Key Points
-
Describes the distinction between success and survival of dental implants.
-
Outlines factors which contribute to failure.
-
Discusses considerations for informed consent throughout the implant placement and restoration process.
Abstract
The use of dental implants to restore edentulous areas has increased significantly since the 1970s and is now considered, by many, the gold standard restorative treatment. As such it has become increasingly important to understand what constitutes success for these rehabilitations. Increasing focus has been given to acknowledging the difference between success and survival: the two being potentially very different outcomes for such invasive and expensive treatment. This article aims to describe this distinction and ultimately the implications of this for both patient and clinician.
Similar content being viewed by others
Introduction
The limitations and biological collateral damage of conventional methods of replacing missing teeth are well documented.1,2,3 As such there has been an ever-increasing focus on the use of dental implants as a solution to restore edentulous sites. Dental implants are inert, alloplastic materials embedded in the alveolar bone for the management of tooth loss and to aid replacement of lost oro-facial structures. Since the first iterations of the original Branemark implant in 1965,4 many designs and materials have been used for implantation into the bone of the maxilla or mandible in order to support a prosthesis. Through trial and error, the current gold standard is titanium, root-form implants which provide a biocompatible environment for 'osseointegration' and predictable stability when functionally loaded.5,6 Further research has shown that dental implants have very good prognoses long term and are a viable option for definitive tooth replacement.7,8
The success of dental implants as a treatment modality has led to a large media focus on implants as the 'ideal' replacement for teeth and as a solution to failed dental treatment or poorly fitting prostheses. An estimated five million endosseous implants were placed in the USA in 2010 with estimated market sales of $10 billion of implant related materials.9 In the UK alone it is estimated 20 implants are placed per 10,000 of the population.9 With more patients demanding implant based therapy, it is becoming increasingly important to understand the limitations of treatment, to identify those patients for whom treatment is less likely to be successful and, ultimately, consent patients to the likely outcomes. More experienced clinicians may be able to offer their own personal success rates but many will have to revert to the published data to inform patients of the risks and likely outcomes of this invasive and invariably costly intervention.
The primary aim of this clinical review paper is to highlight the importance of differentiating success from survival in dental implantology. This distinction has profound implications for patients in their understanding of the benefits and risks of this costly and invasive procedure. The secondary aim is to address those factors that the literature has identified to be associated with complications and failure of implant-based rehabilitation.
This is critical as it permits patient level risk assessment and ultimately informed consent consistent with the 'reasonable patient' test.
Historical parameters of success:
The definition of success has evolved since the first reports of osseointegration and the acceptance of dental implants as a predictable advance in oral rehabilitation. Initial descriptions of success were very much focused on the implant itself and any associated bone changes and/or mobility with no consideration of symptoms. In 1978 at a USA consensus conference, proposed success criteria stipulated no more bone loss than one third of the implant height and mobility of no greater than 1 mm in any direction. In 1979 Schnitman and Schulman10 expanded on this criteria and also included: functional service for 5 years in 75% of patients; gingival inflammation amenable to treatment; absence of symptoms and infection; absence of damage to adjacent teeth; and absence of paraesthesia or violation of adjacent structures.
The most widely accepted criteria of success followed in 19865 and was described by Albrektsson who discussed:
-
Lack of mobility
-
Less than 1.5 mm bone loss in the first year
-
No more than 0.2 mm of vertical bone loss annually thereafter
-
No radiographic evidence of peri-implant radiolucency
-
No radiographic evidence of violation of the mandibular canal
-
No history of pain, suppuration or paraesthesia
These criteria are valid when discussing the implant alone in the context of surgical placement and integration, however, they do not acknowledge prosthetic success or patient satisfaction.
Modern parameters of success
Since the initial description of implant success, it has become clear that the integration of the implant is only one part of the prosthetic process and that the implant-abutment-restoration complex should be viewed as a whole unit. In addition to discussing implant and restorative factors, patient satisfaction with function and aesthetics are becoming more common influences, as the focus of outcomes shifts from predictable osseointegration, as judged by clinicians, to achieving functional and natural-looking prostheses for replacement of the dentition as judged by patients (Fig. 1).7,8
A review in 20128 suggests that modern criteria used to evaluate success are peri-implant soft tissue, implant bone level, prosthesis and patient subjective evaluation. Further to this, Pjetursson et al., 20071 combine possible complications as 'biological' and 'technical'. Biological includes soft tissue problems such as peri-implant lesions and inflammation; bone changes as well as aesthetics. Technical failures include the fracture of porcelain or acrylic, or the loss of luting cement, retaining screws or matrices, as well as rare complications, such as the fracture of components (eg, screws, abutments, implants).
