Abstract
Objectives To compare the effect of topical skin anaesthetic agents on the discomfort and anxiety associated with venous cannulation.
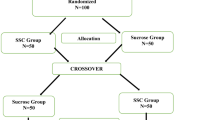
Design Randomised, double-blind, placebo-controlled, within subject, volunteer trial.
Methods 20 healthy volunteers underwent venous cannulation on three separate occasions having received topical skin application of either 4% amethocaine gel (Ametop), 5% eutectic mixture of lidocaine and prilocaine (EMLA) or E45 cream (placebo). Visual analogue and verbal rating scales were used to assess pain and anxiety associated with the venous cannulation, and anticipated anxiety for future cannulation, under each drug condition.
Results Subjects were aged 22-53 years (mean 32.8 years). The mean visual analogue scores (VAS) for discomfort were found to be significantly lower (p<0.001) with Ametop (VAS = 18mm) and EMLA (VAS = 29mm) compared with the control (VAS = 38mm). There was a positive correlation (R2 = 72%, p<0.001) between discomfort and the predicted anxiety if cannulation was to be repeated with the same cream. With the placebo a positive correlation (R2 = 19.8%, p = 0.05) was found between the level of anxiety before cannulation and the level of discomfort recorded.
Conclusions Ametop and EMLA topical anaesthetic agents produce effective skin analgesia for venous cannulation. The use of topical analgesia can reduce perceived anxiety about future cannulation procedures. This has application in the management of anxious patients undergoing intravenous sedation, suggesting that topical analgesia prior to venous cannulation may significantly aid anxiolysis.
Similar content being viewed by others
Main
Anxiety associated with dental treatment is well recognised and has a negative impact on patients' willingness to attend for dental care. Dental fear is a widespread problem and presents a universal barrier to oral health care. Fears, which are acquired in childhood through direct experiences of painful treatment or vicariously through parents, siblings or friends, may persist into adulthood. Symptomatic treatment and lack of trust in dental personnel only serve to exacerbate and reinforce these fears. Up to 45% of the adult UK population claim that fear is 'a major barrier to dental care' which prevents them from seeking dental treatment.1 In order to try and help this large group of patients, techniques of conscious sedation have been developed which aim to reduce their anxiety and allow them to undergo routine dental care.
Intravenous sedation using midazolam is the mainstay of modern sedation practice in the UK and is used extensively for the management of phobic dental patients.2 Unfortunately the actual procedure of venous cannulation, which is necessary for the administration of the sedation agent, can be a significant fear-provoking stimulus for many patients. Fear of pain and especially the fear of dental and other injections are a common concern amongst dental phobics. Many of those with high anticipatory anxiety and expectation of significant pain have been found to over-predict the degree of pain and anxiety they will suffer.3 If the discrepancy between anticipated and actual discomfort is reduced then the patient's confidence has been shown to increase.3 It is therefore important that the discomfort associated with intravenous sedation is minimised in these groups of patients and they are encouraged to regard this minimised discomfort as typical of the procedure being undertaken.
There is good evidence that both adults and children benefit in terms of reduced discomfort and distress if an effective topical analgesic cream is used at the site of venepuncture.4,5 Both the eutectic mixture of the local anaesthetics 2.5% lidocaine and 2.5% prilocaine (EMLA) and the 4% amethocaine gel (Ametop) are effective at producing a reduction in patient discomfort on venepuncture and cannulation.6,7,8,9 It is recognised that the anticipation of a procedure may cause greater distress than the actual procedure itself.10 To date there have been no published works to determine whether the application of an analgesic cream leads to a reduction in patient anxiety because of an anticipated reduction in discomfort of cannulation, or whether it actually heightens anticipation of cannulation and thus increases distress.
It is certainly true that the insertion of an intra-venous cannula causes discomfort and even pain.11 It is clear that the subjective characteristics of pain involve not only the physiology of the person, but also the sum total of past experience and the totality of the present situation in which the individual finds them.12 Both emotional and psychological factors affect the central nervous systems processing of any pain signals. Arntz, Dresen and Merkelbach13 noted that there was a widely held view that anxiety increased pain perception. Their study refuted this and demonstrated that the focus of a person's attention was more important in modifying pain perception. To date, no study has looked at the anxiety associated with intravenous cannulation and its effect on pain perception. Very few studies on the pain associated with venepuncture or cannulation take any account of the level of patients' anxiety or psychological state.
