Abstract
Background
The non-human primate (NHP) model is ideal for pre-clinical testing of novel therapies for human retinal diseases due to its similarity to the human visual system. However, intra-ocular delivery of gene therapy or cell transplantation to the retina gets hampered by the sticky vitreous body and poorly permeable inner limiting membrane (ILM) in primates. Although vitrectomy and ILM peeling are commonly performed in patients, many pitfalls exist in carrying out these procedures in the rhesus macaque, which have not been reported previously.
Methods
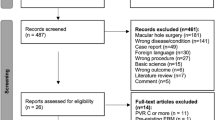
We summarised common surgical pitfalls after performing vitrectomy and ILM peeling in four eyes of two rhesus macaques (one male and one female). We provided corresponding hands-on technical tips based on our surgical experience and literature search. Orbital CT scans were compared between adult rhesus macaques and humans. High-resolution surgical videos were recorded to demonstrate each critical surgical step.
Results
Due to size difference, poor post-operative compliance, and high-standard requirements of a controlled experiment, there were eleven common surgical pitfalls during vitrectomy and ILM peeling in rhesus macaque. Falling into these pitfalls may produce discomfort, add fatigue, cause surgical complications, or even lead to the exclusion of the NHP from an experimental group.
Conclusion
Recognition and circumvention of these pitfalls during vitrectomy and ILM peeling in NHP are essential. By focusing on these surgical pitfalls, we can better carry out preclinical tests of novel therapies for retinal diseases in the NHP model.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Data available within the article or its supplementary materials.
References
Picaud S, Dalkara D, Marazova K, Goureau O, Roska B, Sahel JA. The primate model for understanding and restoring vision. Proc Natl Acad Sci USA. 2019;116:26280–7.
Peng YR, Shekhar K, Yan W, Herrmann D, Sappington A, Bryman GS, et al. Molecular classification and comparative taxonomics of foveal and peripheral cells in primate retina. Cell. 2019;176:1222–37.
Jeffery G, Levitt JB, Cooper HM. Segregated hemispheric pathways through the optic chiasm distinguish primates from rodents. Neuroscience. 2008;157:637–43.
Friedli L, Rosenzweig ES, Barraud Q, Schubert M, Dominici N, Awai L, et al. Pronounced species divergence in corticospinal tract reorganization and functional recovery after lateralized spinal cord injury favors primates. Sci Transl Med. 2015;7:302ra134.
Peynshaert K, Devoldere J, Minnaert AK, De Smedt SC, Remaut K. Morphology and composition of the inner limiting membrane: species-specific variations and relevance toward drug delivery research. Curr Eye Res. 2019;44:465–75.
Zhang KY, Johnson TV. The internal limiting membrane: Roles in retinal development and implications for emerging ocular therapies. Exp Eye Res. 2021;206:108545.
Tshilenge KT, Ameline B, Weber M, Mendes-Madeira A, Nedellec S, Biget M, et al. Vitrectomy before intravitreal injection of AAV2/2 vector promotes efficient transduction of retinal ganglion cells in dogs and nonhuman primates. Hum Gene Ther Methods. 2016;27:122–34.
Peynshaert K, Devoldere J, De Smedt SC, Remaut K. In vitro and ex vivo models to study drug delivery barriers in the posterior segment of the eye. Adv Drug Deliv Rev. 2018;126:44–57.
Johnson TV, Bull ND, Hunt DP, Marina N, Tomarev SI, Martin KR. Neuroprotective effects of intravitreal mesenchymal stem cell transplantation in experimental glaucoma. Investigative Ophthalmol Vis Sci. 2010;51:2051–9.
Gamlin PD, Alexander JJ, Boye SL, Witherspoon CD, Boye SE. SubILM injection of AAV for gene delivery to the retina. Methods Mol Biol. 2019;1950:249–62.
Nguyen CL, Oh LJ, Wong E, Francis IC. Povidone-iodine 3-minute exposure time is viable in preparation for cataract surgery. Eur J Ophthalmol. 2017;27:573–6.
Siqueira RC, Dos Santos WF, Scott IU, Messias A, Rosa MN, Fernandes Cunha GM, et al. Neuroprotective effects of intravitreal triamcinolone acetonide and dexamethasone implant in rabbit retinas after pars plana vitrectomy and silicone oil injection. Retina. 2015;35:364–70.
Konstantinidis L, Berguiga M, Beknazar E, Wolfensberger TJ. Anatomic and functional outcome after 23-gauge vitrectomy, peeling, and intravitreal triamcinolone for idiopathic macular epiretinal membrane. Retina. 2009;29:1119–27.
Li Y, Wolf MD, Kulkarni AD, Bell J, Chang JS, Nimunkar A, et al. In situ tremor in vitreoretinal surgery. Hum Factors. 2021;63:1169–81.
Zurawski CA, McCarey BE, van Rij G, Fernandes A. Corneal biometrics of the rhesus monkey (Macaca mulatta). J Med Primatol. 1989;18:461–6.
Zamora JL. Chemical and microbiologic characteristics and toxicity of povidone-iodine solutions. Am J Surg. 1986;151:400–6.
Jiang J, Wu M, Shen T. The toxic effect of different concentrations of povidone iodine on the rabbit’s cornea. Cutan Ocul Toxicol. 2009;28:119–24.
Speaker MG, Menikoff JA. Prophylaxis of endophthalmitis with topical povidone-iodine. Ophthalmology. 1991;98:1769–75.
Warrier SK, Jain R, Gilhotra JS, Newland HS. Sutureless vitrectomy. Indian J Ophthalmol. 2008;56:453–8.
