Abstract
Purpose
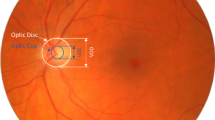
To present a new structural biomarker for detecting glaucoma progression based on structural transformation of the optic nerve head (ONH) region over time.
Methods
Dense ONH deformation was estimated using deep learning methods namely DDCNet-Multires, FlowNet2, and FlowNetCorrelation, and legacy computational methods namely the topographic change analysis (TCA) and proper orthogonal decomposition (POD) methods. A candidate biomarker was estimated as the average magnitude of deformation of the ONH and evaluated using longitudinal confocal scans of 12 laser treated and 12 contralateral normal eyes of 12 primates from the LSU Experimental Glaucoma Study (LEGS); and 36 progressing eyes and 21 longitudinal normal eyes from the UCSD Diagnostic Innovations in Glaucoma Study (DIGS). Area under the ROC curve (AUC) was used to assess the diagnostic accuracy of the biomarker.
Results
AUROC (95% CI) for LEGS were: 0.83 (0.79, 0.88) for DDCNet-Multires; 0.83 (0.78, 0.88) for FlowNet2; 0.83 (0.78, 0.88) for FlowNet-Correlation; 0.94 (0.91, 0.97) for POD; and 0.86 (0.82, 0.91) for TCA methods. For DIGS: 0.89 (0.80, 0.97) for DDCNet-Multires; 0.82 (0.71, 0.93) for FlowNet2; 0.93 (0.86, 0.99) for FlowNet-Correlation; 0.86 (0.76, 0.96) for POD; and 0.86 (0.77, 0.95) for TCA methods. Lower diagnostic accuracy of the learning-based methods for LEG study eyes were due to image alignment errors in confocal sequences.
Conclusion
Deep learning methods trained to estimate generic deformation were able to estimate ONH deformation from image sequences and provided a higher diagnostic accuracy. Our validation of the biomarker using ONH sequences from controlled experimental conditions confirms the diagnostic accuracy of the biomarkers observed in the clinical population. Performance can be further improved by fine-tuning these networks using ONH sequences.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Raw imaging data used in this study were obtained from Dr Claude F. Burgoyne and Dr Linda Zangwill without any intent to redistribute these data or make them public. Datasets are available from the authors upon request and with permission from Drs Burgoyne and Zangwill.
References
Yang H, Reynaud J, Lockwood H, Williams G, Hardin C, Reyes L, et al. The connective tissue phenotype of glaucomatous cupping in the monkey eye - Clinical and research implications. Prog Retin Eye Res. 2017;59:1–52.
Fry LE, Fahy E, Chrysostomou V, Hui F, Tang J, van Wijngaarden P, et al. The coma in glaucoma: retinal ganglion cell dysfunction and recovery. Prog Retin Eye Res. 2018;65:77–92.
Hopkins AA, Murphy R, Irnaten M, Wallace DM, Quill B, O’Brien C. The role of lamina cribrosa tissue stiffness and fibrosis as fundamental biomechanical drivers of pathological glaucoma cupping. Am J Physiol-Cell Physiol. 2020;319:C611–23.
Weinreb RN, Kaufman PL. Glaucoma research community and FDA look to the future, II: NEI/FDA Glaucoma Clinical Trial Design and Endpoints Symposium: measures of structural change and visual function. Investig Ophthalmol Vis Sci. 2011;52:7842–51.
Jonas JB, Budde WM. Diagnosis and pathogenesis of glaucomatous optic neuropathy: Morphological aspects. Prog Retin Eye Res. 2000;19:1–40.
Weinreb RN, Khaw PT. Primary open-angle glaucoma. Lancet 2004;363:1711–20.
Burgoyne CF, Yang H, Downs JC. Clinical cupping: laminar and prelaminar components. In: Schacknow P, Samples J, editors. The Glaucoma Book. New York, NY: Springer; 2010. p. 185–94.
Weinreb RN, Aung T, Medeiros FA. The Pathophysiology and Treatment of Glaucoma: A Review. JAMA. 2014;311:1901–11.