Differentiating success from survival in implantology
Reflecting the acceptance that the best outcome measures consider more than the integration of the implant, success could be redefined as an absence of complications at follow-up or only minimal problems which can be dealt with simply.5,7,8 'Survival' suggests that the implant plus prosthesis is still in situ and 'functioning' regardless of problems encountered in the follow-up time.
In the seminal outcome review Pjetursson et al., 20071 show that survival rates are generally good with over 95% at five years and estimates of almost 90% at ten years. Despite this they suggest that as many as 38.7% of fixed implant-supported prostheses suffered some type of biological or technical problem during an observation period over five years. Such a vast array of complications means that trials must have strictly defined measures of success. Even the smallest problems with implant-retained prostheses could deem a restoration 'unsuccessful', thus negatively affecting research figures; often trials quote both success and survival or just survival rates for this reason.
From a research perspective it is important to define the difference between success and survival to stimulate the profession to seek new techniques and materials to reduce the discrepancy. From the perspective of patients and practitioners, the distinction is important not only to understand the possible longevity of their treatment of choice, but also the likelihood of the need for maintenance or replacement of components. All patients must be consented to a lifetime of, potentially costly, maintenance. Table 1 shows this clear discrepancy between success and survival. The following sections will address in greater depth the biological and technical complications one may encounter following implant rehabilitation.
Biological complications: peri-implant disease
The surface of implants is designed to be micro and macro mechanically rough and thus, not only does plaque accumulate more readily, it is harder to remove. Furthermore, as the connective tissue attachment around the necks of implants is circumferential, not embedded into the implant, bacteria may more readily penetrate along the length of the implant. Peri-implant disease is inflammation adjacent to an endosseous implant, in reaction to a bacterial biofilm on the surface of the implant. This has been categorised into peri-implant mucositis, where the mucosal cuff around the implant is reversibly affected in isolation or peri-implantitis, where there is loss of supporting bone.11,12 Associated signs of peri-implant mucositis include inflammation of the adjacent soft tissues, bleeding on probing and suppuration. Increased probing depth and radiographic evidence of bone loss adjacent to implants is indicative of peri-implantitis and in severe cases this may culminate in mobility and loss of the implant.
Studies suggest that as many as 56% of all implants will develop peri-implantitis.12 As discussed later, there are numerous risk factors which appear to increase prevalence and progression. Prevention is key, with oral hygiene measures and disruption of the biofilm by both patient at home and in-surgery cleaning with appropriate titanium instruments.
Once established, peri-implantitis is very hard to control (Fig. 2). Management strategies for peri-implantitis are centred around cumulative interceptive supportive therapy (CIST) as described by Lang et al. in 1997.13 This involves mechanical debridement, use of antiseptics and antibiotic treatment, and where necessary, regenerative or resective surgery (Fig. 3). Plaque control and non-surgical instrumentation is effective in the management of peri-implant mucositis, but this will not control peri-implantitis. In this case, surgical exploration and debridement must be considered (Fig. 4).11 When peri-implantitis causes severe bone loss and loss of support for restorations, explantation is often the ultimate treatment (Fig. 5). It is important to recognise that failure rate of reimplantation into the site of a failed implant is slightly higher, however, this can be modified by reducing risk factors where possible, and bone grafting procedures to replace lost bone.14
She presented in 2014 with pain from all her implants. There is loss of bone around the implants, profuse bleeding on probing, purulent exudate from all sites and severely compromised soft tissue aesthetics. Though the implant positioning and proximity to each other could be criticised, she has poor oral hygiene and is clearly susceptible to disease
Technical complications
This is defined as complications with any component of the implant or prosthesis. This includes fracture of implant, abutments or screws, fracture or chipping of restorative components and loss of lute or screw loosening (Fig. 6). However, implant fracture occurs in less than 1% of cases.15
The threaded part of the abutment was retained within the implant. If this could not be removed the implant would not be restorable. Disaster was averted with a screw removal instrument (Fig. 6c) used to back the screw out of the implant