The aims of the present study were to compare the topical analgesic preparations EMLA and Ametop with a non-active control cream (E45) in terms of their ability to reduce the discomfort and anticipated and actual anxiety associated with cannulation.
Method
Study Design
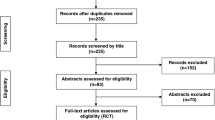
The present study was designed as a double blind, randomised, placebo-controlled, within subject, trial. Twenty healthy (ASA 1) volunteers were recruited from members of the professional dental and nursing staff at the Leeds Dental Institute, Yorkshire, England. Since no previous studies have looked at the effects of topical skin analgesia in relation to anxiety and its effects on perceived discomfort, it was difficult to calculate study numbers. Based on the results of previous studies on the use of topical anaesthetic creams to reduce the discomfort associated with venous cannulation and using a nomogram for power calculations,14 it was estimated that with a sample size of 20 there was an 85% chance of detecting a difference between experimental and control groups with a probability value of 0.05.
Subjects recruited had no history of allergic reactions to local or topical anaesthetics or any dermatological conditions. Subjects who had a history of difficulty with venepuncture or who were assessed as likely to be difficult to cannulate were excluded. Subjects, who were pregnant, thought they might be pregnant or planning to become pregnant were also excluded as were those who were breast-feeding. The ethics committee of the Leeds Teaching Hospitals NHS Trust approved the study protocol prior to recruitment of the volunteers. All volunteers gave their informed consent and were aware that one of the creams being used was a non-active control.
Clinical Procedure
Each subject was seen on three separate occasions, one week apart and a test cream applied to the dorsum of their non-dominant hand at the site chosen for venepuncture. This site was recorded and used again on the subsequent two visits. Only one attempt was made at venepuncture on each occasion using a 22-gauge, 25mm long, intra-venous cannula (Venflon2, BOC Ohmeda AB, Helsingborg, Sweden). No drugs or solutions were injected and the cannula was removed immediately after insertion. The same clinician performed all venepuncture procedures.
The test creams used on each subject were 2 g of the eutectic mixture of 2.5% lidocaine and 2.5% prilocaine (EMLA cream 5%, Astra Pharmaceuticals Ltd, Kings Langley, Hertfordshire, England), 1 g of 4% amethocaine gel (Ametop gel 4%, Smith and Nephew Healthcare Ltd, Goulton Street, Hull, England). Two grammes of the emollient cream E45 (Crookes Healthcare Ltd., Nottingham, England) were used as a non-active control. The Ametop was stored at 4°C as per the manufacturers instructions, but was allowed to return to room temperature prior to it being used.
The order in which the three creams were applied was selected randomly. There were six possible orders in which the creams could be used and each one was allocated a number from 1–6. A series of twenty random numbers from 1–6 were generated by Excel 97 (Microsoft Corporation). These random numbers were then used to allocate the order of cream application for each of the twenty subjects.
A person, other than the clinician performing cannulation, carried out all application and removal of the cream. The clinician carrying out cannulation was therefore blind to the cream being used. The occlusive dressing supplied by the manufacturers was placed over the cream to hold it in place for 45 minutes (OpSite for the Ametop and Tegaderm for the EMLA and E45). This was covered with a gauze pad so that the subjects were unaware of the nature of the cream being applied. In order to keep the subjects blind it was felt to be important to apply the creams for the same length of time. The application time of 45-minutes was chosen, as this seemed to be the minimum time that could be expected to give reliable analgesia with EMLA. The manufacturers recommend that Ametop be not applied for more than 1 hour and to give a margin for error 45-minutes seemed appropriate. Once the cream was removed, any local skin reactions such as erythema, itching or swelling were recorded.