Chauhan BC, Blanchard JW, Hamilton DC, LeBlanc RP. Technique for detecting serial topographic changes in the optic disc and peripapillary retina using scanning laser tomography. Investig Ophthalmol Vis Sci. 2000;41:775–82.
Balasubramanian M, Kriegman DJ, Bowd C, Holst M, Weinreb RN, Sample PA, et al. Localized glaucomatous change detection within the proper orthogonal decomposition framework. Investig Ophthalmol Vis Sci. 2012;53:3615–28.
Balasubramanian M, Bowd C, Weinreb RN, Vizzeri G, Alencar LM, Sample PA, et al. Clinical evaluation of the proper orthogonal decomposition framework for detecting glaucomatous changes in human subjects. Investig Ophthalmol Vis Sci. 2010;51:264–71.
Talukder A, Matthies L. Real-time detection of moving objects from moving vehicles using dense stereo and optical flow. In: 2004 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS) (IEEE Cat. No. 04CH37566). 2004;4:3718–25.
Menze M, Geiger A. Object scene flow for autonomous vehicles. In: Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition. 2015;3061–70.
Chivers K, Clocksin W. Inspection of Surface Strain in Materials using Optical Flow. In BMVC. 2000;1–10.
Pitter MC, See CW, Somekh MG. Subpixel microscopic deformation analysis using correlation and artificial neural networks. Opt Express. 2001;8:322–7.
Wang CC, Deng JM, Ateshian GA, Hung CT. An automated approach for direct measurement of two-dimensional strain distributions within articular cartilage under unconfined compression. J Biomech Eng. 2002;124:557–67.
Abrámoff MD, Niessen WJ, Viergever MA. Objective quantification of the motion of soft tissues in the orbit. IEEE Trans Med Imaging. 2000;19:986–95.
Durig B, Peters W, Hammer M. Digital image correlation measurements of strain in bovine retina. In: Optical Testing and Metrology II. International Society for Optics and Photonics. 1989;954:438–44.
Balasubramanian M. A Computational Framework for the Structural Change Analysis of 3D Volumes of Microscopic Specimens. PhD Dissertation, Louisiana State University; 2006.
Tistarelli M, Marcenaro G. Using optical flow to analyze the motion of human body organs from bioimages. In: Proceedings of IEEE Workshop on Biomedical Image Analysis. 1994;100–9.
Lamberti C, Bulgarelli F, Sgallari F. Optical flow computation in 2-D echocardiography. In Proceedings Computers in Cardiology; 1991;489–92.
Loncaric S, Majcenic Z. Optical flow algorithm for cardiac motion estimation. In: Proceedings of the 22nd Annual International Conference of the IEEE Engineering in Medicine and Biology Society (Cat. No. 00CH37143); 2000;1:415–7.
Badrinarayanan V, Kendall A, Cipolla R. Segnet: A deep convolutional encoder-decoder architecture for image segmentation. IEEE Trans Pattern Anal Mach Intell. 2017;39:2481–95.
Dosovitskiy A, Fischer P, Ilg E, Hausser P, Hazirbas C, Golkov V, et al. Flownet: Learning optical flow with convolutional networks. In: Proceedings of the IEEE International Conference on Computer Vision. 2015;2758–66.
Teney D, Hebert M. Learning to extract motion from videos in convolutional neural networks. In: Asian Conference on Computer Vision. Springer. 2016;412–28.
Heeger DJ. Optical flow using spatiotemporal filters. Int J Comput Vis. 1988;1:279–302.
Goldbaum MH, Lee I, Jang G, Balasubramanian M, Sample PA, Weinreb RN, et al. Progression of patterns (POP): a machine classifier algorithm to identify glaucoma progression in visual fields. Investig Ophthalmol Vis Sci. 2012;53:6557–67.
Burgoyne CF, Thompson HW, Mercante DE, Amin R, Lemij H, Schuman J. Basic issues in the sensitive and specific detection of optic nerve head surface change within longitudinal LDT TopSS images: Introduction to the LSU Experimental Glaucoma (LEG) study. In: Lemij HG, Schuman JS, editors. The Shape of Glaucoma, Quantitative Neural Imaging Techniques. The Hague: Kugler; 2000. p. 1–37.