Technical complications occur in 54.1% of all fixed implant-retained restorations.16 These are more common in screw-retained than cement-retained for fixed prostheses, with loosening of the abutment screw and chipping of porcelain the most common (Fig. 7). Incidence of technical complications is higher still in implant-retained overdentures compared to fixed reconstructions.17 Bar-retained dentures have been reported to need six hours of aftercare per patient over ten years.18 The most common complications are repair of the prosthesis or replacement of precision attachments (Fig. 8). Broken bars and ball attachments are rarely reported (Fig. 9).17
There was resultant trauma and inflammation of the adjacent soft tissues. Sometimes the cement lute can be broken with an instrument, the crown removed and the screw tightened or replaced. In this case the screw had to be accessed through the crown. This approach may also damage the underlying abutment potentially necessitating replacement of the whole prosthetic component
Though they can often be cold-cured back into the denture this can be fiddly and very frustrating for patients. Fig. 8b These gold leaf clips can deform and wear over time necessitating routine replacement
Replacement of these restorations is time consuming and expensive. Furthermore it is wholly dependent upon the clinicians ability to recognise the implant system and access components. This problem alone should encourage all implantologists to use systems that are recognised and evidence based with manufacturers committed to producing components long into the future
Although it may be possible to correct some technical complications relatively easily, many can be challenging, time consuming and expensive to manage. In some cases the only option may be the replacement of the prosthetic component and this can come at significant cost to both patient and dentist.
Aesthetic complications/compromises
Increasingly, aesthetics are a priority when restoring edentulous spaces. It is, therefore, important to assess the gingival biotype and gingival level, as well as resting lip and smile lines as up to 10% of the population will have a high lip line (Fig. 10).19 If aesthetics are compromised by recession or thin gingival biotype, treatment may be regarded as a failure by both clinician and patient and soft-tissue grafting should be considered at primary or uncovering surgery. Bony defects caused by resorption and implant-positioning errors can also affect appearance of definitive restorations (Fig. 11). Precise surgical planning should reduce this, however, if unavoidable, some restorative options are available such as angulation of abutments and the use of pink restorative materials (Fig. 12). Highlighting the aesthetic limitations of treatment early allows management of patients expectations accordingly.
This implant was placed using an immediate placement after extraction protocol in the 11 space. Surgical exploration reveals a complete absence of buccal plate. Immediately placed implants may integrate well but there is as yet poor long term data on other aspects of success such as soft tissue health
Quality of Life
When considering biological or technical complications, longevity of an implant depends on functionality, however, patient satisfaction is becoming more important in the evaluation of implant success and has been described in recent success criteria.8 Various focus groups and patient feedback assessments have deemed implant-supported prostheses, both fixed and removable, as viable restorative options with good perceived quality of life.20,21 Patients rarely experience prolonged discomfort and often report improved appearance, function and psychological confidence following implant treatment.
When comparing quality of life of implant-supported restorations with tooth-borne restorations, the literature shows no significant evidence to support choosing implants over conventional restorative options;20 however, when comparing with edentulousness the quality of life improves greatly.22 Indeed the placement of two mandibular implants to support and retain mandibular overdentures is now regarded as the gold standard treatment.23
Once it is accepted that there may be complications with implant therapy that may jeopardise the success of treatment, the sensible clinician must ask: are there any pre-operative factors that can help predict which cases will be successful and which may suffer complications or failure?
Predicting success
When making the decision to replace teeth with implant-supported restorations, patient selection is paramount for predictable implant osseointegration. There have been many papers that attempt to identify patients for whom the risk of failure or collateral damage is too great.24,25,26,27,28 Extrapolated from these, the following circumstances can be regarded as absolute contraindications:
-
Incomplete growth
-
Patients with an ASA class IV or V
-
Severe psychoses or psychological impairment that precludes informed consent and risks poor compliance with long term maintenance
-
Compromised bone that may result in significant pathological consequences, such as bone affected by severe osteoporosis, osteomalacia, malignancy, ORN, BRONJ or osteomyelitis
-
In severely atrophic mandibles where augmentation is not possible and placement carries a significant risk of pathological fracture
-
Uncontrollable blood dyscrasias, including bleeding disorders and immunocompromised states
-
During active chemo/radiotherapy
-
Active chronic or aggressive periodontitis.
