Key Points
-
The study shows how the role of dental therapists employed in dental practices may vary with the composition of the dental team.
-
A high failed appointment rate of about 20% is shown for appointments with a dental therapist in all four practices studied. This may influence how the appointment system is managed in teams including dental therapists.
-
Calculation of the earnings of the dental therapists based on the GDS statement of remuneration is compared with salary and overhead costs to inform the discussion concerning whether general dental practitioners should judge financial barriers as a reason for not employing dental therapists in their practices.
Abstract
Objectives To describe the type of patients seen and work undertaken by dental therapists employed in four personal dental service practices and to report on their cost-effectiveness within the context of the dental practice.
Method All members of the dental team used a standard day sheet to record all patient contacts and procedures undertaken in that session. Dental therapists recorded data for 30 consecutive sessions and dentists recorded information for 20 sessions. Items were recorded in sufficient detail to allow later matching with the GDS statement of remuneration and a calculation of the average gross fees and patient charges per session.
Results The role of the dental therapist varied between the practices studied. In two practices the therapist saw a high proportion of child patients, and in one of these this was combined with providing care for a high number of adult patients who were exempt from patient charges. In the two practices where the dental team did not include a dental hygienist, the dental therapist had a relatively high workload providing dental hygiene care for adult patients. It appears that the gross fees and patient charges generated by the dental therapist in all four PDS practices fail to cover the cost of the salary of the dental therapist, dental nurse and associated overheads borne by the practice.
Similar content being viewed by others
Introduction
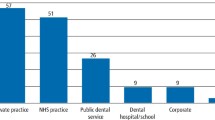
The 1997 NHS (Primary Care) Act allowed the voluntary establishment of pilot schemes to test alternative ways of delivering dental services, in particular general dental services (GDS), through local contracting arrangements. Proposals, which mainly came from dentists based in NHS general dental practices, were submitted to the Department of Health, suggesting ways in which local primary dental care services could be developed.1 Those which were approved became established as personal dental service (PDS) pilots. Within the legislation, the employment of dental therapists in personal dental services was allowed, where previously this had been limited in the UK to only the community dental service and hospital dental services. The stated objective of several PDS pilots was to test the use of dental therapists in a general dental practice like setting, although very little quantitative data has subsequently been published.
The speed of organisational change has continued unabated and there have been further changes to the legislation concerning the employment of dental therapists in UK general dental practice. In July 2002, dental therapists were permitted to work in all types of dental service (including the GDS), and their range of permitted duties were expanded. Despite the fact that general dental services provide the majority of NHS primary dental care in the country, and this development has the potential to change the way in which care is delivered, very little is known about the role dental therapists have in this setting.
The vision for the increased use of dental therapists within primary dental care teams is outlined in the Nuffield Report,2 which states that in order to 'increase the proportion of the population with access to a comprehensive system of care within the cash limits envisaged by the government, a differently constituted workforce would be required with more auxiliaries providing more skills, including preventive and therapeutic skills'. The dental therapists' role within the dental team as envisaged by general dental practitioners (GDPs) is outlined in several surveys which report attitudes of GDPs to employing dental therapists.3,4,5,6 The majority of GDPs surveyed by Hay and Batchelor,4 identified children and patients with special needs as the anticipated client groups for dental therapists, with only 21% suggesting that their client groups might include adults. They also predicted that there would be an equal division of the therapist's time between clinical care and dental health education duties. Indeed some GDPs hold a misconception that therapists are only allowed to undertake operative procedures on children.5,7
Some GDPs involved in establishing PDS pilots have identified the employment of therapists to help in the treatment of difficult child patients as one of the benefits of such a scheme, with the anticipation that therapists could spend more time with the patient than the dentist would be able to do under the financial constraints of the NHS.1 There is, however, no information now such schemes are up and running, that therapists have indeed been used in this way, or whether they have been used merely as extra dental manpower to treat a cross section of patients, in areas where dentists are hard to recruit.8
Whether or not to employ a dental therapist within a GDS practice is now a decision facing many GDPs. Financial considerations appear to play a significant part in that decision.5,6 In a study of GDPs in West Sussex carried out in 2000, when asked what they felt was the biggest barrier to employing a therapist in practice, financial barriers were mentioned most often.5 Comments such as 'if salaried, impossible to employ them for NHS', 'the current GDS fee scale is uneconomic and employing a therapist ....would cost me money', illustrate their concern. It is important that some information is available to address the issue and establish whether or not employing a dental therapist in general dental practice, is indeed uneconomic from the point of view of the employing dental practitioner.