Balasubramanian M, Zabic S, Bowd C, Thompson HW, Wolenski P, Iyengar SS, et al. A framework for detecting glaucomatous progression in the optic nerve head of an eye using proper orthogonal decomposition. IEEE Trans Inf Technol Biomed. 2009;13:781–93.
Burgoyne CF, Mercante DE, Thompson HW. Change detection in regional and volumetric disc parameters using longitudinal confocal scanning laser tomography. Ophthalmology 2002;109:455–66.
Balasubramanian M, Arias-Castro E, Medeiros FA, Kriegman DJ, Bowd C, Weinreb RN, et al. Detecting Glaucoma Progression from Localized Rates of Retinal Changes in Parametric and Nonparametric Statistical Framework With Type I Error Control. Investig Ophthalmol Vis Sci. 2014;55:1684–95.
Ilg E, Mayer N, Saikia T, Keuper M, Dosovitskiy A, Brox T. Flownet 2.0: Evolution of optical flow estimation with deep networks. In: Proceedings of the IEEE conference on computer vision and pattern recognition. 2017:2462–70.
Salehi A, Balasubramanian M. DDCNet: Deep dilated convolutional neural network for dense prediction. Neurocomputing 2023;523:116–29.
Salehi A, Balasubramanian M. DDCNet-Multires: Effective Receptive Field Guided Multiresolution CNN for Dense Prediction. Neural Proc Lett. 2022:1–25.
Salehi A, Balasubramanian M. Dense Optic Nerve Head Deformation Estimated using CNN as a Structural Biomarker of Glaucoma Progression. Investig Ophthalmol Vis Sci. 2021;62:1851.
Mayer N, Ilg E, Hausser P, Fischer P, Cremers D, Dosovitskiy A, et al. A large dataset to train convolutional networks for disparity, optical flow, and scene flow estimation. In: Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition. 2016:4040–8.
Butler DJ, Wulff J, Stanley GB, Black MJ. A naturalistic open source movie for optical flow evaluation. In: Fitzgibbon A et al., editors. European Conf. on Computer Vision (ECCV). Part IV, LNCS 7577. Springer-Verlag; 2012. p. 611–25.
Geiger A, Lenz P, Stiller C, Urtasun R. Vision meets robotics: The KITTI dataset. Int J Robot Res. 2013;32:1231–7.
Baker S, Scharstein D, Lewis J, Roth S, Black MJ, Szeliski R. A database and evaluation methodology for optical flow. Int J Comput Vis. 2011;92:1–31.
Coleman A, Friedman D, Gandolfi S, Singh K, Tuulonen A, Weinreb R, et al. Levels of evidence in diagnostic studies. Glaucoma Diagnosis: Structure and Function The Hauge. The Netherlands: Kugler Publications; 2004. p. 9–12.
Vermeer KA, Lemij HG. Challenges in estimating the accuracy of imaging-based detection methods for glaucomatous progression. Br J Ophthalmol. 2013;97:385–6.
O’Leary N, Crabb DP, Garway-Heath DF. An in silico model of scanning laser tomography image series: an alternative benchmark for the specificity of progression algorithms. Investig Ophthalmol Vis Sci. 2010;51:6472–82.
Vermeer KA, Vos FM, Lo B, Zhou Q, Lemij HG, Vossepoel AM, et al. Modeling of scanning laser polarimetry images of the human retina for progression detection of glaucoma. IEEE Trans Med imaging. 2006;25:517–28.
Burgoyne CF, Downs JC, Bellezza AJ, Suh JKF, Hart RT. The optic nerve head as a biomechanical structure: a new paradigm for understanding the role of IOP-related stress and strain in the pathophysiology of glaucomatous optic nerve head damage. Prog Ret Eye Res. 2005;24:39–73.
Downs JC, Roberts MD, Burgoyne CF. The mechanical environment of the optic nerve head in glaucoma. Optom Vis Sci: Off Publ Am Acad Optom. 2008;85:425.