López-Guajardo L, Pareja-Esteban J, Teus-Guezala MA. Oblique sclerotomy technique for prevention of incompetent wound closure in transconjunctival 25-gauge vitrectomy. Am J Ophthalmol. 2006;141:1154–6.
Yamane S, Kadonosono K, Inoue M, Kobayashi S, Watanabe Y, Arakawa A. Effect of intravitreal gas tamponade for sutureless vitrectomy wounds: three-dimensional corneal and anterior segment optical coherence tomography study. Retina. 2011;31:702–6.
Kanclerz P, Grzybowski A. Complications associated with the use of expandable gases in vitrectomy. J Ophthalmol. 2018;2018:8606494.
Gupta V, Prabhakar A, Yadav M, Khandelwal N. Computed tomography imaging-based normative orbital measurement in Indian population. Indian J Ophthalmol. 2019;67:659–63.
Fernandes A, Bradley DV, Tigges M, Tigges J, Herndon JG. Ocular measurements throughout the adult life span of rhesus monkeys. Invest Ophthalmol Vis Sci. 2003;44:2373–80.
Bach A, Villegas VM, Gold AS, Shi W, Murray TG. Axial length development in children. Int J Ophthalmol. 2019;12:815–9.
Uchino E, Uemura A, Ohba N. Initial stages of posterior vitreous detachment in healthy eyes of older persons evaluated by optical coherence tomography. Arch Ophthalmol. 2001;119:1475–9.
Inoue M. Wide-angle viewing system. Dev Ophthalmol. 2014;54:87–91.
Virata SR, Kylstra JA, Singh HT. Corneal epithelial defects following vitrectomy surgery using hand-held, sew-on, and noncontact viewing lenses. Retina. 1999;19:287–90.
Sheng Lim K, Garg A, Cheng J, Muthusamy K, Beltran-Agullo L, Barton K. Comparison of short-term postoperative hypotony rates of 23-gauge vs 25-gauge needles in formation of the scleral tract for Baerveldt tube insertion into the anterior chamber. J Curr Glaucoma Pr. 2018;12:36–9.
Ho LY, Garretson BR, Ranchod TM, Balasubramaniam M, Ruby AJ, Capone A Jr, et al. Study of intraocular pressure after 23-gauge and 25-gauge pars plana vitrectomy randomized to fluid versus air fill. Retina. 2011;31:1109–17.
Inoue Y, Kadonosono K, Yamakawa T, Uchio E, Watanabe Y, Yanagi Y, et al. Surgically-induced inflammation with 20-, 23-, and 25-gauge vitrectomy systems: an experimental study. Retina. 2009;29:477–80.
Sedova A, Steiner I, Matzenberger RP, Georgopoulos M, Scholda C, Kriechbaum KF, et al. Comparison of safety and effectiveness between 23-gauge and 25-gauge vitrectomy surgery in common vitreoretinal diseases. PLoS One. 2021;16:e0248164.
Sawada T, Kakinoki M, Sawada O, Kawamura H, Ohji M. Closure of sclerotomies after 25- and 23-gauge transconjunctival sutureless pars plana vitrectomy evaluated by optical coherence tomography. Ophthalmic Res. 2011;45:122–8.
Barth H, Crafoord S, Arner K, Ghosh F. Inflammatory responses after vitrectomy with vitreous substitutes in a rabbit model. Graefes Arch Clin Exp Ophthalmol. 2019;257:769–83.
Chen W, Mo W, Sun K, Huang X, Zhang YL, Song HY. Microplasmin degrades fibronectin and laminin at vitreoretinal interface and outer retina during enzymatic vitrectomy. Curr Eye Res. 2009;34:1057–64.
Grinton M, Steel DH. Cochrane Corner: Ocriplasmin-why isn’t it being used more? Eye (Lond). 2019;33:1195–7.
Gandorfer A, Rohleder M, Sethi C, Eckle D, Welge-Lüssen U, Kampik A, et al. Posterior vitreous detachment induced by microplasmin. Invest Ophthalmol Vis Sci. 2004;45:641–7.
Wassmer SJ, Carvalho LS, György B, Vandenberghe LH, Maguire CA. Exosome-associated AAV2 vector mediates robust gene delivery into the murine retina upon intravitreal injection. Sci Rep. 2017;7:45329.
Acknowledgements
The sponsor or funding organisation had no role in the design or conduct of this research. We thank MJEditor (www.mjeditor.com) for language editing.
Funding
National Key R&D Program of China [2021YFA1101200]. National Key R&D Program of China [2016YFC1101200]. National Natural Science Foundation of China [81770926;81800842]. Key R&D Program of Zhejiang Province [2019C03009; 2021C03065]. Key R&D Program of Wenzhou Eye Hospital [YNZD1201902]. National Key R&D Program of China [2019YFC0119300].
Author information
Authors and Affiliations
Contributions
Conceptualisation: YZ, QP; Data curation: YZ, SL, ML; Formal Analysis: SL, ML, HP, LW, YM; Funding acquisition: YZ, WW; Methodology: YZ, QP; Visualisation: YZ, QP, SL, ML. Writing – original draft: YZ, QP, SL, ML; Writing – review & editing: YZ, QP, WW.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The research followed the principles of the Declaration of Helsinki, and was approved by the ethics committees of Wenzhou Eye Hospital, Wenzhou Medical University (Ethics ID number: KYK (2017) 53). Patient consents from three male adults were obtained before analysis of their orbital CT scan data in this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pan, Q., Lu, S., Li, M. et al. Vitrectomy and ILM peeling in rhesus macaque: pitfalls and tips for success. Eye 37, 2257–2264 (2023). https://doi.org/10.1038/s41433-022-02327-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02327-5