45 minutes after application the occlusive dressing and cream were removed and a 22-gauge cannula was inserted through the skin and into a vein. The cannula was advanced fully and the needle withdrawn to ensure the cannula was correctly sited in the vein. The cannula was then removed and a cotton wool roll placed over the venepuncture site.
Pain Measurement
Subjects were asked to rate the pain/discomfort they felt during cannulation on a standard 100 mm visual analogue scale (VAS) from 0 = comfortable to 100 = very painful. They also used a verbal rating with 5 categories namely, comfortable, mild discomfort, moderate discomfort, painful and very painful. This was completed immediately after removal of the cannula.
Anxiety Measurement
Prior to application of the cream, subjects were asked to estimate how anxious they would feel if cannulation was about to be performed without any cream. 45 minutes after application of the cream they were asked to indicate how anxious they were feeling just prior to cannulation. Finally, after cannulation, they were asked to estimate how anxious they thought they would be prior to a similar cannulation procedure in the future using the same cream.
Anxiety was recorded by the subjects using a 100 mm visual analogue scale ranging from 0 = relaxed to 100 = very anxious. There were no other markings on the line used. The markings on the visual analogue scales were measured to the nearest mm. A verbal rating was also used with 5 categories namely; relaxed, mildly apprehensive, moderately apprehensive, anxious and very anxious.
Each subject also completed a standard hospital anxiety and depression questionnaire at the commencement of the study to obtain baseline information on the individual's general anxiety status (Zigmond and Snaith, 1983).
Physiological Measurement
Pulse rate, respiratory rate and arterial blood pressure were recorded prior to cream application, just before cannulation and 15 minutes after cannulation. A Biox 3740-pulse oximeter (BOC Health Care, Louisville, Colorado, USA) was used with a transilluminating finger probe to measure the pulse rate. Arterial blood pressure was measured on the left arm at heart level using a DinamapTM vital signs monitor 1846SX (Critikon Inc. Tampa, Florida, USA). The mean arterial blood pressure was calculated from the diastolic pressure plus one third of the pulse pressure. The respiratory rate was measured by observing chest movements over a 1-minute period.
Statistical Analyses
Repeated measures analysis of variance was carried out to analyse differences between pulse rate, mean arterial blood pressure, respiration rate, anxiety and discomfort. Multivariate analysis allowed comparisons between the creams used, time of measurement and appointment number. Individual subjects' visual analogue scores were matched with their verbal ratings responses. This allowed analysis of the relationship between the two scoring systems and meaningful comparisons with other studies. Differences between visual analogue scores, grouped by their corresponding verbal ratings, were analysed using an analysis of variance and pair-wise comparisons made using Tukey's method. Linear regression analysis was carried out to look at the correlation between the anxiety scores prior to cannulation vs. amount of discomfort felt during cannulation and the amount of discomfort felt during cannulation vs. the level of anxiety predicted if the same cream was used in the future. A p-value of <0.05 was considered to indicate statistical significance. Statistical packages used were SPSS for Windows (SPSS, Chicago) and Minitab (Minitab Inc. State College, PA).
Results
Study Population
Twenty fit and healthy volunteers aged from 22–53 years, mean 32.8 years (SD 8.2 years) were included in the study. There were 65% females (n = 13) and 35% males (n = 7). The majority of the subjects had white skin (95%, n = 19), with one person from India having brown skin. The baseline Hospital Anxiety and Depression (HAD) median anxiety score was 6.5 (inter-quartile range 5–7) and median depression score was 1.0 (inter-quartile range 0–1.25).
Physiological Data
The mean values for pulse rate per minute, respiratory rate per minute and mean arterial blood pressure (BP in mmHg) are displayed in Table 1. The mean pulse rate showed a very small decrease after cannulation with all three creams. This did not reach a level of statistical significance (p=0.08 for comparisons with time, p=0.63 for comparisons between different creams). The pulse rate was not found to significantly differ over the three visits (p=0.16). There was a slightly higher mean respiratory rate with E45 prior to cannulation, compared with EMLA and Ametop, but was not significant (p=0.28). The respiratory rate showed no significant differences at any other time point or between visits (p=0.74) or creams (p = 0.63). The mean arterial blood pressure showed a small reduction from just before drug application to just before cannulation with EMLA and Ametop. With E45 there was a small rise in mean arterial blood pressure from drug application to just prior to cannulation. None of these differences were found to be statistically significant nor were there significant differences between the mean arterial blood pressure at any time point (p=0.10) or between visits (p=0.21) or creams (p=0.80).