For rare conditions or syndromes for which there is no high quality evidence of success rates, it is best practice to obtain a second opinion from a multidisciplinary team in secondary care. It must be noted, however, that there is very little evidence for the influence of many systemic diseases on outcomes, and that most advice is drawn from supposition and informed risk assessment. The clinician must, therefore, ask themselves the following questions:
-
Will the placement of the implant/implants jeopardise this patient's immediate health?
-
Will this treatment present significant risk to this patient's future health?
-
Will this patient have the resources and ability to maintain this treatment, and, if not, does this risk the need for significant intervention or changes to their treatment plan later in life?
If the answer to any of these questions is yes, this may not be an appropriate patient to take on for implant-based care. For those patients insistent on implant-retained solutions despite high risks or the presence of contraindications, it is important that clinicians do not feel pressurised into providing care. It is prudent to refer these patients for a second opinion. For all other potential implant cases it is the identification of risk factors that is the most important aspect of consent to long-term outcomes (Table 2). These include:7,29,30
Patient factors
Heavy smoking has been proven to reduce success rates of implants.8,29 The odds of developing peri-implant disease are up to five times greater in smokers.31,32,33 It is sensible to recommend smoking cessation before implant placement. Pragmatic clinicians may place implants in smokers, but the consent for failure and complications must be adjusted accordingly (Fig. 13).
Medical factors
Diabetics with poor glycaemic control have been found to have reduced survival rates of implants, potentially based on reduced healing capacity.34,35 Similarly, alteration of bone composition by bisphosphonates or radiation therapy also affect predictable healing and, thus, may affect osseointegration or result in medication-related osteonecrosis or osteoradionecrosis.35 Though the British Society of Restorative Dentistry does not recommend placing implants in patients with uncontrolled diabetes, patients with osteoporosis on bisphosphonates or those patients with a history of irradiation of the head and neck, there may be patients with these conditions who can only be adequately rehabilitated with dental implants.26 For those taking bisphosphonates it is important to differentiate high-risk patients from those of lower risk. Treatment should be avoided or referred for patients taking bisphosponates for greater than three years, with additional steroid supplements for those on IV bisphosphonates.36 Placement in irradiated patients is not an absolute contraindication, but this care should be provided as part of a multidisciplinary team in secondary care to support rehabilitation of patients where conventional treatment is not possible (Fig. 14). For all these patients, not only must the risk of failure be identified, but also significant complications such as ORN or BRONJ.
Oral environment
Periodontal disease
Patients with active periodontitis suggests poor levels of oral hygiene and the presence of virulent microorganisms that may result in peri-implant disease.29,40 Implants placed into patients with a history of periodontal disease have a higher risk of peri-implantitis, peri-implant bone loss and implant loss.37 In patients with at least one 6 mm periodontal pocket, there is a further increase in the risk of peri-implant disease. No implants should be placed in periodontally active individuals and, furthermore, if there are any concerns about a patients current ability to maintain a prosthesis and implants, treatment should be deferred until they can demonstrate excellent plaque control (Fig. 15).
A fixed bridge was placed on 4 implants in the mandible with a non-cleansable design and the results were catastrophic. Fig. 15b clearly shows the calculus deposits underneath the bridge, Fig. 15c the inflammation around the implants and Fig. 15d the extent of peri-implant disease at surgical exploration.
Parafunction
Consideration must also be given to the distribution of occlusal forces where placing implants. Parafunction may increase implant failure due to increased levels of unpredictable loading (Fig. 16).30,41,42 Though not a contraindication, special precautions must be taken. All patients with evidence of parafunctional habits should be given bite guards to protect restorations. The restorative dentists should also consider using materials that may cause less damage to the opposing dentition and can be easily repaired such as acrylic and composite. Implants should ideally be loaded axially, free from excursive guidance with flattened cusps and shallow fossae.42
Site selection
Poor bone volume and quality have been proven to contribute to implant failure.9,30,41 Thin cortical bone, and loosely organised trabecular bone may require modification of drilling technique and reduced ridge volume may require grafting or sinus lifting in order to provide sufficient for implant placement. Grafting potentially reduces the prognosis of implants.43 This reduced prognosis has to be weighed against the risk of failure when using shorter, wider implants in a reduced bone volume. Grafting can be carried out using a block of cortical-cancellous bone from a donor site or a particulate graft using bone fragments, often with an osteo-conductive material. In both cases it is important to allow time, often over six months, for blood supply to develop within the bone and in the particulate graft for the lamellar pattern to mature and give strength. This also allows monitoring for resorption of the graft over the initial period. Grafting may not be successful (Fig. 17).
