Abstract
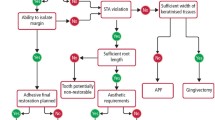
This paper aims to update the reader on how minimally invasive (MI) techniques may be used to improve the longevity of carious or defective/compromised first permanent molars (cFPMs) in young children. Clinical and radiographic diagnosis and the prognostic factors will be discussed in view of recent studies showing that these teeth can be kept in function and have an improved prognosis as the child gets older. Clinical protocols for their care, based on the latest evidence and techniques for MI restorations, together with longevity information of possible restorative options, are described. This paper also explores the rationale behind enforced extractions and related morbidity, in order to help oral healthcare practitioners to determine the optimal management of these key elements in the dentition for the benefit of the patients.
Key points
-
Dental practitioners treating young children frequently face cavitated carious or hypomineralised first permanent molars in their clinical practice.
-
The use of improved minimally invasive techniques and materials, such as high-viscosity glass ionomers, may improve the prognosis of compromised first permanent molars in young children and reduce the need for extractions under general anaesthesia.
-
Compromised first permanent molars may be able to survive longer in the oral cavity of young children, postponing definitive restorative treatment for later in life.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Taylor G D, Pearce K F, Vernazza C R. Management of compromised first permanent molars in children: Cross-sectional analysis of attitudes of UK general dental practitioners and specialists in paediatric dentistry. Int J Paediatr Dent 2019; 29: 267-280.
Cobourne M T, Williams A, Harrison M. National clinical guidelines for the extraction of first permanent molars in children. Br Dent J 2014; 217: 643-648.
Ashley P, Noar J. Interceptive extractions for first permanent molars: A clinical protocol. Br Dent J 2019; 227: 192-195.
Sayagh M, Maniere-Ezvan A, Vernet C, Muller-Bolla M. Therapeutic decisions in the presence of decayed permanent first molars in young subjects: A descriptive inquiry. Int Orthod 2012; 10: 318-336.
Thylstrup A, Bruun C, Holmen L. In vivo caries models: Mechanisms for caries initiation and arrestment. Adv Dent Res 1994; 8: 144-157.
Agel M, Banerjee A, Neves A A, Costa L S, Hosey M T. First permanent molar extractions under general anaesthesia: A CEDACORE survey. J Dent Res 2018; 97(Special Issue B): 2678.
Carvalho J C, Ekstrand K R, Thylstrup A. Dental plaque and caries on occlusal surfaces of first permanent molars in relation to stage of eruption. J Dent Res 1989; 68: 773-779.
Carvalho J C, Figueredo C S, Mestrinho H D. Clinical report on plaque formation, distribution and maturation within the primary, mixed and permanent dentitions. Eur J Paediatr Dent 2009; 10: 193-199.
Zhao D, Dong B, Yu D, Ren Q, Sun Y. The prevalence of molar incisor hypomineralization: Evidence from 70 studies. Int J Paediatr Dent 2018; 28: 170-179.
Jalevik B, Dietz W, Noren J G. Scanning electron micrograph analysis of hypomineralized enamel in permanent first molars. Int J Paediatr Dent 2005; 15: 233-240.
Xie Z H, Mahoney E K, Kilpatrick N M, Swain M V, Hoffman M. On the structure-property relationship of sound and hypomineralized enamel. Acta Biomater 2007; 3: 865-872.
Fatturi A L, Wambier L M, Chibinski A C et al. A systematic review and meta-analysis of systemic exposure associated with molar incisor hypomineralization. Community Dent Oral Epidemiol 2019; 47: 407-415.
Jeremias F, Pierri R A, Souza J F et al. Family-based genetic association for molar-incisor hypomineralization. Caries Res 2016; 50: 310-318.
Bussaneli D G, Restrepo M, Fragelli C M B et al. Genes regulating immune response and amelogenesis interact in increasing the susceptibility to molar-incisor hypomineralization. Caries Res 2019; 53: 217-227.
Farah R A, Swain M V, Drummond B K, Cook R, Atieh M. Mineral density of hypomineralised enamel. J Dent 2010; 38: 50-58.
Neves A B, Americano G C A, Soares D V, Soviero V M. Breakdown of demarcated opacities related to molar-incisor hypomineralization: A longitudinal study. Clin Oral Investig 2019; 23: 611-615.
SDCEP. Prevention and management of dental caries in children: Dental clinical guidance (second edition). 2018. Available at https://www.sdcep.org.uk/wp-content/uploads/2018/05/SDCEP-Prevention-and-Management-of-Dental-Caries-in-Children-2nd-Edition.pdf (accessed September 2020).