Pain Scores
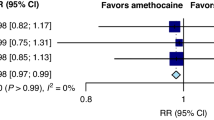
The mean VAS pain scores calculated for each cream are represented in Figure 1. The data equates to 24% less discomfort with EMLA and 53% less discomfort with Ametop compared with the non-active control cream. These differences were found to be highly significant (p < 0.001). The mean scores for each visit were first visit 30mm (SD 24mm), second visit 30mm (SD 22mm) and third visit 25mm (SD 19mm). These were not significantly different (p = 0.58). The mean verbal pain ratings are shown in Table 2. Differences in verbal pain ratings between the creams were found to be highly significant (p < 0.001). There were no significant differences between the first, second or third visits (p = 0.63).
In order to determine the relationship between the VAS and verbal ratings of pain, individual subjects' visual analogue scores were matched with their individual verbal rating responses. Individual subjects VAS scores were then pooled for each category on the verbal rating scale and the mean value and standard deviations calculated. The combined data is represented in Figure 2. One-way analysis of variance was performed and showed a highly significant difference between groups (p<0.001). Tukey's pairwise comparisons were carried out with the family error rate held at 0.05. This gave 95% confidence intervals that showed a significant difference between the VAS scores for all the verbal categories except between 'moderate discomfort' and 'painful'.
Anxiety Scores
The mean VAS anxiety scores calculated for each cream for the various times are represented in Figure 3. With E45 there was a small rise in anxiety from cream application to just before cannulation. With EMLA there was no change and with Ametop a small reduction. The levels of anxiety, which subjects would expect if the same cream were being used again, are shown in Figure 4. Anxiety increased by 32% after cannulation using E45 but with EMLA there was a reduction of 24% and with Ametop a reduction of 42%. The differences between the creams were highly significant at this third time point (p=0.003). The results of the verbal anxiety ratings just prior to cannulation are shown in Table 3 and Table 4 shows subjects' predicted verbal anxiety scores if cannulation was to be undertaken in the future using the same cream as they had just received.
In order to determine the relationship between the VAS and verbal ratings of anxiety, individual subjects' visual analogue scores were matched with their individual verbal rating responses. Individual subjects VAS scores were then pooled for each category on the verbal rating scale and the mean value and standard deviations calculated. The combined data is represented in Figure 5. A one-way analysis of variance showed a highly significant difference between the groups (p<0.001). Tukey's pairwise comparisons were carried out with the family error rate held at 0.05. This gave 95% confidence intervals that showed a significant difference between the VAS scores for all the verbal categories.
Correlation of Anxiety & Pain Data
Linear regression analysis of the VAS pain scores plotted against VAS anxiety scores just prior to cannulation was performed in order to reveal any correlation between the level of anxiety and the perception of discomfort. Plots of the E45 data gave a significant R-squared value of 19.8% (p=0.05). The slope of the line was 0.4 with a y-axis intercept value of 26.4 mm. For EMLA the R-squared value was 3.5%, which was not significant (p=0.43). The R-squared value for Ametop was 10.4%, which was also not significant (p = 0.17). With the values from the three creams pooled then no significant relationship was seen between anxiety and discomfort.
Linear regression analysis of the VAS pain scores plotted against the VAS anxiety scores after cannulation was also performed to reveal the correlation between level of discomfort and anticipated anxiety, if the same cream was being used again (Figure 6). All three creams gave highly significant results. With E45 the R-squared value was 71.8%, slope 0.9 and y-axis intercept 2.4 mm (p<0.001). EMLA gave an R-square value of 59.1%, slope of 0.56 and a y-axis intercept of 5.2 mm (p<0.001). Ametop gave an R-square value of 51.2%, slope of 0.47 and y-axis intercept of 5.4 mm (p<0.001).
