Abstract
Aim This study aimed to compare the long-term outcome of implant therapy in partially edentulous patients with severe periodontitis compared to those with no history of periodontitis.
Design Retrospective cohort study.
Cohort selection Eighty-eight patients (34 men and 54 women; age ranging from 28 to 45 years) with severe periodontitis (47 patients with 108 implants) and no history of periodontitis (41 patients with 78 implants) were included in this institutional study. All these cohorts had received implants 6-8 years previously.
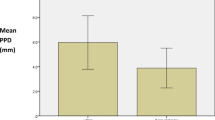
Data analysis Probing pocket depth, radiographic marginal bone level and peri-implantitis were the primary outcomes, while bleeding on probing was the secondary outcome. The effect of variables was measured by odds ratio with 95% confidence interval. Both patient-level and implant-level analyses were used to evaluate the association between peri-implantitis and potential risk factors. In addition, the association between probing pocket depth and radiographic marginal bone level with potential risk factors was assessed at implant-level analyses. In contrast, for patient-level data, a positive relationship was assessed with the Chi-square test.
Results Patients with a history of severe periodontitis (OR = 11.13; p = 0.045), implants with a lack (<2 mm) of peri-implant keratinised mucosa (OR = 14.94; p <0.001) and implants placed in bone-grafted sites (OR = 4.93; p = 0.047) were associated with greater risk of peri-implantitis, at 6-8 years post-implant placement. The risk of developing radiographic marginal bone level ≥3 mm was significantly greater (OR = 1.20; p <0.001) in patients with higher full-mouth bleeding scores. The chance of peri-implant bleeding on probing was independently and especially higher in patients who brushed their teeth at most once per day (OR = 3.20; p = 0.04), with higher full-mouth bleeding score values (OR = 1.16; p <0.001) and irregular recall visits (OR = 15.34; p = 0.001).
Conclusion This retrospective cohort study concluded that partially edentulous patients with a history of severe periodontitis were more prone to develop peri-implantitis at 6-8 years post-implant placement.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Papapanou P N, Sanz M, Buduneli N et al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol 2018; 45 Suppl 20: S162-S170.
Avila G, Galindo-Moreno P, Soehren S, Misch C E, Morelli T, Wang H L. A novel decision-making process for tooth retention or extraction. J Periodontol 2009; 80: 476-491.
Ferreira S D, Martins C C, Amaral S A et al. Periodontitis as a risk factor for peri-implantitis: Systematic review and meta-analysis of observational studies. J Dent 2018; 79: 1-10.
Carra M C, Rangé H, Swerts P J, Tuand K, Vandamme K, Bouchard P. Effectiveness of implant-supported fixed partial denture in patients with history of periodontitis: A systematic review and meta-analysis. J Clin Periodontol 2021; DOI: 10.1111/jcpe.13481.
Alhakeem M, Kanounisabet N, Nowzari H, Aslroosta H, Moslemi N. Risk indicators of long-term outcome of implant therapy in patients with a history of severe periodontitis or no history of periodontitis: A retrospective cohort study. Int J Dent Hyg 2022; DOI: 10.1111/idh.12587.
Critical Appraisal Skills Programme. CASP (Cohort Study) Checklist. 2018. Available at https://casp-uk.net/casp-tools-checklists/ (accessed April 2022).
Wells G, Shea B, O'Connell D et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available at http://www.ohri.ca/programmes/clinical_epidemiology/oxford.asp (accessed April 2022).
Schwarz F, Derks J, Monje A, Wang H L. Peri-implantitis. J Periodontol 2018; 89 Suppl 1: S267-S290.
Hashim D, Cionca N A. Comprehensive Review of Peri-implantitis Risk Factors. Curr Oral Health Rep 2020; 7: 262-273.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Dhingra, K., Jeng, JH. Are partially edentulous patients with a history of severe periodontitis more prone to develop peri-implantitis over the long term?. Evid Based Dent 23, 81–83 (2022). https://doi.org/10.1038/s41432-022-0269-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41432-022-0269-4
This article is cited by
-
Characteristics of mandibular anterior alveolar bone in patients with different degrees of periodontitis: a retrospective study based on CBCT
Clinical Oral Investigations (2023)