Four PDS pilots in the North West of England employed a dental therapist from the outset. All of these became PDS practices between October 1999 and 2000. Three of the dental practices were located in relatively low socio-economic areas of Merseyside, whereas the other was situated in Ellesmere Port, an industrial area on the southern border of the Wirral peninsula. One dental practice (practice 1) was situated in an area which has an average Townsend material deprivation score of 8.30 and is ranked second worst of all local authorities in the country (based on 1998 boundaries) according to income and employment scores.9 Practices 2 and 3 were situated in areas where the average Townsend material deprivation score was 1.15 and 2.31 respectively. This places practices 2 and 3 in areas ranked 40th and 56th respectively when local authorities are ranked according to income and unemployment statistics. Practice 4, was in an area, significantly more wealthy than the others, with an average Townsend score of 0.04, and ranked 112th out of the 353 local authorities in the country. All four practices had more than one dentist.
Previous studies10,11 have used data from day books routinely kept to record all treatment given to analyse the role of the dental therapist in the dental team. Both of these studies give an insight into the work undertaken by dental therapists in the community dental service. This methodology was therefore used to look at the work undertaken by dental therapists within the context of four PDS pilots. It is possible to describe whether the therapists had a mainly preventive or therapeutic role and whether there were differences between the four practices studied, and also to report on what proportion of work undertaken by dentists in these teams could still have been undertaken by the therapist. Using the GDS statement of remuneration, the income generated by the therapist can be calculated, and put together with the therapist salary and estimate of surgery overheads, a judgement as to whether the employment of a dental therapist is financially beneficial to the practice can be made. The aim of this paper is therefore to describe the type of patients seen, and type of work undertaken by dental therapists in these four PDS practices and to report on their cost-effectiveness within the context of the dental practice.
Method
A day sheet proforma was designed for the purpose of the study, similar to the system used in previous studies10,11 to collect information on the numbers and type of patients seen and dental procedures undertaken by each member of the dental team for each session. The same proforma was used to collect data in all four PDS practices studied. Data was recorded for all booked appointments, with cancellations and patients failing to attend also recorded. Children were defined as those up to and including the age of 16 years. Information on whether adults were exempt from charges was also recorded. Items were recorded in sufficient detail to allow later matching with the GDS statement of dental remuneration. Each dental therapist collected data for 30 consecutive sessions, and all other members of the dental team collected data for 20 consecutive sessions. The number of sessions for which data was recorded was irrespective of the number of sessions per week the individual usually worked at the practice. Members of the dental team who worked fewer sessions therefore collected data over a longer period of time than those working full-time. In practice 2, data for two associates were combined to make 20 sessions of data recorded because of maternity leave arrangements. Data was analysed using the Statistical Package for Social Sciences (SPSS). Differences within the four practices were tested using the Chi-squared and Mann Whitney U-test.
Results
Table 1 shows the composition of the dental team in the four PDS practices by the number of sessions for which data was collected, with the number of booked patients for which data was recorded. PDS practice 1 had only one associate dentist whereas all the others had more than one dentist working in the practice, besides the principal dentist. Subsequent analysis for the various associate dentists are combined into a category 'other dentists'. A hygienist was employed as well as a therapist in PDS practices 2 and 4, but not in PDS practices 1 and 3.
All four practices were mainly NHS practices. Over the study period between 90% (1,145), (practice 2) and 98% (1,279), (practice 4) of all patient attendances were for NHS care. Table 2 shows the percentage of appointments where the patient attended (this excludes failed appointments and cancellations) and also the mean number of failed patient attendances per session for each member of the dental team. The proportion of booked appointments with the dental therapist where the patient attended (and did not either cancel or fail to attend) is relatively equal between the four PDS practices, at between 77% and 79%. In PDS practices 1, 3 and 4 this was a significantly lower rate of attendance than for dentists working in the same practice (p<0.05), although for PDS practice 2 this was not the case. In PDS 1,3 and 4 the overall percentage of patient attendances for the principal and associate dentists was fairly high and so the distinction between the dentists and the therapist was more marked than in PDS practice 2, where dentists had a lower overall percentage of patient attendances.
