Key Points
-
Outlines the role of the dental team in adult safeguarding issues.
-
Explains how the 'Care Act 2014' affects dental practitioners.
-
Reviews types of abuse, who is affected by safeguarding issues and what happens when a report is made.
-
Provides scenarios as examples.
Abstract
The legal responsibilities of all those involved in the care of adults at risk of harm were set out in the 'Care Act 2014' which became law in England in April 2015. In the same month, the General Dental Council (GDC) announced that 'safeguarding vulnerable adults' was to become a recommended topic for continuing professional development (CPD), along with 'safeguarding children and young people.' This paper updates on relevant legislation, and outlines the role of dental professionals in adult safeguarding. It then advises on issues surrounding safeguarding concerns, using three scenarios for illustration. Rather than covering the very broad topic of abuse of adults in general, the paper focusses on 'adults at risk' to whom statutory safeguarding law applies.
Similar content being viewed by others
Background
The 'Care Act 2014'1 enacted in April 2015 in England included an update on protecting 'adults at risk' from abuse or neglect (also known as 'safeguarding'). The Care Act clarifies to whom adult safeguarding procedures apply. They concern any adult who:
-
Has care and support needs
-
Is experiencing, or is at risk of, abuse or neglect
-
Is unable to protect themselves because of their care and support needs.2
According to the Department of Health the previous legal framework for adult protection was 'neither systematic nor coordinated, reflecting sporadic development of safeguarding policy over the last 25 years.'3
The Act sets out the legal responsibilities of all clinicians. It is important for the dental practitioner to establish clear pathways for reporting safeguarding issues. The Care Act places the responsibility for investigating adult safeguarding concerns with local authorities. There is a legal requirement that each local authority must set up a Safeguarding Adults Board (SAB) which must 'include the local authority, the NHS and the police, who should meet regularly to discuss and act upon local safeguarding issues'.1
A year on year increase in reports of abuse of vulnerable adults in England has been described in the 'Abuse of vulnerable adults in England' annual reports published by the Health and Social Care Information Centre (HSCIC). In the year 2012–2013 a total of 176,000 adult safeguarding alerts were raised.4 This compared to 136,000 in 2011–20125 and 94,200 in 2010–2011.6 Although reporting English data the results are relevant to all dental teams and the stark annual increases exemplify the need to be cognisant of local reporting procedures. National reporting procedures changed for the year 2013–2014, and are now referred to as the 'Safeguarding adults return'.7 A number of data items have been modified which mean annual comparisons cannot now be made in many cases. For example, the total number of individuals for whom safeguarding referrals were opened are now reported, whereas previous data reported the total number of separate 'alerts'. An 'alert' is a contact by a professional concerning an individual the professional is concerned about. Several alerts may be raised by different professionals about the same individual. A 'safeguarding referral' is when an investigation is instigated under the safeguarding process after one or more alerts has been raised about a risk of abuse. In 2013–2014, safeguarding referrals were opened for 104,050 individual adults.7
The need for collaboration between all health and social care professionals is evidenced by the results of the Francis inquiry into patient care at Mid Staffordshire NHS Foundation Trust.8 This highlighted repeated failures to raise concerns leading to the 'appalling suffering of many patients'.8 Dentists and other members of the dental team are in a key position to raise concerns over abuse of adults at risk of harm. Table 1 shows that only social care staff make more referrals than health staff.
What is 'safeguarding' and who is 'at risk'?
'Safeguarding' involves activity aimed to protect adults at risk and includes prevention initiatives, investigations and professional training in identifying abuse. Table 2 is taken from the Department of Health's 'Six safeguarding principles'.9
The term 'adult at risk of harm' has increasingly been used over 'vulnerable adult'.10 The Care Act continues to use the term 'adult at risk' but more frequently refers to 'adults with care and support needs'.1 Adults who may be at risk are summarised in Table 3.2
Each of the examples in Table 3 can present across a broad spectrum and may require dental care from any area of dental services. Although adults with more severe disabilities may receive care within the community or hospital dental services, the role of the dental team in general practice is essential in identifying early signs of abuse for vulnerable adults who use their service. Indeed, General Dental Practitioners (GDPs) in many ways are in a unique position to help protect people in that they may see the same patients throughout their lifetime. They may well be the first health care professionals to notice signs of abuse if the adult at risk has limited contact with health services. Figure 1 shows the percentage of referrals based on client type.