Ismail A I, Sohn W, Tellez M et al. The International Caries Detection and Assessment System (ICDAS): An integrated system for measuring dental caries. Community Dent Oral Epidemiol 2007; 35: 170-178.
Chawla N, Messer L B, Silva M. Clinical studies on molarincisorhypomineralisation part 2: Development of a severity index. Eur Arch Paediatr Dent 2008; 9: 191-199.
Ha N, Kim Y, Kim H, Nam S. A prognostic assessment of first permanent molars showing molar-incisor hypomineralization based on restorative materials and defect class. J Korean Acad Pediatr Dent 2017; 44: 263-271.
Leal S C. Minimal intervention dentistry in the management of the paediatric patient. Br Dent J 2014; 216: 623-627.
Oliveira D C, Favretto C O, Cunha R F. Molar incisor hypomineralization: Considerations about treatment in a controlled longitudinal case. J Indian Soc Pedod Prev Dent 2015; 33: 152-155.
Kramer N, Bui Khac N N, Lucker S, Stachniss V, Frankenberger R. Bonding strategies for MIH-affected enamel and dentin. Dent Mater 2018; 34: 331-340.
Lygidakis N A. Treatment modalities in children with teeth affected by molar-incisor enamel hypomineralisation (MIH): A systematic review. Eur Arch Paediatr Dent 2010; 11: 65-74.
Souza J F, Fragelli C B, Jeremias F, Paschoal M A B, Santos-Pinto L, Loiola-Cordeiro R C. Eighteen-month clinical performance of composite resin restorations with two different adhesive systems for molars affected by molar incisor hypomineralization. Clin Oral Investig 2017; 21: 1725-1733.
Dhareula A, Goyal A, Gauba K, Bhatia S K, Kapur A, Bhandari S. A clinical and radiographic investigation comparing the efficacy of cast metal and indirect resin onlays in rehabilitation of permanent first molars affected with severe molar incisor hypomineralisation (MIH): A 36-month randomised controlled clinical trial. Eur Arch Paediatr Dent 2019; 20: 489-500.
Fragelli C M, Souza J F, Jeremias F, de Cássia Loiola Cordeiro R, Santos-Pinto L. Molar Incisor Hypomineralization (MIH): Conservative treatment management to restore affected teeth. Braz Oral Res 2015; DOI: 10.1590/1807-3107BOR-2015.vol29.0076.
Cvar J F, Ryge G. Reprint of criteria for the clinical evaluation of dental restorative materials. 1971. Clin Oral Investig 2005; 9: 215-232.
Hickel R, Peschke A, Tyas M et al. FDI World Dental Federation - Clinical criteria for the evaluation of direct and indirect restorations. Update and clinical examples. J Adhes Dent 2010; 12: 259-272.
Green D, Mackenzie L, Banerjee A. Minimally invasive long-term management of direct restorations: The 5 R's. Dent Update 2015; DOI: 10.12968/denu.2015.42.5.413.
Lucarotti P S, Burke F J. The ultimate guide to restoration longevity in england and wales. Part 6. Molar teeth: Restoration time to next intervention and to extraction of the restored tooth. Br Dent J 2018; 225: 525-536.
Davies G M, Davies R M. Delivering Better Oral Health - An evidence-based toolkit for prevention: A review. Dent Update 2008; DOI: 10.12968/denu.2008.35.7.460.
Crombie F A, Cochrane N J, Manton D J, Palamara J E, Reynolds E C. Mineralisation of developmentally hypomineralised human enamel in vitro. Caries Res 2013; 47: 259-263.
Ozgul B M, Saat S, Sonmez H, Oz F T. Clinical evaluation of desensitizing treatment for incisor teeth affected by molar-incisor hypomineralization. J Clin Pediatr Dent 2013; 38: 101-105.
Pasini M, Giuca M R, Scatena M, Gatto R, Caruso S. Molar incisor hypomineralization treatment with casein phosphopeptide and amorphous calcium phosphate in children. Minerva Stomatol 2018; 67: 20-25.
Frencken J E. The state-of-the-art of ART sealants. Dent Update 2014; DOI: 10.12968/denu.2014.41.2.119.
Schwendicke F, Splieth C, Breschi L et al. When to intervene in the caries process? An expert DELPHI consensus statement. Clin Oral Investig 2019; 23: 3691-3703.
Schwendicke F. Removing carious tissue: Why and how? Mon Oral Science 2018; 27: 56-67.
Najeeb S, Khurshid Z, Zafar M S et al. Modifications in glass ionomer cements: Nano-sized fillers and bioactive nanoceramics. Int J Mol Sci 2016; 17: 1134.