Timing of placement has attracted significant interest as the ability to place an implant into a fresh extraction socket can significantly reduce the duration of treatment and number of surgery appointments. Though implants can integrate well when placed immediately, the final aesthetics, soft tissue healing and patient satisfaction in these cases are often underreported.44
Aesthetic factors
As discussed, poor aesthetics may contribute to failure of an implant supported restoration. This can be due to bony defects, more common in periodontally involved teeth or teeth long since extracted, or implant position, which may be compromised if the ridge is far from the aesthetic zone. Soft tissue problems, for example thin biotype allowing shine-through of metal components or lack of papillae, are also common. In sites with insufficient keratinised tissue, there may be increased plaque, inflammation, mucosal recession and, potentially, attachment loss.45 In these cases, roll flaps, free gingival grafts or connective tissue, and coronally advanced flaps are predictable techniques to bolster the tissues.
Surgical factors
After planning is complete, implant type and placement contribute further towards an optimum environment for healing. Threaded implants give increased primary stability and newer, material-modified and roughened implant surfaces increase the predictability of osseointegration.43 It is good practice to use a surgical stent to guide an accurate, prosthetically-driven placement (Fig. 18). Slow drilling with water-cooling prevents transmission of heat at the implant-bone interface, thus preventing bony necrosis, which can lead to early failure.41,43
Fig. 18c revealed how a lack of restorative awareness and no stent can result in very poor positioning
There is some low-quality evidence to support the use of antibiotics pre-operatively when placing implants to reduce early failure, however, there is no evidence that any specific regimen is significantly better than another, and the mechanism of this effect is unclear.46 Post-operative use of antimicrobials has no specific supporting evidence.
During and after placement of the implant, it is important that the soft tissues are managed appropriately in order to assist effective healing, as well as satisfactory aesthetics where required. Surgery can be carried out by raising a muco-periosteal flap to expose bone or by using a 'flapless' approach with similar aesthetic and survival outcomes in the long term.47
Operator skill may also be associated with improved outcomes of treatment.48 As such, it is not only important to quote evidence-based survival and success data, but to frame this in the context of one's own experience. Practitioners new to implantology should arguably reduce their success rates accordingly.
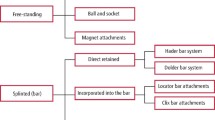
Restorative factors
Removable prostheses have an increased incidence of implant and prosthesis failure.49 Nonetheless, there are situations where removable complete or partial dentures with implant attachments (often ball-, bar- or magnet-retained) are the only option to restore large edentulous spans. This is most notable where aesthetics require a flange, where soft tissue visualisation is required or where maintenance of fixed prostheses will likely be compromised. Implant retained complete dentures are the gold-standard treatment for the atrophic edentulous mandible23 and there is evidence that patients are as satisfied with removable prostheses as they are with fixed.50
Fixed prostheses are employed commonly and predictably in small spans and single-tooth replacements. For larger spans there are options for full mouth fixed restorations in an 'all-on-four'51 or 'all-on-six' type approach with evidence supporting use of four or more implants for full arch restoration.49 There is so far a dearth of success-based evidence around the 'all-on-four' protocol. The ambition should be to plan for screw-retained restorations wherever possible, as this allows removal for maintenance and future retrievability, should there be any technical complications. Though there is evidence of increased screw loosening in screw-retained restorations, this risk must be balanced with the benefit of access. Furthermore, cement-retained restorations have an associated risk of cement extrusion sub-gingivally, resulting in peri-implant cementitis and potentially peri-implantitis.