Adverse Reactions
There were no adverse reactions with any subjects with the control cream E45. With EMLA, 65% (n=13) had no reaction and 35% (n=7) exhibited slight paleness of the skin. With Ametop, 60% (n=12) had no visible reactions, whilst the remaining 40% (n=8) had mild erythema at the site of application. One of the subjects with mild erythema also had mild itching at the site of application. There were no apparent systemic reactions to any of the creams. Although not formally measured, it was reported by all of the subjects that localised numbness was present for several hours with the Ametop, but had passed more quickly with the EMLA.
Discussion
In the present study both the 5% EMLA and 4% Ametop were more effective than a non-active control at reducing discomfort during cannulation. This was found to be consistent with other published studies that utilised visual analogue scales to measure discomfort. O'Connors and Tomlinson,6 using a 20 gauge cannula, found mean scores of 27 mm for the placebo cream and 7 mm with 4% amethocaine gel. This compared with 38 mm (placebo) and 18 mm (4% amethocaine) in the present study. Molodecka, Stenhouse, Jones and Tomlinson16 recorded 13.5 mm with EMLA and 8.5 mm with a 5% amethocaine gel. The corresponding value for EMLA in the present study was 29 mm. They used an 18-gauge cannula, but applied the creams for 1 hour and used a higher concentration of amethocaine.
Differences in analgesic concentration, length of time of application and size of cannula make direct comparisons between studies difficult. The only study which used similar drug application conditions to the present one, compared EMLA and 4% amethocaine gel applied for 40-minutes prior to venous cannulation with a 22-gauge cannula in the dorsum of the hand in children aged 3–12 years.17 Using a three point verbal rating scale this study found that 66% of the patients registered either mild or no discomfort. In the present study the comparable figure was 70%. With 4% amethocaine gel they found 85% had mild discomfort or no pain. The same figure was found in the present study. It is interesting that the results are comparable despite the considerable subject age differences between these two studies.
To date, no published work in this area has taken account of the subject's anxiety status. It might be expected that as the time for cannulation approached that the level of anxiety would increase. In order to examine if the application of the cream increased or decreased anxiety it was felt that the baseline for comparison should be to ask subjects prior to cream placement to estimate the level of anxiety they would be feeling if cannulation were to go ahead without any cream. It can be seen from Figure 3 that there was no significant change in the level of anxiety between the start and 45 minutes later just before cannulation. Thus, it appears that the time the subject has to wait before cannulation appears to have no influence on level of anxiety about the procedure. It should be noted that this study was undertaken on a group of volunteers who fell within normal ranges for anxiety status, as revealed by the Hospital Anxiety and Depression data.
Discomfort and anxiety were recorded in this study using both a visual analogue scale and a verbal rating scale. The visual analogue scale has been well validated and is widely used in pain research as a reliable and sensitive measure.18 Unfortunately many studies on skin analgesia and discomfort only use verbal rating scales. The verbal rating scores in the present study were included to allow meaningful comparison with other studies and also to allow the relationship between the two scoring methods to be explored. When individual visual analogue scores were compared with their corresponding verbal rating scores, the mean values for the visual analogue scores of anxiety, grouped by their corresponding verbal ratings, were found to be significantly different (Figure 5). The corresponding exercise for the discomfort score also showed that there was a significant difference between all the groups, except the 'moderate discomfort' group and the 'painful' group (Figure 2). This was useful since it took the subjective terms interpreted by each subject and attached a number that they had ascribed with the visual analogue score. If this had not been done then the difference in interpretation of 'moderate discomfort' and 'pain' would not have been revealed. Collins, Moore and McQuay19 showed that if the relationship between verbal ratings and the visual analogue scores is established, the findings of a number of studies on pain can be combined using techniques such as meta-analysis.
