Abstract
Objectives
To investigate the changes in the temporal vascular angles after epiretinal membrane (ERM) surgery and utilize the angles to predict visual outcomes.
Methods
A total of 168 eyes from 84 patients with unilateral ERM who underwent vitrectomy were enrolled from a single institution. The angles of temporal venous (anglevein) and arterial arcades (angleartery) were measured on fundus photographs. The relationships between the angles and the best-corrected visual acuity (BCVA) were explored and multivariable logistic models and receiver operating characteristic (ROC) curves were analyzed to identify the factors that predicted visual outcomes.
Results
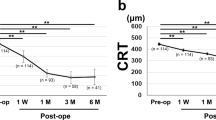
At baseline, both angleartery and anglevein were narrower in the eyes with ERM than the fellow eyes (p < 0.001 and 0.007) but had no correlation with the baseline BCVA (p = 0.754 and 0.804). Postoperatively, the angleartery and anglevein significantly widened (both p < 0.001) and a greater BCVA improvement was associated with a greater widening of the angleartery (p = 0.029) and anglevein (p = 0.050). Multivariable logistic analyses found a narrower baseline angleartery compared to the fellow eye had a higher chance for BCVA improvement ≧ 2 lines (Odds ratio = 0.97; 95% CI, 0.94–0.99; p = 0.016). ROC curve showed the baseline difference in the angleartery between bilateral eyes predicted BCVA improvement ≧ 2 lines (area under the curve = 0.74; p = 0.035), and a 0.73 sensitivity and 0.80 specificity with a cut-off value of −27.19 degrees.
Conclusions
The retinal vascular angles widened after ERM surgery and the fundus photograph-derived angles may serve as a highly-accessible biomarker to predict postoperative visual outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Data supporting the findings of the current study are available from the corresponding author on reasonable request.
References
Smiddy WE, Maguire AM, Green WR, Michels RG, de la Cruz Z, Enger C, et al. Idiopathic epiretinal membranes. Ultrastructural characteristics and clinicopathologic correlation. Ophthalmology. 1989;96:811–20.
Kim JH, Kim YM, Chung EJ, Lee SY, Koh HJ. Structural and functional predictors of visual outcome of epiretinal membrane surgery. Am J Ophthalmol. 2012;153:103–10.
Fung AT, Galvin J, Tran T. Epiretinal membrane: A review. Clin Exp Ophthalmol. 2021;49:289–308.
Chen X, Klein KA, Shah CP, Heier JS. Progression to Surgery for Patients With Idiopathic Epiretinal Membranes and Good Vision. Ophthalmic Surg Lasers Imaging Retin. 2018;49:S18–22.
Dawson SR, Shunmugam M, Williamson TH. Visual acuity outcomes following surgery for idiopathic epiretinal membrane: an analysis of data from 2001 to 2011. Eye (London). 2014;28:219–24.
Matoba R, Morizane Y. Surgical Treatment of Epiretinal Membrane. Acta Med Okayama. 2021;75:403–13.
Miliatos I, Lindgren G. Epiretinal membrane surgery evaluated by subjective outcome. Acta Ophthalmol. 2017;95:52–9.
Scheerlinck LM, van der Valk R, van Leeuwen R. Predictive factors for postoperative visual acuity in idiopathic epiretinal membrane: a systematic review. Acta Ophthalmol. 2015;93:203–12.
Coppola M, Brambati M, Cicinelli MV, Marchese A, Zanzottera EC, Peroglio Deiro A, et al. The visual outcomes of idiopathic epiretinal membrane removal in eyes with ectopic inner foveal layers and preserved macular segmentation. Graefes Arch Clin Exp Ophthalmol. 2021;259:2193–201.
Feng J, Yang X, Xu M, Wang Y, Shi X, Zhang Y, et al. Association of Microvasculature and Macular Sensitivity in Idiopathic Macular Epiretinal Membrane: Using OCT Angiography and Microperimetry. Front Med (Lausanne). 2021;8:655013.
Weinberger D, Stiebel-Kalish H, Priel E, Barash D, Axer-Siegel R, Yassur Y. Digital red-free photography for the evaluation of retinal blood vessel displacement in epiretinal membrane. Ophthalmology. 1999;106:1380–3.
Yang HK, Kim SJ, Jung YS, Kim KG, Kim JH, Yu HG. Improvement of horizontal macular contraction after surgical removal of epiretinal membranes. Eye (London). 2011;25:754–61.
Nagura K, Inoue T, Zhou HP, Obata R, Asaoka R, Arasaki R, et al. Association between retinal artery angle and visual function in eyes with idiopathic epiretinal membrane. Transl Vis Sci Technol. 2021;10:35.
Govetto A, Lalane RA 3rd, Sarraf D, Figueroa MS, Hubschman JP. Insights into epiretinal membranes: presence of ectopic inner foveal layers and a new optical coherence tomography staging scheme. Am J Ophthalmol. 2017;175:99–113.
Govetto A, Virgili G, Rodriguez FJ, Figueroa MS, Sarraf D, Hubschman JP. Functional and anatomical significance of the ectopic inner foveal layers in eyes with idiopathic epiretinal membranes: surgical results at 12 months. Retina. 2019;39:347–57.
