRRT and mild HI patients compared with the observed data (literate resources and our research data), for moderate HI patients, it showed a sufficient accuracy between predicted and observed data. The CL, V ss, t 1/2, AUC, C max of different patients with different dosage regimens are shown in Table 3. The fold-error of all dosage regimens were less than 2.
Simulated and mean observed (symbol±SD)16 plasma concentration-time profiles of caspofungin after 70/70 mg (A), 100/100 mg (B), 150/150 mg (C) and 200/200 mg (D)16 intravenous multiple doses in general patients. A solid thick line adjacent to the middle of the concentration-time profile represents the mean of the predictive values. Solid squares represent the observed clinical concentration-time data16. The shaded area represents the 90% confidence interval for the simulated data, and the thin lines on either hand represent individual simulated results of the 100% range of simulated individual data.
Simulated and mean observed (symbol ± SD) plasma concentration-time profiles of caspofungin after the recommended intravenous multiple doses in ICU patients with Child-Pugh B(A)9, ICU patients on continuous renal replacement therapy (CRRT) (B)17, moderate (C) and mild HI patients (D)10. A solid thick line adjacent to the middle of the concentration-time profile represents the mean of the predictive values. Solid squares represent the observed clinical concentration-time data9,17,10, and solid circles represent our data of trough concentrations (mean±SD). The shaded area represents the 90% confidence interval for the simulated data, and the thin lines on either hand represent individual simulated results of the 100% range of simulated individual data.
Virtual trial simulations
PK parameters of general patients and ICU patients are shown in Table 3. Particularly, the PK parameters of ICU patients were recorded. At steady state, the AUC of 70/35 mg, 70/70 mg, 100/100 mg of caspofungin in ICU patients were 74.5 mg·h/L, 155.5 mg·h/L, 218.4 mg·h/L, respectively. The AUC of moderate HI patients were 92.6 mg·h/L, 178.6 mg·h/L, 280 mg·h/L after simulation of the reduction dose of 50/25 mg and dose escalating of 70/70 mg, 100/100 mg.
Supplementary Figure 3A, 3B and 3C showed the relationship between C max, C min, AUC, CL and BW with caspofungin 70/50 mg in general patients and ICU patients and 70/35 mg in moderate HI patients, respectively. We find that C min were constant in all investigated virtual patients and did not correlate to BW or other covariates. This was also valid for the CL. But C max and AUC began a slow decline with the increase of body weight. The variation tendency was not obvious in HI patients.
As shown in Supplementary Figure 3D, patients with different ages showed no statistical difference in PK parameters. Compared with Westerner, C max in Asian showed a slight increase and C min showed a slight decrease in all of these general patients, ICU patients and HI patients (Supplementary Figure 4).
Optimization of the clinical dosage regimens
The WB-PBPK model coupled with a MCS showed the currently recommended dosage regimens of caspofungin in all patients achieved CFR ≥ 90% for C. albicans and C. glabrata, but achieved CFR ≤ 65% for C. parapsilosis, a maintenance dose of 100/100 mg in ICU and mild HI patients and 70/70 mg in moderate HI patients achieved CFR ≥ 90% for C. parapsilosis (Figure 4 and Table 4).
Figure 4a were PTA for C.albicans, C.glabrata, C.parapsilosis of the recommended dosage regimens of caspofungin in general patients, intensive care unit (ICU) patients (including ICU patients on CRRT and ICU patients with Child-Pugh B), mild hepatic insufficiency (HI) and moderate HI patients. The recommended dosage regimens of caspofungin for general patients (solid circles), ICU patients (hollow circles) and mild HI patients (solid triangles) were 70/50 mg, and for moderate HI patients (hollow squares), the recommended dosage regimen was 70/50 mg. Figure 4b were PTA for C. albicans, C. glabrata, C. parapsilosis of the adjustive dosage regimens of caspofungin in general patients (100/100 mg, solid circles), ICU patients (100/100 mg, hollow circles), ICU patients with Child-Pugh B (70/35 mg, downward hollow triangles), mild HI (100/100 mg, upward solid triangles) and moderate HI (70/70 mg, hollow squares; 50/25 mg, a circle with a fork in it) patients. The pharmacodynamic index was fAUC/MIC.
Disscussion
Drug research based on the mathematical models becomes extremely important for the optimization of clinical dosage regimens in special populations, mostly by providing reasonable dose selection method and thereby offer a reliable way to evaluate the risks and benefits. At present, WB-PBPK models have been used for prediction of the pharmacokinetics in special populations for their strength in data integration and delivery of mechanistic insights and superior predictive power24. These models could explain phenomenons from the perspective of mathematical model principles and can be applied to forecast disease dependencies and can also be used to investigate the variability expected in different patient populations24. Based on the WB-PBPK models, this investigation focus on the influence of disease state on the PK of caspofungin. But most importantly, the study makes innovation in combining WB-PBPK model with MCS to optimize the clinical dosage regimens in special patients.