It was also clear that the visual analogue scores were not evenly distributed between the various verbal ratings. This was also demonstrated in a recent study by Tammaro, Berggren and Bergenholtz.20 They took five common pain descriptors and asked various groups to relate them to a visual analogue scale. They used a group of 80 dental students, 48 patients undergoing periodontal treatment and a group of 31 patients with a dental phobia. They found that there were differences in interpretation of pain descriptors between the groups, that age influenced the findings and, as in the present study, the descriptors did not divide the analogue scale equally. The findings of this and the present study suggest that when a verbal rating score is being used alone then great care needs to be taken when analysing and interpreting the results.
Although subjects in the present study reported a range of anxiety levels this was not mirrored in the measurements recorded for arterial blood pressure, pulse and respiratory rate. These might be expected to increase with increasing feelings of anxiety, but the lack of difference between the vital signs at each repeated measure is consistent with the findings in a number of studies. Lawson, Smart, Gudgeon and Morton17 found no significant change in their study on amethocaine gel in heart rate or arterial blood pressure before application of the gel and after its removal. This apparent response desynchrony was something which was seen in a study by Rachman and Hodgson.21 They frequently noted results of behavioural avoidance tests, cognitive measures and physiological measurements of anxiety were not consistent in indicating the presence of anxiety and were often poorly correlated to each other.
A strong relationship was revealed between the level of discomfort recorded and the estimated anxiety which subjects would anticipate feeling if the cannulation were repeated at a later date using the same cream. After using the non-active control cream subjects estimated that their anxiety next time would be 32% higher. However both EMLA and Ametop were effective in reducing the anticipated anxiety. With EMLA this was a reduction by 24% and with Ametop TM it was reduced by 42%. It is not clear whether reduction in anticipatory anxiety resulting from the patient being confident in the effectiveness of the analgesic cream would lead to a reduction in the subsequent use of any pharmacological sedation. It seems possible that if the main focus of an individual patient's anxiety was injections and needles then this might well be the case. It was clear from the study that if a favourable cannulation procedure is carried out with an effective analgesic cream then the level of anxiolysis for future cannulation can be expected to be significantly improved if the patient knows that the same cream is being used. This is in keeping with the study by Kent3 and suggests that anxious patients would have a more accurate expectation of the cannulation procedure once the cream has been used successfully.
There were no significant adverse effects with the analgesics creams used in this study. In keeping with other studies a proportion of subjects experienced localised erythema at the site where the amethocaine gel had been applied. Localised blanching of the skin was seen in 35% of the subjects after EMLA was used. In this study 40% of subjects experienced mild localised erythema which is close to the figure of 37% found in the study on 4% amethocaine gel by Lawson, Smart, Gudgeon and Morton.17 It might be assumed that as a consequence it would be easier to cannulate a vein after using an amethocaine gel as compared with EMLA.
In conclusion, this study demonstrated that Ametop produced a reliable reduction in the discomfort felt during venous cannulation. A 45-minute application of EMLA produced a significant reduction in discomfort, although not as great. There was a strong correlation between the degree of discomfort felt and the subjects predicted anxiety before future cannulation procedures using the same cream. There did not appear to be a significant relationship between the level of anxiety before cannulation and the degree of discomfort felt and there was no obvious change in anxiety from the time the cream was applied up to the time of cannulation.
References
Todd J E, and Lader D (1991). Adult Dental Health, 1988. London: HMSO.
Girdler N M, Hill C M (1998). Sedation in dentistry. Butterworth Heinemann. Oxford.
Kent G . The typicality of therapeutic 'surprises'. Behaviour, Research and Therapy 1986; 24: 625–628.
Hallén B, Carlsson P, Uppfeldt A . Clinical study of a lignocaine-prilocaine cream to relieve the pain of venepuncture. Br J Anaesth. 1985; 57: 326–328.
Manner T, Kanto J, Iisalo E, Lindberg R, Viinamaki O et al. Reduction of pain at venous cannulation in children with a eutectic mixture of lidocaine and prilocaine (EMLA cream): comparison with placebo cream and no local premedication. Acta Anaesthesiologica Scandinavica 1987; 31: 735–739.