González-Saldivar G, Berger A, Wong D, Juncal V, Chow DR. Ectopic Inner Foveal Layer Classification Scheme Predicts Visual Outcomes After Epiretinal Membrane Surgery. Retina. 2020;40:710–7.
Mavi Yildiz A, Avci R, Yilmaz S. The predictive value of ectopic inner retinal layer staging scheme for idiopathic epiretinal membrane: surgical results at 12 months. Eye (Lond). 2021;35:2164–72.
Kim BH, Kim DI, Bae KW, Park UC. Influence of postoperative ectopic inner foveal layer on visual function after removal of idiopathic epiretinal membrane. PLoS One. 2021;16:e0259388.
Mahmoudzadeh R, Israilevich R, Salabati M, Hsu J, Garg SJ, Regillo CD, et al. Pars plana vitrectomy for idiopathic epiretinal membrane: oct biomarkers of visual outcomes in 322 Eyes. Ophthalmol Retin. 2022;6:308–17.
Kunavisarut P, Supawongwattana M, Patikulsila D, Choovuthayakorn J, Watanachai N, Chaikitmongkol V, et al. Idiopathic epiretinal membranes: visual outcomes and prognostic factors. Turk J Ophthalmol. 2022;52:109–18.
Lee MW, Jung I, Song YY, Baek SK, Lee YH. Long-term outcome of epiretinal membrane surgery in patients with internal limiting membrane dehiscence. J Clin Med. 2020;9:2470.
Jeon S, Jung B, Lee WK. Long-term prognostic factors for visual improvement after epiretinal membrane removal. Retina. 2019;39:1786–93.
Zhmurin R, Grajewski L, Krause L. Influence of preoperative foveal layers’ Thickness on Visual Function and Macular Morphology by Phacovitrectomy for Epiretinal Membrane. J Ophthalmol. 2022;2022:1895498.
Doguizi S, Sekeroglu MA, Ozkoyuncu D, Omay AE, Yilmazbas P. Clinical significance of ectopic inner foveal layers in patients with idiopathic epiretinal membranes. Eye (Lond). 2018;32:1652–60.
Kaplan RI, Chen M, Gupta M, Rosen RB. Impact of automated OCT in a high-volume eye urgent care setting. BMJ Open Ophthalmol. 2019;4:e000187.
Gupta P, Sadun AA, Sebag J. Multifocal retinal contraction in macular pucker analyzed by combined optical coherence tomography/scanning laser ophthalmoscopy. Retina. 2008;28:447–52.
Mase T, Ishibazawa A, Nagaoka T, Yokota H, Yoshida A. Radial peripapillary capillary network visualized using wide-field montage optical coherence tomography angiography. Invest Ophthalmol Vis Sci. 2016;57:504–10.
Iwase T, Ra E, Yamamoto K, Kaneko H, Ito Y, Terasaki H. Differences of retinal blood flow between arteries and veins determined by laser speckle flowgraphy in healthy subjects. Med (Baltim). 2015;94:e1256.
Matsopoulos GK, Asvestas PA, Delibasis KK, Mouravliansky NA, Zeyen TG. Detection of glaucomatous change based on vessel shape analysis. Comput Med Imaging Graph. 2008;32:183–92.
Liu R, Li Q, Xu F, Wang S, He J, Cao Y, et al. Application of artificial intelligence-based dual-modality analysis combining fundus photography and optical coherence tomography in diabetic retinopathy screening in a community hospital. Biomed Eng Online. 2022;21:47.
Rodenbeck SJ, Mackay DD. Examining the ocular fundus in neurology. Curr Opin Neurol. 2019;32:105–10.
Beduk T, Beduk D, Hasan MR, Guler Celik E, Kosel J, Narang J, et al. Smartphone-Based Multiplexed Biosensing Tools for Health Monitoring. Biosens (Basel). 2022;12:583.
Fraser-Bell S, Symes R, Vaze A. Hypertensive eye disease: a review. Clin Exp Ophthalmol. 2017;45:45–53.
Wagner-Schuman M, Dubis AM, Nordgren RN, Lei Y, Odell D, Chiao H, et al. Race- and sex-related differences in retinal thickness and foveal pit morphology. Invest Ophthalmol Vis Sci. 2011;52:625–34.
Kashani AH, Zimmer-Galler IE, Shah SM, Dustin L, Do DV, Eliott D, et al. Retinal thickness analysis by race, gender, and age using Stratus OCT. Am J Ophthalmol. 2010;149:496–502.
Asano S, Yamashita T, Asaoka R, Fujino Y, Murata H, Terasaki H, et al. Retinal vessel shift and its association with axial length elongation in a prospective observation in Japanese junior high school students. PLoS One. 2021;16:e0250233.
Author information
Authors and Affiliations
Contributions
HDC, YCC: writing the manuscript, analysing the results, and interpreting the data. EYCK, YHC, LL, KJC, YSH, ANC, WCW, CCL: data collection. HDC, YCC, PYW: data processing. HDC, YCC: conception and design of the work. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chou, HD., Chang, YC., Wu, PY. et al. Retinal vascular arcade angle as a biomarker for visual improvement after epiretinal membrane surgery. Eye 38, 778–785 (2024). https://doi.org/10.1038/s41433-023-02776-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02776-6