Percentage distribution of Individuals with referrals by primary client group, 2013-14 England (taken from The Adult Safeguarding Return by HSCIC7)
It can be difficult to ascertain whether safeguarding procedures apply.11 The Social Care Institute for Excellence's response to The Care Act 2014 gives further clarification here by stating that the above:
'...is not an exhaustive list. In its definition of who should receive a safeguarding response, the legislation also includes people who are victims of sexual exploitation, domestic abuse and modern slavery. These are all largely criminal matters, however, and safeguarding duties would not be an alternative to police involvement, and would only be applicable at all where a person has care and support needs that mean that they are not able to protect themselves.'2
What can be considered abuse?
The Care Act supersedes the previous 'No Secrets'12 document which sought to define abuse. The Department of Health accompanied the Care Act with 'Care and Support Statutory Guidance'.13 This expands on the types of abuse listed in 'No Secrets' but stresses that, rather than being an exhaustive list, this is 'an illustrative guide as to the sort of behaviour which could give rise to a safeguarding concern'.13 Table 4 gives a summary of these.
Of interest to the dental profession is the increased emphasis on neglect and, in particular, self-neglect. These additional topics aim to give the relevant authorities more scope in providing support for individuals whose behaviour is putting themselves at increased risk.
Of interest in Table 5 is that neglect, financial and psychological abuse were the second, third and fourth most common forms of alleged abuse in 2012–2013, and these three forms made up 61% of all alleged cases. These may demand more subtle forms of enquiry with the patient, and dental professionals may need to make further enquiries from families and carers. As always, clear recording of any observations is essential.
Reporting suspected abuse
The British Medical Association (BMA) have produced a safeguarding toolkit for General Medical Practitioners (GMPs) to refer to14 which is highly relevant to General Dental Practitioners (GDPs) and indeed all dental professionals who treat adults. The toolkit recommends a stepped approach beginning with identification and risk assessment of individuals who could be at risk of harm, assessing the patient's competence (an assessment of 'mental capacity' which is outlined in the Mental Capacity Act 2005.15 The GDC 'Standards for the dental team' does not offer guidance on disclosing information concerning adults who lack capacity.16 Specific information on this can be found in the 'Confidentiality guidance: Disclosures about patients who lack capacity to consent' section of the GMC's 'Good Medical Practice' document.17 Advice from defence organisations would be useful in deciding whether confidentiality should be broken.
Typically, an alert is raised with the local authority which has responsibility for acting on safeguarding concerns. In some jurisdictions this responsibility may be delegated to another organisation (for example a partnership NHS trust).
National variation
The Care Act guidance exemplifies the difficulty in providing a generic 'who to contact' directory and it is hoped that the legal change that the act represents will ensure a more transparent reporting system for dentists, and all those with safeguarding responsibilities, to follow. The Care Act only relates to England however. In Wales there are four regions, each with its own 'Adult Protection Forum' which co-ordinate adult protection locally.18 The 'Social Services and Wellbeing (Wales) Act 201419 places more responsibility within the local authorities and introduces provision of an “adult protection and support order” allowing local authorities access to the homes of people suspected of being abused. The legal responsibilities of all relevant parties in reporting suspected abuse are increased and outlined. In Scotland the 'Adult Support and Protection (Scotland) Act (2007)'20 states that 'each council must establish an Adult Protection Committee (APC)', and there are increasing moves to merge social care and NHS budgets.
In Northern Ireland the 'Protocol for Joint Investigation of Alleged and Suspected Cases of Abuse of Vulnerable Adults (2009)'21 suggests that multiple agencies are involved but the Police Service of Northern Ireland and Health and Social Care bodies work collaboratively. Some areas in Northern Ireland have a dedicated team, others recommend the police as a first contact.