The principal dentists in practices 1, 2 and 3 all saw a very similar proportion of children (Table 3). The principal dentist in practice 4 saw a lower proportion of children (p<0.001), although in this practice it was notable that for his therapist, about three-quarters of her patients were children, much higher than the other practices. (P<0.001). The therapist in practice 4 also saw a relatively higher proportion of adults patients who were exempt from charges when compared with dentists in her practice (p<0.001), a pattern that was not seen in the other three practices (Table 3).
There is a large range of diagnostic, preventive and therapeutic procedures which may be routinely undertaken by the dental team in dental practice. Table 4 gives details of some of the most common procedures in terms of the mean number of times in one session that the operator undertook this type of task. In practices 1, 2 and 3, the dental therapist undertook more scale and polishes than dentists (p<0.001, p<0.001 and p<0.001 respectively), although this was not the case in practice 4. The dental therapists in practices 1, 3 and 4 also gave dental health education more often per session than dentists in these practices (p<0.001, p<0.001 and p<0.001 respectively) although there was no such difference in practice 2. Fissure sealants were more often undertaken by dental therapists than dentists in all four practices (p<0.001), although in practice 3 this formed a relatively minor part of the therapists' workload.
In all practices apart from practice 1, dental therapists did more restorations on deciduous teeth per session than dentists in their teams; practice 2 (p< 0.001), practice 3 (p<0.05), and practice 4 (p<0.001). The role of the dental therapist was not however confined to the restoration of deciduous teeth, since they were apparently also involved in the restoration of a significant numbers of permanent teeth (Table 4). In practice 2 the therapist actually did more restorations on permanent teeth than dentists (p<0.01).
Table 5 shows the percentages of patient attendances for dentists in each of the four practices where the dentist only was permitted to perform at least one of the procedures. Overall, in the four practices, for almost 80% of patients attending a dentist, the dentist undertook at least one procedure which meant that a therapist would not have been permitted to treat the patient (under the permitted duties in place at that time). This ranged from 84% of patient attendances in practice 1 to 78% in practice 2.
The range of clinical activities within dental practice can be grouped into diagnostic (eg examinations, X rays), preventive (eg scale and polish, oral hygiene instruction, fissure sealants) and therapeutic (eg restorations, extractions). Table 6 shows, comparing dentists and therapists, the percentage of patient attendances per session where diagnostic, preventive and therapeutic activities were undertaken. Dentists in all four practices undertook a diagnostic activity on a relatively high proportion of patient visits, whilst prevention was less often undertaken. This was in contrast to dental therapists, who overall undertook prevention on 75% of patient visits.
When each item of activity was associated with the relevant fee as stated in the GDS statement of dental remuneration used at the time, the mean income per session could be calculated for each dental therapist. These values ranged from £72.82 per session for PDS 4 to £105.45 per session for PDS 1. Since the fee scale represents a gross value which includes factors for overheads and salary, when the fees are offset by the salary paid to the dental therapist and a figure for overheads of 50% is used, as in other studies of this kind,10,12 all of the four practices made a loss per session (Table 7).
Discussion
This study was based in four different dental practices in the North-West of England. Whilst its findings may not be generalisable to other parts of the country because of the relatively small number of practices involved and the potential for each dental practice to have local factors which influence the efficiency and referral patterns within the practice, it does however show that there are differences between dental practices in the way dental therapists are used.
