Abstract
Oral rehabilitation of head and neck cancer patients is an integral component of the care pathway. Maxillectomy procedures can cause significant defects, such as oronasal fistulas, loss of support for the cheek and lip, aesthetic defects in the middle third of the face and functional impairments. Orofacial rehabilitation plays a fundamental role in restoring aesthetics and functional capabilities, such as speech, mastication and deglutition.
Rehabilitation of maxillectomy patients poses a challenge for both clinicians and patients. This paper utilises case examples to demonstrate the treatment options for the oral rehabilitation of these patients. We will summarise the treatment pathways for conventional obturators, delayed (secondary) implant retained fixed rehabilitation following composite free flap and early rehabilitation using a zygomatic implant perforated flap technique. This paper aims to highlight the challenges in treatment planning and the importance of a multidisciplinary approach in improving patient outcomes.
Key points
-
Maxillectomy defects can have a significant impact on both psychological and functional capabilities.
-
Several rehabilitation options exist for these patients, with various considerations as to the most appropriate option.
-
This paper provides a summary of the rehabilitation options and the pathways for managing these patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Wells M, Cunningham M, Lang H et al. Distress, concerns and unmet needs in survivors of head and neck cancer: a cross-sectional survey. Eur J Cancer Care (Engl) 2015; 24: 748-760.
Tirelli G, Rizzo R, Biasotto M et al. Obturator prostheses following palatal resection: clinical cases. Acta Otorhinolaryngol Ital 2010; 30: 33-39.
dos Santos D M, de Caxias F P, Bitencourt S B, Turcio K H, Pesqueira A A, Goiato M C. Oral rehabilitation of patients after maxillectomy. A systematic review. Br J Oral Maxillofac Surg 2018; 56: 256-266.
The Royal College of Surgeons of England. The Oral Management of Oncology Patients Requiring Radiotherapy, Chemotherapy and/or Bone Marrow Transplantation: Clinical Guidelines. 2018. Available at https://www.rcseng.ac.uk/-/media/files/rcs/fds/publications/rcs-oncology-guideline-update--v36.pdf (accessed May 2022).
Dexter W S, Jacob R F. Prosthetic rehabilitation after maxillectomy and temporalis flap reconstruction: a clinical report. J Prosthet Dent 2000; 83: 283-286.
Barclay C W, Foster E C, Taylor C L. Restorative aspects of oral cancer reconstruction. Br Dent J 2018; 225: 848-854.
Brierley J, Gospodarowicz M, Wittekind C. TNM Classification of Malignant Tumours. 8th ed. New Jersey: Wiley-Blackwell, 2020.
Won H S, Chun S H, Kim B-S et al. Treatment outcome of maxillary sinus cancer. Rare Tumors 2009; DOI: 10.4081/rt.2009.e36.
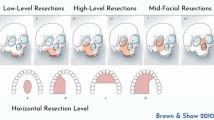
Brown J S, Shaw R J. Reconstruction of the maxilla and midface: Introducing a new classification. Lancet Oncol 2010; 11: 1001-1008.
Butterworth C, McCaul L, Barclay C. Restorative dentistry and oral rehabilitation: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol 2016; DOI: 10.1017/S0022215116000414.
Wang W H, Zou Z R, Xu B, Wang W Q, Shen S Y. Maxillary Reconstruction Using Submental Artery Island Flap and Sagittal Mandibular Ramus/Coronoid Process Graft Pedicled With Temporalis Muscle. J Oral Maxillofac Surg 2017; DOI: 10.1016/j.joms.2017.06.035.
Moreno M A, Skoracki R J, Hanna E Y, Hanasono M M. Microvascular free flap reconstruction versus palatal obturation for maxillectomy defects. Head Neck 2010; 32: 860-868.
Butterworth C J, Rogers S N. The zygomatic implant perforated (ZIP) flap: a new technique for combined surgical reconstruction and rapid fixed dental rehabilitation following low-level maxillectomy. Int J Implant Dent 2017; DOI: 10.1186/s40729-017-0100-8.
Rogers S N, Lowe D, Fisher S E, Brown J S, Vaughan E D. Health-related quality of life and clinical function after primary surgery for oral cancer. Br J Oral Maxillofac Surg 2002; 40: 11-18.