Responsibilities of individual professionals and of practice owners
The overall effect of the Care Act on the dental profession is that although greater legal emphasis is placed on the responsibility of all those involved in the care of vulnerable adults, local arrangements for reporting will still vary between local authorities. This means that a dentist working across a number of sites may need to be cognisant of a number of different agencies responsible for adult protection. According to the General Dental Council's 'Standards for the dental team', 'You must take appropriate action if you have concerns about the possible abuse of children or vulnerable adults'.16 Furthermore if you 'employ, manage or lead a team' then there must be an effective procedure for raising concerns which should be readily available to all staff. To be compliant with the Care Quality Commission, providers of dental services must 'Ensure that government and local guidance about safeguarding people from abuse is accessible to all staff and put into practice'.22 Due to wide local variation for reporting abuse of adults it is recommended that each practice, clinic or hospital has up-to-date contact details for the agency responsible for adult protection.
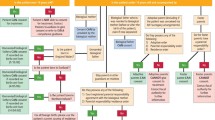
What happens after a report has been made?
It should be noted that a report of suspected abuse will not always lead to a full investigation. Rather, the relevant authorities will determine whether an investigation is necessary.
The professional, usually a social worker, responsible for discussing your concern (an 'alert') about a vulnerable adult will ask questions to clarify detail. From the information you give, and other intelligence they have about the case, they will make a judgement on whether to proceed with a safeguarding investigation (a 'referral'). If an investigation goes ahead they will use a variety of inquisitive methods in order to establish the facts. This may include a meeting of professionals involved in caring for the patient, including the dentist, to decide on a way forward. If there is the suspicion that a crime has been committed, the police will be involved through their specialist safeguarding teams.
Scenarios
The following case studies give examples of possible scenarios and how a dental professional may be involved in safeguarding issues. Key safeguarding principles from the Department of Health9 are given in italics. Every situation will be different but definitions of abuse and safeguarding aim to make it clear when to act. However, all of these scenarios would likely require a record being made in the patient's notes of what happened and what action, if any, was taken. The primary aim is for the protection of adults at risk so if in any doubt, aim to discuss concerns with an expert in safeguarding.
Scenario 1
A 70-year-old female patient with advanced Alzheimer's disease attends a general dental practice regularly. She usually attends with her son and she is often, but not always, very confused at appointments. On one appointment she is brought by her daughter and the patient tells you she has been complaining of severe toothache for two weeks but no-one has made her an appointment until now. Her daughter claims this isn't true.
This scenario may be a form of neglect. If the patient is reliant on others for personal care and those needs are ignored then any omission that results in harm may amount to neglect. However given the patient has Alzheimer's disease, it may be that the patient is disorientated to time and is mistaken about how long she has waited for the appointment.
It would be important to clarify detail as far as possible (to ensure proportionality of response). A discussion with the daughter around the history of presenting complaint may help build understanding of how the situation evolved (as part of working towards protection). Given she is usually very confused in the surgery it would be reasonable to enquire after her usual care arrangements at home, how her meals are prepared and who supports her diet. The patient may be willing to talk to you on her own where she may feel more able to disclose more detail about her comments (a way of promoting empowerment of the individual). These may confirm or allay your suspicions of abuse.
If you remain concerned, liaison with other professionals can be key (working in partnership). The GP is a key contact and knows the breadth of care that the patient is receiving and may have information relevant to your concerns. Alternatively talking with your local social work safeguarding adults professionals may help decide whether a more comprehensive investigation is necessary. The dentist's main role here would be to share information in order for social care to make a decision about next steps, such as whether a safeguarding referral is appropriate.
Scenario 2
A 25-year-old female with learning difficulties attends your general practice regularly for treatment. When advising her about reducing sugar in her diet she tells you that she is not allowed to buy sweets and her sister doesn't let her have any of her own money. She goes on to say that her sister 'takes' all of her benefits and she never has access to any cash. She tells you she has not bought anything with her own money for a long time.