The four dental therapists appear to have taken on different roles within the four dental teams. In dental practice 4 (situated in a relatively more affluent area than the others), about three-quarters of dental therapist patient contacts were with children, a markedly different profile of patients than for dentists in the same dental team (less than 20% of their patients were children). This pattern was also evident in practice 2, but to a slightly lesser extent. It is possible that in these dental practices, the role defined for the dental therapist, was as someone to treat children attending the practice, once a dentist had designed a treatment plan. This is in keeping with the reported attitudes of general dental practitioners, the majority of whom see child patients as the therapists' main client group.4 In practices 1 and 3 therapists appear to have a wider remit, with the proportion of child patients' seen being similar or even lower than that of dentists working in the same practice. Perhaps this is surprising given the nature of the socio-economic status of the area in which these dental practices are situated. One might expect that in such areas the level of dental caries would be particularly high, and if the therapists' role was mainly in the treatment of childhood dental caries, they would be fully engaged in this task. Indeed, results of BASCD studies for the electoral wards in which these practices are situated shows that the mean dmft for 5-year-olds to be 4.13 for the area around practice 1 and 3.94 for the area around practice 3.
The role taken on by the dental therapists in these four teams is revealed by the records of procedures undertaken. The dental therapist in practice 1 actually undertook a relatively high number of restorations on deciduous teeth when compared with dentists in the team, but also spent a significant amount of time undertaking dental hygiene duties for adult patients. The fact that there was no dental hygienist in this team meant that she performed a dual role. The size of the team may also be an important consideration in the dynamics of delegation. Some have argued that since dentists are required to spend time doing examinations and treatment plans before the work can be delegated to a dental therapist, in small teams the dentist would struggle to supply the therapist with an appropriate workload whilst spending the majority of his/her time doing work that only a dentist could do.13,14 Perhaps if the therapist was not fully occupied with work which demanded all the training of a therapist, the remainder of her time was filled with work which could have been carried out by a hygienist. This may have been particularly relevant in PDS practice 1, which was a smaller practice in terms of manpower compared with the others (Table 1). Practice 3 is another example of a team without a dental hygienist and results show that the therapist was used almost entirely as a dental hygienist in this situation. This raises the question, previously posed in a leader in the British Dental Journal in 1980 'what kind of ancillary help do you want?',15 indicating that dental therapists undertaking a dental hygienist role may be not ideal in terms of skill mix.
In one of the PDS practices (practice 4) the dental therapist also appeared to see a disproportionately high number of adult patients who were exempt from patient charges when compared with other members of the team. There are several possible reasons for this pattern. Perhaps dentists within this practice consciously referred exempt adult patients because there would be little possibility of the patient wishing to have work carried out on a private basis, and the dentists were wishing to maximise this source of income. Alternatively, perhaps many fee-paying adults expressed a wish to be seen by a dentist rather than a therapist, and there was the capacity within the practice to accommodate this, whereas patients who were exempt from patient charges either did not express this preference, or were not given any option, but to have treatment with a therapist. The practice concerned was situated in a more affluent area than the others, and further research is needed to establish whether this pattern of referral is characteristic of the dynamics of dental teams in this type of area.
One pattern which did emerge as being remarkably similar in the four practices studied was the level of failed appointments with the dental therapists (around 20%). Two analyses of failed appointments in general dental practice both report an overall failure rate of 11%.16,17 In three of the four practices, the failed appointment rate for the therapist was much higher than for dentists in the team, and in the fourth dental practice (practice 2) there was a policy of heavily overbooking recall examination sessions in anticipation of a high number of these patients failing to attend the appointment, and this explains the relatively high failure rate for appointments with a dentist in this practice. There are several possible reasons for patients being less likely to attend for a dental appointment with a dental therapist than with a dentist, and further research is needed to investigate this issue.
The balance between the therapeutic and preventive role of the dental therapist is an interesting issue. This study showed that even whilst in some practices focusing on undertaking restorative work for children, dental therapists appear to balance this with a relatively high amount of preventive work. Holt and Murray,10 in their study of the clinical contribution of New Cross dental therapists to the community dental service, also noted that the preventive role of dental therapists was assuming a greater importance. It has been argued that since the GDS is structured to provide treatment led by demand, and prevention is not usually demand-led,2 an emphasis on prevention in this situation is difficult to achieve. Dentists who employ dental hygienists have been found to have a higher 'preventive awareness'.18 Perhaps dentists employing PDS dental therapists also have a relatively high 'preventive awareness' and see their employment as a way of increasing the emphasis of prevention in their dental practice. Dentists employing hygienists are reported to perceive that prevention enhances the reputation of the practice, adds to the job satisfaction of the dentist and is part of modern dental philosophy.18 On the other hand, although it might add value to their practice in this respect, the adding of value in terms of financial gain is more questionable. A study of the economic contribution of dental hygienists in America,19 concluded that services carried out by hygienists were something of a 'loss leader' in terms of the rate of return for time spent, however, if dentists wished to provide such services, it was in their interest to delegate these procedures to the maximum extent possible to enable the dentists' productivity to be applied to procedures with higher rates of return. Unfortunately, no such studies are available in the UK.