This article first describes the use of WB-PBPK modelling to assist research and clinical study of PK of caspofungin in ICU patients and HI patients. The approach which integrated drug-specific parameters such as logP, pK a, solubility and permeability and in vitro data such as plasma protein binding and blood-to-plasma concentration ratio was able to simulate the pharmacokinetics of caspofungin across multiple dose levels in different human populations with suitable accuracy. The methodology also provided a reliable way to understand the mechanisms underlying the pharmacokinetic processes of caspofungin considering the influence of weight, age and race. Based on the changes of caspofungin pharmacokinetic parameters and combined with MCS, an optimization of dosage regimens was developed in these special patients.
After WB-PBPK simulation, we find that for ICU patients on CRRT, the PK parameters from the WB-PBPK simulation were in good agreement with those of the observed (our research data). When combined with MCS method, the recommended dosage regimen (70/50 mg) is appropriate in these patients. But caspofungin maintenance dose should not be reduced to 35 mg in ICU patients with Child-Pugh B which based on the Child-Pugh score if this classification is driven by hypoalbuminemia as it results in significantly lower exposure. A dosage reduction to 35 mg daily following the 70 mg loading dose is reasonable for moderate HI patients with Child-Pugh score B. If the maintenance dose was reduced to 25 mg/d, C max will decrease (Mean: 5.5 mg/L, data were from the model simulation), which would affect the therapeutic effect of caspofungin. On the other hand, a maintenance dose increased to 50 mg/d will lead to a higher C min of 4.2 mg/L (data were from the model simulation), which would induce adverse reactions during the period of treatment.
With the increase of BW, PK of echinocandins might be altered due to changes in volume of distribution and/or CL. Studies have shown that PK in obese patients might be altered due to a change of more fat tissue in relation to BW, change in liver metabolism and an increase in CL, and change in plasma protein constituents should also be considered25,26,27. Clinically, PK data of echinocandins in obese patients are scarce. One study demonstrated that patients weighing >80 kg are advised to receive caspofungin 70/70 mg28. In surgical ICU patients, weighing >75 kg were advised to receive a dosage regimen of 70/70 mg for lower C min (decreased by 28%) were predicted in these patients7. But in general ICU populations and hematopoietic stem cell transplantation patients (BW: range 50–99 kg) were discovered have no effect on caspofungin PK9,12. With the WB-PBPK simulation, our study demonstrated that general and ICU patients weighing >70 kg are advised to receive 70/70 mg. But no dose adjustment is needed for mild and moderate HI patients weighing >70 kg for the recommended dosage regimens (70/50 mg for mild HI patients and 70/35 mg for moderate HI patients) could achieve CFR ≥ 90% for most Candida spp., such as C. albicans and C. glabrata. For adult patients, age has no effect on the PK of all these patients, there is also no need for dose adjustment in old patients. Compared with Westerners, C max in Japanese showed a slight increase and C min showed a slight decrease in all of these general patients, ICU patients and HI patients (Supplementary Figure 4). But no dose adjustment is needed.
WB-PBPK model coupled with MCS showed that the current recommended dosage regimens of caspofungin in all patients achieved CFR ≥ 90% for C. albicans and C. glabrata, but achieved CFR ≤ 65% for C. parapsilosis. The dosage regimens of 100/100 mg in ICU and mild HI patients and 70/70 mg in moderate HI patients achieved CFR ≥ 90% (Figure 4). So for C. albicans and C. glabrata in all patients, the recommended dosage regimens are reasonable. For C. parapsilosis, dosage regimens of 100/100 mg in ICU and mild HI patients and 70/70 mg in moderate HI patients are needed.
Assignment of metabolism to transporters in the model is not considered in this paper but would be necessary for more detailed conclusions about the sources of variability in caspofungin PK. This would also require careful consideration of the demographics of the studied population and of other sources of variability. One study demonstrated that the intake approach of caspofungin into the liver is a biphasic process with a fast, reversible binding to the surface of hepatocytes and a slow transport through the active OATP1B15. Clinically, effective and reliable data on transporters and enzymes from in vitro experiments are needed in WB-PBPK models29, but we did not obtain utilizable K M and V max values of OATP1B1 for the transport of caspofungin in the literature. So data of V max and K M in vitro is urgently needed to refine the WB-PBPK model of caspofungin. Another limitation of this study is that the data for the model verification were almost from the literate resources and we acquired them from the manuscripts, but not given by the original authors. In order to make up for the defects, we collected 508 trough concentrations from 161 patients (39 ICU patients with Child-Pugh B, 16 ICU patients on CRRT, 47 moderate HI patients and 68 mild HI patients) to evaluate the model and found that they all showed sufficient accuracy between predicted and observed data.