Harwerth R, Wheat J, Fredette M, Anderson D. Linking structure and function in glaucoma. Prog Ret Eye Res. 2010;29:249–71.
Schreier H, Orteu JJ, Sutton MA. Image correlation for shape, motion and deformation measurements: Basic concepts, theory and applications. Boston, MA: Springer-Verlag US; 2009.
Sutton MA, Wolters W, Peters W, Ranson W, McNeill S. Determination of displacements using an improved digital correlation method. Image Vis Comput. 1983;1:133–9.
Sutton M, Mingqi C, Peters W, Chao Y, McNeill S. Application of an optimized digital correlation method to planar deformation analysis. Image Vis Comput. 1986;4:143–50.
Coudrillier B, Campbell IC, Read AT, Geraldes DM, Vo NT, Feola A, et al. Effects of peripapillary scleral stiffening on the deformation of the lamina cribrosa. Investig Ophthalmol Vis Sci. 2016;57:2666–77.
Pyne JD, Genovese K, Casaletto L, Vande, Geest JP. Sequential digital image correlation for mapping human posterior sclera and optic nerve head deformation. J Biomech Eng. 2014;136:021002.
Girard MJ, Strouthidis NG, Desjardins A, Mari JM, Ethier CR. In vivo optic nerve head biomechanics: performance testing of a three-dimensional tracking algorithm. J R Soc Interfac. 2013;10:20130459.
Girard MJ, Beotra MR, Chin KS, Sandhu A, Clemo M, Nikita E, et al. In vivo 3-dimensional strain mapping of the optic nerve head following intraocular pressure lowering by trabeculectomy. Ophthalmology 2016;123:1190–200.
Balasubramanian M, Salehi A. Optic nerve head elastography (ONH) for detecting glaucoma progression. Investig Ophthalmol Vis Sci. 2021;62:1837–1837.
Morgan WH, Chauhan BC, Yu DY, Cringle SJ, Alder VA, House PH. Optic disc movement with variations in intraocular and cerebrospinal fluid pressure. Investig Ophthalmol Vis Sci. 2002;43:3236–42.
Agoumi Y, Sharpe GP, Hutchison DM, Nicolela MT, Artes PH, Chauhan BC. Laminar and prelaminar tissue displacement during intraocular pressure elevation in glaucoma patients and healthy controls. Ophthalmology 2011;118:52–9.
Glidai Y, Lucy KA, Schuman JS, Alexopoulos P, Wang B, Wu M, et al. Microstructural Deformations Within the Depth of the Lamina Cribrosa in Response to Acute In Vivo Intraocular Pressure Modulation. Investig Ophthalmol Vis Sci. 2022;63:25–25.
Wallace DM, O’Brien CJ. The role of lamina cribrosa cells in optic nerve head fibrosis in glaucoma. Exp Eye Res. 2016;142:102–9.
Acknowledgements
The authors thank Claude F. Burgoyne, M.D., Devers Eye Institute, Portland, OR for providing us with the LEG study topographic library; and Linda Zangwill, Ph.D., University of California San Diego, San Diego, CA for providing us with the clinical DIGS dataset for evaluating the candidate biomarkers of glaucoma progression developed in this work. The contents presented here are solely the responsibility of the authors and do not necessarily represent the official views of the funding agencies.
Funding
Research supported in part by an unrestricted startup fund and a Herff graduate fellowship, Herff College of Engineering, The University of Memphis; and a summer student fellowship from Fight for Sight.
Author information
Authors and Affiliations
Contributions
AS contributed to the following areas: Conceptualisation, methodology, software, validation, formal analysis, investigation, data curation, writing—original draft, writing—review & editing, visualisation. MB contributed to the following areas: Conceptualisation, methodology, software, validation, formal analysis, investigation, resources, data curation, writing—original draft, writing—review & editing, supervision, project administration, and funding acquisition.
Corresponding author
Ethics declarations
Competing interests
AS–None; MB–None.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Salehi, A., Balasubramanian, M. Dense optic nerve head deformation estimated using CNN as a structural biomarker of glaucoma progression. Eye 37, 3819–3826 (2023). https://doi.org/10.1038/s41433-023-02623-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02623-8