Maintenance
Good oral hygiene and preventative care forms the basis of dental prevention. Although dental implants and implant-retained prostheses are not at risk of caries, plaque-related gingival diseases can still affect them.40,52,53 The odds ratio of developing disease around implants is up to fourteen times greater in patients with poor oral hygiene.29 This can be further compounded by systemic factors such as diabetes or xerostomia, either at the time of implant placement or developed subsequently.34,35 Patients must be informed of their responsibility to maintain their implants and should be educated to undertake their own oral hygiene maintenance to the highest standard with interdental brushes and irrigation devices (Fig. 19). However, in-surgery maintenance should be carried out at appropriate intervals based on risk factors.54 This may require removal of the implant suprastructure to probe and clean around the implants. Unfortunately, this may only be possible with screw-retained restorations.
The reasonable patient standard
Following the case of Montgomery vs the Lanarkshire Health Board, the traditionally applied Bolam test may no longer stand up to scrutiny in the face of a legal challenge. Instead a new concept of consent has emerged called the 'lay standard' or 'reasonable patient standard.' Decisions about health care interventions must now be made by considering what the reasonable patient may expect to know in advance of care, rather than what a body of dentists would suggest the patient should know.55 Therefore, the clinician must disclose all information that a reasonable patient would want to know. It is as yet unclear how different the consent process should be, but this change opens clinicians' communications and information transfer to the judgement of lay people, not simply fellow health professionals or experts. As such it may emerge in time that patients have very differing concepts of what constitutes informed consent. Nonetheless, key themes to consider when taking consent and communicating with patients may include:
-
How long will this rehabilitation take and what factors may complicate or delay treatment?
-
How long will this last?
-
What maintenance regimes are required and what will these cost?
-
What happens when this treatment fails?
-
What happens when teeth around this prosthesis fail?
Conclusion
The differentiation between success and survival is a significant one. Implant placement and restoration is complex. With this complexity comes the risk of failure. As parameters of success evolve, this may not only include failure of the implant or the restorative suprastructure, but more simply failure to meet the patient's expectations. Thorough experience and evidence-based consent must be undertaken to prevent a disconnect between expectation and reality. This includes making patients aware of pre-existing risk factors, the surgical process and the importance of patient compliance, as well as the likelihood that the restorations may need periodic replacement. If in combination these risk factors suggest the outcome of care may be unpredictable it may be sensible to counsel against implant-based treatment.
References
Pjetursson B E, Brägger U, Lang N P, Zwahlen M . Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin Oral Implants Res 2007; 18 (Suppl. 3): 97–113.
Saunders W P, Saunders E M . The root filling and restoration continuumprevention of long-term endodontic failures. Alpha Omegan 1997; 90: 40–46.
Edelhoff D, Sorensen J A . Tooth structure removal associated with various preparation designs for anterior teeth. J Prosthet Dent 2002; 87: 503–509.
Brånemark P I, Adell R, Breine U, Hansson B O, Lindström J, Ohlsson A . Intra-osseous anchorage of dental prostheses. I. Experimental studies. Scand J Plast Reconstr Surg 1969; 3: 81–100.
Albrektsson T, Zarb G, Worthington P, Eriksson A R . The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants 1986; 1: 11–25.
Jung R E, Zembic A, Pjetursson B E, Zwahlen M, Thoma D S . Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin Oral Implants Res 2012; 23 (Suppl. 6): 2–21.
Porter J A, von Fraunhofer J A . Success or failure of dental implants? A literature review with treatment considerations. Gen Dent 2005; 53: 423–432.
Papaspyridakos P, Chen CJ, Singh M, Weber HP, Gallucci G O . Success criteria in implant dentistry: a systematic review. J Dent Res 2012; 91: 242–248.
Misch C E . Contemporary implant dentistry. St. Louis: Mosby Elsevier; 2008.
Schnitman P A, Shulman L B . Recommendations of the consensus development conference on dental implants. J Am Dent Assoc 1979; 98: 373–377.
Lindhe J, Meyle J, Group D of European Workshop on Periodontology. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol 2008; 35 (Suppl. 8): 282–285.
Zitzmann N U, Berglundh T . Definition and prevalence of peri-implant diseases. J Clin Periodontol 2008; 35 (Suppl. 8): 286–291.
Lang N P, Mombelli A, Tonetti M S, Brägger U, Hämmerle C H . Clinical trials on therapies for peri-implant infections. Ann Periodontol 1997; 2: 343–356.
Grossmann Y, Levin L . Success and survival of single dental implants placed in sites of previously failed implants. J Periodontol 2007; 78: 1670–1674.