This person would be considered a vulnerable adult and has disclosed potential financial abuse. There could be a number of reasons that she reports not having access to her money. She may have issues with managing her money so caring relatives may support her in budgeting and avoiding over spending. Further discussion should reveal whether she has no access to cash at all or whether she has agreed to any restrictions. In cases of significant concern an appointeeship may have been arranged. This is a formal legal arrangement with the Department of Work and Pensions (in England) for an appointed person to manage benefits on behalf of another. Often the appointed person is a family member.
The alternative explanation may be that her benefits are being stolen by her sister and she is being financially abused. If this is the case, the patient may not want to discuss this further. She could be worried that her sister will get into trouble, or be concerned about what further abuse she will suffer if her sister finds out that she has told someone what is happening. Vulnerable people can depend on families for care. This reliance on others and lack of independence can create a relationship where abuse may be more likely to occur. An uneven distribution of power or stressful domestic arrangements can be important factors that can lead to abuse (which can undermine empowerment).
If you do have concerns that she is being financially abused it would be appropriate to seek advice and discuss your concerns with an expert in safeguarding (working in partnership with colleagues). A conversation with the vulnerable adult around next steps can help them to understand that the process is intended to be helpful and may result in alternative forms of support for her and possibly for her sister. The authority would decide whether to proceed with an investigation and put a protection plan in place. Depending on the outcome of the investigation there could be a number of actions by the local authority ranging from additional support to the family if there are genuine concerns over budgeting, to appointeeship with the family or local authority, to criminal proceedings towards the sister. As with any form of abuse, uncovering financial abuse may reveal other forms of abuse including psychological and physical abuse. If so the protection plan and social interventions go much further than anticipated to support the vulnerable person.
Scenario 3
A 75-year-old male in a wheelchair attends your general practice with several facial bruises. He is in a large residential care home but you have no reason to suspect he lacks capacity. A member of care staff brings him to the surgery and waits in the waiting room and the patient makes his own treatment decisions. When asked about the bruises he claims some of the staff in the home can be 'a bit heavy handed' but he'd 'rather not make a fuss.'
Again, suspicion of abuse should be a high priority in this case given the serious injury. The man lives in a care home, and therefore there may be other victims that have experienced abusive treatment. It would be important to clarify with this man what he means, whether the home have recorded his injuries as an incident, whether the injuries were considered accidental or intentional, and what action was taken by the home to protect the man from further injury.
It may be appropriate to contact the manager of the care home. This person would have a responsibility for overseeing care in the home (and hold significant accountability for safeguarding people in their care). They should be able to clarify what has happened and collaborate (work in partnership) on necessary next steps. If this is not possible or your concerns remain, you should seek to speak about this with your local safeguarding adults team. It is important to make sure that there is a plan before he leaves the surgery as he may return to his home to experience further abuse. The plan could involve contact with the police by social services as there is concern that the patient may have been assaulted.
References
Department of Health. The Care Act 2014. 2014. Online information available at www.legislation.gov.uk/ukpga/2014/23/contents/enacted (accessed September 2015).
Social Care Institute for Excellence. Care Act 2014 Beyond compliance – towards excellence. 2014. Online information available at www.scie.org.uk/care-act-2014/safeguarding-adults/adult-safeguarding-practice-questions/index.asp (accessed September 2015).
Department of Health, Factsheet 7 The Care Act – Protecting adults from abuse or neglect. 2014. Online information available at www.gov.uk/government/uploads/system/uploads/attachment_data/file/366087/Factsheet_7_-_Safeguarding.pdf (accessed September 2015).
Health and Social Care Information Centre (HSCIC). Abuse of vulnerable adults in England 20122013', 2014. Online information available at www.hscic.gov.uk/catalogue/PUB13499 (accessed September 2015).
Health and Social Care Information Centre (HSIC). Abuse of vulnerable adults in England 20112012. 2013 Online information available at www.hscic.gov.uk/catalogue/PUB10430 (accessed September 2015).