Ali R, Altaie A, Nattress B. Rehabilitation of oncology patients with hard palate defects. Part 1: The surgical planning phase. Dent Update 2015; 42: 326-328.
Breeze J, Rennie A, Morrison A et al. Health-related quality of life after maxillectomy: obturator rehabilitation compared with flap reconstruction. Br J Oral Maxillofac Surg 2016; 54: 857-862.
Dalkiz M, Dalkiz A S. The Effect of Immediate Obturator Reconstruction after Radical Maxillary Resections on Speech and other Functions. Dent J (Basel) 2018; DOI: 10.3390/dj6030022.
Ali R, Altaie A, Nattress B. Rehabilitation of oncology patients with hard palate defects Part 2: Principles of obturator design. Dent Update 2015; 42: 428-434.
Shah D, Meenakshi A. The obturator prostheses for maxillectomy. SRM J Res Dent Sci 2012; 3: 193-197.
Kumar N. Updated clinical guidelines on the oral management of oncology patients. Facult Dent J 2019; 10: 62-65.
Butterworth C J. Primary vs secondary zygomatic implant placement in patients with head and neck cancer - A 10-year prospective study. Head Neck 2019; 41: 1687-1695.
Bidra A S. Surgical and prosthodontic consequences of inadequate treatment planning for fixed implant-supported prosthesis in the edentulous mandible. J Oral Maxillofac Surg 2010; 68: 2528-2536.
Laverty D P, Kelly R, Addison O. Survival of dental implants placed in autogenous bone grafts and bone flaps in head and neck oncology patients: a systematic review. Int J Implant Dent 2018; DOI: 10.1186/s40729-018-0131-9.
Rohner D, Bucher P, Hammer B. Prefabricated fibular flaps for reconstruction of defects of the maxillofacial skeleton: planning, technique, and long-term experience. Int J Oral Maxillofac Implants 2013; DOI: 10.11607/jomi.te01.
Meloni S; Tallarico M; Canullo L; De Riu G; Massarelli O. Periimplant soft-tissue management in patients with fibula free flap reconstruction: Case series and description of a new technique. J Oral Sci Rehabil 2016; 2: 26-30.
Patel J, Antov H, Nixon P. Implant-supported oral rehabilitation in oncology patients: a retrospective cohort study. Br J Oral Maxillofac Surg 2020; 58: 1003-1007.
Burgess M, Leung M, Chellapah A, Clark J R, Batstone M D. Osseointegrated implants into a variety of composite free flaps: A comparative analysis. Head Neck 2017; 39: 443-447.
Chow J. Zygomatic Implants: Optimization and Innovation. Switzerland: Springer, 2020.
Chrcanovic B R, Albrektsson T, Wennerberg A. Survival and Complications of Zygomatic Implants: An Updated Systematic Review. J Oral Maxillofac Surg 2016; 74: 1949-1964.
Hackett S, El-Wazani B, Butterworth C. Zygomatic implant-based rehabilitation for patients with maxillary and mid-facial oncology defects: A review. Oral Dis 2021; 27: 27-41.
Lan K, Wang F, Huang W, Davó R, Wu Y. Quad Zygomatic Implants: A Systematic Review and Meta-analysis on Survival and Complications. Int J Oral Maxillofac Implants 2021; 36: 21-29.
Kanatas A, Ho M W. Monitoring of free flaps and reconstruction for oral cancer. Br J Oral Maxillofac Surg 2018; DOI: 10.1016/j.bjoms.2018.01.008.
Salvatori P, Mincione A, Rizzi L et al. Maxillary resection for cancer, zygomatic implants insertion, and palatal repair as single-stage procedure: report of three cases. Maxillofac Plast Reconstr Surg 2017; DOI: 10.1186/s40902-017-0112-6.
Author information
Authors and Affiliations
Contributions
Olivia Barraclough, Jaymit Patel, Stephanie Milne, Michael W. Ho and Zaid Ali have all equally contributed to writing and editing this manuscript.
Corresponding author
Ethics declarations
None of the authors have any conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Barraclough, O., Patel, J., Milne, S. et al. Pathways for the rehabilitation of resection defects in the maxilla. Br Dent J 232, 783–789 (2022). https://doi.org/10.1038/s41415-022-4342-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-022-4342-3