Jung R E, Pjetursson B E, Glauser R, Zembic A, Zwahlen M, Lang NP . A systematic review of the 5year survival and complication rates of implant-supported single crowns. Clin Oral Implants Res 2008; 19: 119–130.
Sailer I, Mühlemann S, Zwahlen M, Hämmerle C H F, Schneider D . Cemented and screw-retained implant reconstructions: a systematic review of the survival and complication rates. Clin Oral Implants Res 2012; 23 (Suppl. 6): 163–201.
Berglundh T, Persson L, Klinge B . A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol 2002; 29 (Suppl. 3): 197–212.
Meijer H J A, Raghoebar G M, Van't Hof M A, Visser A . A controlled clinical trial of implant-retained mandibular overdentures: 10 years' results of clinical aspects and aftercare of IMZ implants and Brånemark implants. Clin Oral Implants Res 2004; 15: 421–427.
Tjan A H, Miller G D, The J G . Some esthetic factors in a smile. J Prosthet Dent 1984; 51: 24–28.
Dostálová T, Radina P, Seydlová M, Zvárová J, Valenta Z . Overdenture implants versus teeth quality of life and objective therapy evaluation. Prague Med Rep 2009; 110: 332–342.
Gatten D L, Riedy C A, Hong S K, Johnson J D, Cohenca N . Quality of life of endodontically treated versus implant treated patients: a University-based qualitative research study. J Endod 2011; 37: 903–909.
Awad M A, Locker D, Korner-Bitensky N, Feine J S . Measuring the effect of intra-oral implant rehabilitation on health-related quality of life in a randomized controlled clinical trial. J Dent Res 2000; 79: 1659–1663.
Feine J S, Carlsson G E, Awad M A et al. The McGill consensus statement on overdentures. Mandibular two-implant overdentures as first choice standard of care for edentulous patients. Gerodontology 2002; 19: 3–4.
Buser D, von Arx T, ten Bruggenkate C, Weingart D . Basic surgical principles with ITI implants. Clin Oral Implants Res 2000; 11 (Suppl. 1): 59–68.
Bornstein M M, Cionca N, Mombelli A . Systemic conditions and treatments as risks for implant therapy. Int J Oral Maxillofac Implants 2009; 24 (Suppl.): 12–27.
British Society of Restorative Dentistry. Statement on implantology. 2013.
Chanavaz M . Patient screening and medical evaluation for implant and preprosthetic surgery. J Oral Implantol 1998; 24: 222–229.
Cionca N, Giannopoulou C, Ugolotti G, Mombelli A . Amoxicillin and metronidazole as an adjunct to full-mouth scaling and root planing of chronic periodontitis. J Periodontol 2009; 80: 364–371.
Heitz-Mayfield L J A . Peri-implant diseases: diagnosis and risk indicators. J Clin Periodontol 2008; 35 (Suppl. 8): 292–304.
Palmer R M . Risk management in clinical practice. Part 9. Dental implants. Br Dent J 2010; 209: 499–506.
Bain C A, Moy P K . The association between the failure of dental implants and cigarette smoking. Int J Oral Maxillofac Implants 1993; 8: 609–615.
Clementini M, Rossetti P H O, Penarrocha D, Micarelli C, Bonachela W C, Canullo L . Systemic risk factors for peri-implant bone loss: a systematic review and meta-analysis. Int J Oral Maxillofac Surg 2014; 43: 323–334.
Strietzel F P, Reichart P A, Kale A, Kulkarni M, Wegner B, Küchler I . Smoking interferes with the prognosis of dental implant treatment: a systematic review and meta-analysis. J Clin Periodontol. 2007; 34: 523–544.
Mellado-Valero A, Ferrer García J C, Herrera Ballester A, Labaig Rueda C . Effects of diabetes on the osseointegration of dental implants. Med Oral Patol Oral Cir Bucal 2007; 12: E38–E43.
Donos N, Calciolari E . Dental implants in patients affected by systemic diseases. Br Dent J 2014; 217: 425–430.
Madrid C, Sanz M . What impact do systemically administrated bisphosphonates have on oral implant therapy? A systematic review. Clin Oral Implants Res 2009; 20 (Suppl. 4): 87–95.
Sgolastra F, Petrucci A, Severino M, Gatto R, Monaco A . Smoking and the risk of peri-implantitis. A systematic review and meta-analysis. Clin Oral Implants Res 2015; 26: E62–E67.