Health and Social Care Information Centre (HSIC). Abuse of vulnerable adults in England 20102011. 2012. Online information available at www.hscic.gov.uk/pubs/provabusevulnerableadults1011 (accessed September 2015).
Health and Social Care Information Centre (HSIC). Safeguarding Adults Return, Annual Report, England 201314: Summary. 2014 Online information available at www.hscic.gov.uk/catalogue/PUB15671 (accessed September 2015).
Francis R . Report of the Mid Staffordshire NHS Foundation Trust public inquiry. 2013. Online information available at www.midstaffspublicinquiry.com/report (accessed September 2015).
Department of Health. Adult safeguarding: statement of government policy. 2013. Online information available at www.gov.uk/government/uploads/system/uploads/attachment_data/file/215591/dh_126770.pdf (accessed September 2015).
The Law Commission. Adult Social Care. 2011. The Stationary Office, London.
Boland B, Burnage, J, Chowhan H . Safeguarding adults at risk of harm Br Med J 2013; 346: 346351.
Department of Health. No secrets: Guidance on developing and implementing multi-agency policies and procedures to protect vulnerable adults from abuse'. 200. Online information available at www.gov.uk/government/publications/no-secrets-guidance-on-protecting-vulnerable-adults-in-care (accessed September 2015).
Department of Health. Care and Support Statutory Guidance. Online information available at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/366104/43380_23902777_Care_Act_Book.pdf (accessed September 2015).
British Medical Association. Safeguarding vulnerable adults: a toolkit for general practitioners. 2011. Online information available at http://web.bma.org.uk/pressrel.nsf/wall/DE99DE079FECAEF2802578DA0037A83B?OpenDocument (accessed September 2015).
United Kingdom Government. Mental Capacity Act. 2005. Online information available at www.legislation.gov.uk/ukpga/2005/9/section/2 (accessed September 2015).
General Dental Council. Standards for the dental team'. 2013. Online information available at www.gdc-uk.org/Dentalprofessionals/Standards/Documents/Standards%20for%20the%20Dental%20Team.pdf (accessed September 2015).
General Medical Council. Good Medical Practice. 2013. Online information available at Available at www.gmc-uk.org/guidance/ethical_guidance/confidentiality_57_63_patients_who_lack_capacity.asp (accessed September 2015).
Social Services Improvement Agency (Wales). Interim Policy and Procedures for the Protection of Vulnerable Adults from Abuse. 2013. Online information available at www.ssiacymru.org.uk/home.php?page_id=8297 (accessed September 2015).
Social Services Improvement Agency (Wales). Social Services Improvement Act 2014. 2014. Online information available at www.ssiacymru.org.uk/home.php?page_id=8297http://www.legislation.gov.uk/anaw/2014/4/contents (accessed September 2015).
The Scottish Government. Adult Support and Protection (Scotland) Act 2007. 2007. Online information available at www.scotland.gov.uk/Topics/Health/Support-Social-Care/Adult-Support-Protection (accessed September 2015).
The Regulation and Quality Improvement Authority (Northern Ireland). Protocol for Joint Investigation of Alleged and Suspected Cases of Abuse of Vulnerable Adults. 2009. Online information available at www.rqia.org.uk/cms_resources/Vulnerable%20Adults%20Protocol%20Jul%2009.pdf (accessed September 2015).
Care Quality Commission. Guidance about compliance. Essential standards of quality and safety. Care Quality Commission. 2010. Online information available at www.cqc.org.uk/sites/default/files/documents/guidance_about_compliance_summary.pdf (Accessed September 2015).
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Lewney, J., Boland, B. Adult safeguarding; guidance for dental professionals. Br Dent J 219, 287–291 (2015). https://doi.org/10.1038/sj.bdj.2015.721
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2015.721
This article is cited by
-
A guide to treatment planning in complex older adults
British Dental Journal (2018)
-
Holistic care: Vulnerable in pregnancy
British Dental Journal (2016)
-
Elder abuse and the dental team
BDJ Team (2016)