O'Connors B, Tomlinson A A . Evaluation of the efficacy and safety of amethocaine gel applied topically before venous cannulation in adults. Br J Anaesth. 1995; 74: 706–708.
McCafferty D F, Woolfson A D, Boston V . In vivo assessment of percutaneous local anaesthetic preparations. Br J Anaesth. 1989; 62: 17–21.
Ravey T, Weinberg M D, Sibirsky O, Caspi MD, Moor EV et al. Efficacy of the Topical Anaesthetic Cream, EMLA, in Alleviating Both Needle Insertion and Injection Pain. Annals of Plastic Surgery 35 1995 576–579.
Riendeau L A, Bennett D, Black-Noller G et al. Evaluation of the analgesic efficacy of EMLA cream in volunteers with differing skin pigmentation undergoing venepuncture. Regional Anesthesia and Pain Medicine 1999; 24: 165–169.
Corah N L, Gale E N, Illig S J . Assessment of a dental anxiety scale. JADA. 1981; 97: 816.
Langham B T and Harrison D A . Local anaesthetic: does it really reduce the pain of insertion of all sizes of venous cannulae?. Anaesthesia 1992 47: 890–891.
Vingoe F J . Clinical Psychology and Medicine: An Interdisciplinary Approach. 1981 Oxford University Press, Oxford.
Arntz A, Dreessen L, Merckelbach H . Attention, not anxiety, influences pain. Behaviour, Research and Therapy 1991 29: 41–50.
Altman D . How large a sample?. In Statistics in Practice. Gore S, Altman D. (eds) 1982 British Medical Association.
Zigmond A S, Snaith R P . The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand 1983; 67: 361–370.
Molodecka J, Stenhouse C, Jones J M, Tomlinson A . Comparison of percutaneous anaesthesia for venous cannulation after topical application of either amethocaine or EMLA cream. Br J Anaesth.; 1995.; 72: 174–176.
Lawson R A, Smart N G, Gudgeon A C, Morton N S . Evaluation of a gel preparation for percutaneous analgesia before venous cannulation in children. Br J Anaesth. 1995; 75: 282–285.
Revill S I, Robinson J O, Rosen M, Hogg M I J . The reliability of a linear analogue for evaluating pain. Anaesthesia 1976; 31: 1191–1198.
Collins S L, Moore R A, McQuay H J . The visual analogue pain intensity scale: what is moderate pain in millimetres?. Pain 1997; 72: 95–97.
Tammaro S, Berggren U, Bergenholtz G . Representation of verbal pain descriptors on a visual analogue scale by dental patients and dental students. European Journal of Oral Sciences. 1997; 105: 207–212.
Rachman S, Hodgson RI . Synchrony and desynchrony in fear and avoidance. Behaviour, Research and Therapy 1974; 12: 311–318.
Acknowledgements
The authors would like to express their thanks to the volunteers for their participation in this study. This research was undertaken as a component of the Diploma in Concious Sedation run by the Northern Region Postgraduate Institute of Medicine and Dentistry of the University of Newcastle. The first author would like to express his thanks to Professor J. P. Ralph, Postgraduate Dental Dean for Yorkshire for his generous support which allowed this work to be undertaken.
Author information
Authors and Affiliations
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Speirs, A., Taylor, K., Joanes, D. et al. A randomised, double-blind, placebo-controlled, comparative study of topical skin analgesics and the anxiety and discomfort associated with venous cannulation. Br Dent J 190, 444–449 (2001). https://doi.org/10.1038/sj.bdj.4800999
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800999
This article is cited by
-
Comparison of the use of the Valsalva maneuver and the eutectic mixture of local anesthetics (EMLA®) to relieve venipuncture pain: a randomized controlled trial
Journal of Anesthesia (2013)
-
Valsalva manoeuvre and the wrist block
European Journal of Plastic Surgery (2011)
-
Highly anxious dental patients report more pain during dental injections
British Dental Journal (2008)
-
Beyond halothane: an update on pediatric anesthesia pharmacology
Canadian Journal of Anesthesia/Journal canadien d'anesthésie (2003)
-
A study of topical skin analgesics
British Dental Journal (2001)