Conclusion
In conclusion, a WB-PBPK model for caspofungin was developed and qualified in diverse adult population groups. The model successfully predicted the intravenous and PK of caspofungin across multiple dose levels in normal human populations and special patients. This represents a case study that highlights the prospective applications of the WB-PBPK model combined with the MCS to provide clinical PK predictions and optimize the clinical dosage regimens. PK of caspofungin can be obtained before proceeding with clinical studies. Clinically, when BW is higher than 70 kg in ICU patients, an increasing maintenance dose of 70 mg every day should be considered in humans at lower exposures. Dose reduction of caspofungin in ICU Patients with Child Pugh B will result in suboptimal exposure. In the future, combined with other methods, the model could be used as a basis for further clinical investigations to enable a priori adjustment of drug dosing for maximal efficacy and minimal toxicity.
Author contribution
Ya-lin DONG designed the study and edited the manuscript; Qian-ting YANG contributed to the analysis, interpretation, manuscript writing, and final approval of the manuscript; Ya-jing ZHAI contributed to the conception and design, analysis, interpretation, manuscript writing, and final approval of the manuscript; Lu CHEN contributed to the data collection, analysis, interpretation, manuscript writing, and final approval of the manuscript; Tao ZHANG, Yan YAN, Ti MENG, Lei-chao LIU, Li-mei CHEN, Xue WANG contributed to the conception and design, data collection, interpretation, manuscript writing, and final approval of the manuscript; All authors read and approved the final manuscript.
References
Pappas PG, Kauffman CA, Andes D, Benjamin DK, Calandra TF, Edwards JE, et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis 2009; 48: 503–35.
Kofla G, Ruhnke M. Pharmacology and metabolism of anidulfungin, caspofungin and micafungin in the treatment of invasive candidosis: review of the literature. Eur J Med Res 2011; 16: 159–66.
Walsh TJ, Adamson PC, Seibel NL, Flynn PM, Neely MN, Schwartz C, et al. Pharmacokinetics, safety, and tolerability of caspofungin in children and adolescents. Antimicrob Agents Chemother 2005; 49: 4536–45.
Stone JA, Holland SD, Wickersham PJ, Sterrett A, Schwartz M, Bonfiglio C, et al. Single- and multiple-dose pharmacokinetics of caspofungin in healthy men. Antimicrob Agents Chemother 2002; 46: 739–45.
Sandhu P, Lee W, Xu X, Leake BF, Yamazaki M, Stone JA, et al. Hepatic uptake of the novel antifungal agent caspofungin. Drug Metab Dispos 2005; 33: 676–82.
Balani SK, Xu X, Arison BH, Silva MV, Gries A, DeLuna FA, et al. Metabolites of caspofungin acetate, a potent antifungal agent, in human plasma and urine. Drug Metab Dispos 2000; 28: 1274–8.
Nguyen TH, Hoppe-Tichy T, Geiss HK, Rastall AC, Swoboda S, Schmidt J, et al. Factors influencing caspofungin plasma concentrations in patients of a surgical intensive care unit. J Antimicrob Chemother 2007; 60: 100–6.
Smith BS, Yogaratnam D, Levasseur-Franklin KE, Forni A, Fong J. Introduction to drug pharmacokinetics in the critically ill patient. Chest 2012; 141: 1327–36.
Muilwijk EW, Schouten JA, Leeuwen HJ, Zanten AR, Lange DW, Colbers A, et al. Pharmacokinetics of caspofungin in ICU patients. J Antimicrob Chemother 2014; 69: 3294–9.
Mistry GC, Migoya E, Deutsch PJ, Winchell G, Hesney M, Li S, et al. Single- and multiple-dose administration of caspofungin in patients with hepatic insufficiency: implications for safety and dosing recommendations. J Clin Pharmacol 2007; 47: 951–61.
Muilwijk EW, Lempers VJ, Burger DM, Warris A, Pickkers P, Aarnoutse RE, et al. Impact of special patient populations on the pharmacokinetics of echinocandins. Expert Rev Anti Infect Ther 2015; 13: 799–815.
Wurthwein G, Young C, Lanvers-Kaminsky C, Hempel G, Trame MN, Schwerdtfeger R, et al. Population pharmacokinetics of liposomal amphotericin B and caspofungin in allogeneic hematopoietic stem cell recipients. Antimicrob Agents Chemother 2012; 56: 536–43.
Sinnollareddy MG, Roberts JA, Lipman J, Akova M, Bassetti M, De Waele JJ, et al. Pharmacokinetic variability and exposures of fluconazole, anidulafungin, and caspofungin in intensive care unit patients: Data from multinational Defining Antibiotic Levels in Intensive care unit (DALI) patients Study. Crit Care 2015; 19: 33.