Two of the studies10,12 used the information to judge the cost-effectiveness of dental therapists by calculating the net earnings of the dental therapists using the GDS statement of dental remuneration and setting this against overheads of 50%. It is striking that even given the differences in the type of treatment undertaken by the dental therapists, the therapists' average gross earnings per session is similar for PDS practices 1,2 and 3. Using the 50% overheads figure, all four practices failed to cover the salary costs of the dental therapist, even though the therapists' salary was not particularly high compared with values from a BDA survey of PCD pay,21 which put the average pay (albeit in 2003) for an employed hygienist at £18.18 per hour. The same survey quotes the average hourly rate for a dental nurse working in a mainly NHS dental practice in the UK as £6.25, or £23.13 for a 3.7 hour session. If we assume that each dental therapist works with a dental nurse, and instead of taking a figure of 50% for overheads, purely off-set the cost of the salary of the therapist and nurse against the gross earnings for the therapists, PDS practice 4 would make a loss per session and PDS 2 practice would break even (even before any account was made of the cost of materials, maintenance of equipment, surgery heating and lighting etc). The cost of supervision of the dental therapist in terms of reduced output from the dentist may also need to be taken into account, and is estimated to be an average loss of one operation per day.11 PDS practice 3 would have £2.98 per session to take account of these additional factors, and PDS practice 1 would have £13.87 per session, after the therapists' and nurses' salary had been taken from the therapists' gross earnings.
This simple equation may not, however, give the full picture of the cost-effectiveness of the dental therapist within this context. It has to be borne in mind that if the work had not been done by the dental therapist, these tasks would have formed part of the dentist' workload and thus the profit margin would have been even less favourable. Delegation may have allowed dentists to spend relatively more time undertaking tasks which only they were permitted to do. Indeed, it is striking that such a high proportion of patient visits to dentists in these practices involved the dentist in a procedure in which no other member of the dental team was permitted to undertake. The Nuffield Report made the point, based on Dental Practice Board statistics, that about 45% of all items of service were combinations of an examination, an X-ray and a scale and polish, with another 35% described as routine extractions and fillings,2 and such low technology work might be suitable for dental auxiliaries. Figures from this study compare favourably with this, with dentists in the PDS practices appearing to concentrate mainly on work for which they were suitably qualified.
Further developments have taken place since this study was undertaken. Dental therapists may now undertake a range of additional duties, which may alter the range of treatment undertaken, and thus the balance of costs within the dental practice. However, the study does provide information relating to the range of duties permitted at the time and will be of value in the planning of future studies. The system of payment of dentists working in the GDS is also set to change, with less of an emphasis on the item of service. The item of service system of payment does however help in the estimation of costs in this type of study, and even though the four PDS practices would have moved away from the item of service system of payment towards more of a block contract, the block contract would have been based on historical earnings based when the practice was operating within the GDS system of fee-per-item, immediately prior to becoming a PDS. If adding a dental therapist to the team is undertaken in order to expand the capacity for treatment and prevention within the practice beyond that which was provided by dentists alone, allowance would have to be made in adding growth money at the outset of the new contract, since it is clear that the addition of a dental therapist to the team would not be self-financing. Further studies need to be undertaken under the new system so that development of the dentists' range of tasks once a therapist is added to the team can be adequately taken into consideration.
Conclusions
The study showed differences in the role undertaken by dental therapists working in four PDS dental practices. In two dental teams the therapist saw a relatively high proportion of child patients compared with dentists, and in one of these teams the therapist also provided care for a relatively large number of patients exempt from dental charges. In two dental teams, both without a dental hygienist, the therapist also provided a dental hygiene service for significant numbers of adult patients.