Salvi G E, Carollo-Bittel B, Lang N P . Effects of diabetes mellitus on periodontal and peri-implant conditions: update on associations and risks. J Clin Periodontol 2008; 35 (Suppl. 8): 398–409.
Kotsovilis S, Karoussis I K, Fourmousis I . A comprehensive and critical review of dental implant placement in diabetic animals and patients. Clin Oral Implants Res 2006; 17: 587–599.
Ferreira S D, Silva G L M, Cortelli J R, Costa J E, Costa F O . Prevalence and risk variables for peri-implant disease in Brazilian subjects. J Clin Periodontol 2006; 33: 929–935.
Handelsman M . Surgical guidelines for dental implant placement. Br Dent J 2006; 201: 139–152.
Kinsel R P, Lin D . Retrospective analysis of porcelain failures of metal ceramic crowns and fixed partial dentures supported by 729 implants in 152 patients: patient-specific and implant-specific predictors of ceramic failure. J Prosthet Dent 2009; 101: 388–394.
Chrcanovic B R, Albrektsson T, Wennerberg A . Reasons for failures of oral implants. J Oral Rehabil 2014; 41: 443–476.
Buser D, Chen S T, Weber H P, Belser U C . Early implant placement following single-tooth extraction in the esthetic zone: biologic rationale and surgical procedures. Int J Periodontics Restorative Dent 2008; 28: 441–451.
Lin GH, Chan HL, Wang HL . The significance of keratinized mucosa on implant health: a systematic review. J Periodontol 2013; 84: 1755–1767.
Esposito M, Coulthard P, Oliver R, Thomsen P, Worthington H V . Antibiotics to prevent complications following dental implant treatment. Cochrane Database Syst Rev 2003; 3: CD004152.
Esposito M, Maghaireh H, Grusovin M G, Ziounas I, Worthington H V . Interventions for replacing missing teeth: management of soft tissues for dental implants. Cochrane Database Syst Rev 2012; 2: CD006697.
Esposito M, Hirsch J M, Lekholm U, Thomsen P . Biological factors contributing to failures of osseointegrated oral implants. (I). Success criteria and epidemiology. Eur J Oral Sci 1998; 106: 527–551.
Kern JS, Kern T, Wolfart S, Heussen N . A systematic review and meta-analysis of removable and fixed implant-supported prostheses in edentulous jaws: post-loading implant loss. Clin Oral Implants Res 2015; 10.1111/clr.12531.
Fueki K, Kimoto K, Ogawa T, Garrett N R . Effect of implant-supported or retained dentures on masticatory performance: a systematic review. J Prosthet Dent 2007; 98: 470–477.
Maló P, de Araújo Nobre M, Lopes A, Francischone C, Rigolizzo M . 'Allon4' immediate-function concept for completely edentulous maxillae: a clinical report on the medium (3 years) and long-term (5 years) outcomes. Clin Implant Dent Relat Res 2012; 14 (Suppl. 1): E139–E150.
Alani A, Kelleher M, Bishop K . Peri-implantitis. Part 1: Scope of the problem. Br Dent J 2014; 217: 281–287.
Alani A, Bishop K . Peri-implantitis. Part 3: current modes of management. Br Dent J 2014; 217: 345–349.
Alani A, Bishop K . Peri-implantitis. Part 2: Prevention and maintenance of peri-implant health. Br Dent J 2014; 217: 289–297.
D'Cruz L, Kaney H . Consent a new era begins. Br Dent J 2015; 219: 57–59.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Beaumont, J., McManus, G. & Darcey, J. Differentiating success from survival in modern implantology – key considerations for case selection, predicting complications and obtaining consent. Br Dent J 220, 31–38 (2016). https://doi.org/10.1038/sj.bdj.2016.26
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2016.26
This article is cited by
-
Evaluation of the accuracy of fully guided implant placement by undergraduate students and postgraduate dentists: a comparative prospective clinical study
International Journal of Implant Dentistry (2024)
-
Restorative dentistry clinical decision-making for hypodontia: managing missing premolar teeth
British Dental Journal (2023)
-
Management of missing maxillary lateral incisors in general practice: space opening versus space closure
British Dental Journal (2019)
-
Unilateral removable partial dentures
British Dental Journal (2017)