Rodriguez-Hernandez MJ, Ruiz-Perez de Pipaon M, Marquez-Solero M, Martin-Rico P, Caston-Osorio JJ, Guerrero-Sanchez FM, et al. [Candidemias: multicentre analysis in 16 hospitals in Andalusia (Spain)]. Enferm Infecc Microbiol Clin 2011; 29: 328–33.
Schmitt W, Willmann S. Physiology-based pharmacokinetic modeling: ready to be used. Drug Discov Today Technol 2004; 1: 449–56.
Wurthwein G, Cornely OA, Trame MN, Vehreschild JJ, Vehreschild MJGT, Farowski F, et al. Population pharmacokinetics of escalating doses of caspofungin in a phase II study of patients with invasive aspergillosis. Antimicrob Agents Chemother 2013; 57: 1664–71.
Weiler S, Seger C, Pfisterer H, Stienecke E, Stippler F, Welte R, et al. Pharmacokinetics of caspofungin in critically ill patients on continuous renal replacement therapy. Antimicrob Agents Chemother 2013; 57: 4053–7.
Jones HM, Dickins M, Youdim K, Gosset JR, Attkins NJ, Hay TL, et al. Application of PBPK modelling in drug discovery and development at Pfizer. Xenobiotica 2012; 42: 94–106.
Stader F, Wuerthwein G, Groll AH, Vehreschild JJ, Cornely OA, Hempel G. Physiology-based pharmacokinetics of caspofungin for adults and paediatrics. Pharm Res 2015; 32: 2029–37.
Andes D, Diekema DJ, Pfaller MA, Bohrmuller J, Marchillo K, Lepak A. In vivo comparison of the pharmacodynamic targets for echinocandin drugs against Candida species. Antimicrob Agents Chemother 2010; 54: 2497–506.
Jones HM, Parrott N, Jorga K, Lave T. A novel strategy for physiologically based predictions of human pharmacokinetics. Clin Pharmacokinet 2006; 45: 511–42.
Parrott N, Paquereau N, Coassolo P, Lave T. An evaluation of the utility of physiologically based models of pharmacokinetics in early drug discovery. J Pharm Sci 2005; 94: 2327–43.
Yang Q, Wang T, Xie J, Wang Y, Zheng X, Chen L, et al. Pharmacokinetic/ pharmacodynamic adequacy of echinocandins against Candida spp in intensive care unit patients and general patient populations. Int J Antimicrob Agents 2016; 47: 397–402.
Strougo A, Yassen A, Krauwinkel W, Danhof M, Freijer J. A semiphysiological population model for prediction of the pharmacokinetics of drugs under liver and renal disease conditions. Drug Metab Dispos 2011; 39: 1278–87.
Brill MJ, Diepstraten J, Rongen A, Kralingen S, Anker JN, Knibbe CA. Impact of obesity on drug metabolism and elimination in adults and children. Clin Pharmacokinet 2012; 51: 277–304.
Jain R, Chung SM, Jain L, Khurana M, Lau SW, Lee JE, et al. Implications of obesity for drug therapy: limitations and challenges. Clin Pharmacol Ther 2011; 90: 77–89.
Knibbe CA, Brill MJ, Rongen A, Diepstraten J, Graaf PH, Danhof M. Drug disposition in obesity: toward evidence-based dosing. Annu Rev Pharmacol Toxicol 2015; 55: 149–67.
Vorwerk CK, Tuchen S, Streit F, Binder L, Hofmuller W, Behrens-Baumann W. Aqueous humor concentrations of topically administered caspofungin in rabbits. Ophthalmic Res 2009; 41: 102–5.
Edginton AN, Theil FP, Schmitt W, Willmann S. Whole body physiologically-based pharmacokinetic models: their use in clinical drug development. Expert Opin Drug Metab Toxicol 2008; 4: 1143–52.
Acknowledgements
The authors gratefully thank Tangdu Hospital of Fourth Medical University for outstanding assistance in the software support (Gastroplus 9.0).
This work is supported by the National Natural Science Foundation of China (No 81473177 and 81672954) and the Shaanxi Provincial Natural Science Foundation (No 2016JM8015).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Supplementary Information
Supplementary Figures
Rights and permissions
About this article
Cite this article
Yang, Qt., Zhai, Yj., Chen, L. et al. Whole-body physiology-based pharmacokinetics of caspofungin for general patients, intensive care unit patients and hepatic insufficiency patients. Acta Pharmacol Sin 39, 1533–1543 (2018). https://doi.org/10.1038/aps.2017.176
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2017.176
Keywords
This article is cited by
-
Administration and Dosing of Systemic Antifungal Agents in Pediatric Patients
Pediatric Drugs (2020)