It appears that dental therapists may play an important role within the dental team, particularly in relation to prevention. However, when the equation comparing the gross fees and patient charges generated by the dental therapist under the current system of remuneration is equated with the cost of the salary of the dental therapist, dental nurse and associated overheads, the dental practice may well make a loss financially. If skill mix is to be expanded in general dental practice, these issues need to be addressed.
References
Barker N, Dixon H . Personal Dental Services – a practitioner's point of view. Br Dent J 2000; 188: 125– 128.
The education and training of personnel auxiliary to dentistry. The Nuffield Foundation, 1993.
Woolgrove J, Harris R . Attitudes of dentists towards delegation. Br Dent J 1982; 153: 339– 340.
Hay IS, Batchelor PA . The future role of dental therapists in the UK: a survey of District Dental Officers and General Practitioners in England and Wales. Br Dent J 1993; 175: 61– 66.
Gallagher JL, Wright DA . General dental practitioners' knowledge of and attitudes towards the employment of dental therapists in general practice. Br Dent J 2002; 193: 37– 41.
Newton JT, Gibbons DE . Vacant posts reported in dental practice: implications for human resource planning. Br Dent J 2002; 192: 37– 39.
Ireland RS . Dental therapists: their future role in the dental team. Dent Update 1997; 24: 269.
Harris RV, Haycox A . The role of team dentistry in improving access to dental care in the UK. Br Dent J 2001; 190: 353– 356.
Department of the Environment, Transport and the Regions. Compendium of clinical and health indicators 2000. Office for National Statistics, March 2001.
Holt RD, Murray JJ . An evaluation of the role of New Cross Auxiliaries and of their clinical contribution to the Community Dental Service. Part 2 – Analysis of day books. Br Dent J 1980; 149: 259– 263.
Sutcliffe P . Dental Auxiliaries: a method of measuring their clinical usefulness. Br Dent J 1969; 139: 418– 420.
Jones DE, Gibbons DE, Doughty JF . The worth of a therapist. Br Dent J 1981; 151: 127– 128.
Swallow N . School for dental therapists. Br Dent J 1996; 180: 285.
Scarrott DM . The economic case for delegation in dentistry. Br Dent J 1973; 134: 23– 24.
Leader. What kind of ancillary help do you want? Br Dent J 1980; 149: pp.
Reekie D, Devlin H, Worthington H . The prevention of failed appointments in general dental practice. Br Dent J 1997; 182: 139– 143.
Moxon S . The patient who did not attend. Br Dent J 1995; 179: 280.
Holloway PJ, Clarkson JE . Cost: benefit of prevention in practice. Int Dent J 1994; 44: 317– 322.
Bader JD, Kaplan AL, Lange KW, Mullins MR . Production and economic contributions of dental hygienists. J Public Health Dent 1984; 44: 28– 34.
General Dental Council (1966). Final report on the experimental scheme for the training and employment of dental auxiliaries. HMSO. London.
British Dental Association. Advice sheet D2: Rewarding staff. PCD pay survey results. British Dental Association. London, 2003.
Acknowledgements
The authors would like to thank all those in the dental practices concerned who helped in the collection of data and in the interpretation of the results. In order to protect the anonymity of the dental practices involved they are not identified by name.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Harris, R., Burnside, G. The role of dental therapists working in four personal dental service pilots: type of patients seen, work undertaken and cost-effectiveness within the context of the dental practice. Br Dent J 197, 491–496 (2004). https://doi.org/10.1038/sj.bdj.4811749
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4811749
This article is cited by
-
What are the possible barriers and benefits to the use of dental therapists within the UK Military Dental Service?
British Dental Journal (2022)
-
What are the possible barriers and benefits to the use of dental therapists within the UK Military Dental Service?
BDJ Team (2022)
-
Timings and skill mix in primary dental care: a pilot study
British Dental Journal (2019)
-
General dental practices with and without a dental therapist: a survey of appointment activities and patient satisfaction with their care
British Dental Journal (2018)
-
Alternative scenarios: harnessing mid-level providers and evidence-based practice in primary dental care in England through operational research
Human Resources for Health (2015)