Diem V T, Tyas M J, Ngo H C, Phuong L H, Khanh N D. The effect of a nano-filled resin coating on the 3year clinical performance of a conventional high-viscosity glass-ionomer cement. Clin Oral Investig 2014; 18: 753-759.
Grossi J A, Cabral R N, Ribeiro A P D, Leal S C. Glass hybrid restorations as an alternative for restoring hypomineralized molars in the art model. BMC Oral Health 2018; 18: 65.
Van Meerbeek B, De Munck J, Yoshida Y et al. Buonocore memorial lecture - adhesion to enamel and dentin: Current status and future challenges. Oper Dent 2003; 28: 215-235.
Isolan C P, Sarkis-Onofre R, Lima G S, Moraes R R. Bonding to sound and caries-affected dentin: A systematic review and meta-analysis. J Adhes Dent 2018; 20: 7-18.
Van Meerbeek B, Peumans M, Poitevin A et al. Relationship between bond-strength tests and clinical outcomes. Dent Mater 2009; DOI: 10.1016/j.dental.2009.11.148.
William V, Burrow M F, Palamara J E, Messer L B. Microshear bond strength of resin composite to teeth affected by molar hypomineralization using 2 adhesive systems. Pediatr Dent 2006; 28: 233-241.
Sönmez H, Saat S. A clinical evaluation of deproteinization and different cavity designs on resin restoration performance in MIH-affected molars: Two-year results. J Clin Pediatr Dent 2017; 41: 336-342.
Rosenblatt A, Stamford T C, Niederman R. Silver diamine fluoride: A caries "silver-fluoride bullet". J Dent Res 2009; 88: 116-125.
Gao S S, Zhao I S, Hiraishi N C et al. Clinical trials of silver diamine fluoride in arresting caries among children: A systematic review. JDR Clin Trans Res 2016; 1: 201-210.
Zhao I S, Gao S S, Hiraishi N et al. Mechanisms of silver diamine fluoride on arresting caries: A literature review. Int Dent J 2018; 68: 67-76.
Chu C H, Lo E C. Promoting caries arrest in children with silver diamine fluoride: A review. Oral Health Prev Dent 2008; 6: 315-321.
Yee R, Holmgren C, Mulder J, Lama D, Walker D, van Palenstein Helderman W. Efficacy of silver diamine fluoride for arresting caries treatment. J Dent Res 2009; 88: 644-647.
Alvear Fa B, Jew J A, Wong A, Young D. Silver modified atraumatic restorative technique (SMART): An alternative caries prevention tool. Stomatol Edu J 2016; 3: 18-23.
Puwanawiroj A, Trairatvorakul C, Dasanayake A P, Auychai P. Microtensile bond strength between glass ionomer cement and silver diamine fluoride-treated carious primary dentin. Pediatr Dent 2018; 40: 291-295.
Jalevik B, Klingberg G A. Dental treatment, dental fear and behaviour management problems in children with severe enamel hypomineralization of their permanent first molars. Int J Paediatr Dent 2002; 12: 24-32.
Elhennawy K, Krois J, Jost-Brinkmann P G, Schwendicke F. Outcome and comparator choice in molar incisor hypomineralisation (MIH) intervention studies: A systematic review and social network analysis. BMJ Open 2019; DOI: 10.1136/bmjopen-2018-028352.
Jalevik B, Moller M. Evaluation of spontaneous space closure and development of permanent dentition after extraction of hypomineralized permanent first molars. Int J Paediatr Dent 2007; 17: 328-335.
Wu M, Chen L, Bawole E, Anthonappa R P, King N M. Is there sufficient evidence to support an optimum time for the extraction of first permanent molars? Eur Arch Pediatr Dent 2017; 18: 155-161.
Teo T K, Ashley P F, Derrick D. Lower first permanent molars: Developing better predictors of spontaneous space closure. Eur J Orthod 2016; 38: 90-95.
Mittal N. Phenotypes of enamel hypomineralization and molar incisor hypomineralization in permanent dentition: Identification, quantification and proposal for classification. J Clin Pediatr Dent 2016; 40: 367-374.
Hosey M T, Macpherson L M, Adair P, Tochel C, Burnside G, Pine C. Dental anxiety, distress at induction and postoperative morbidity in children undergoing tooth extraction using general anaesthesia. Br Dent J 2006; DOI: 10.1038/sj.bdj.4813123.
Alohali A A, Al-Rubaian N, Tatsi C, Sood S, Hosey M T. Post-operative pain and morbidity in children who have tooth extractions under general anaesthesia: A service evaluation. Br Dent J 2019; 227: 713-718.
Rodd H, Hall M, Deery C, Gilchrist F, Gibson B J, Marshman Z. 'I felt weird and wobbly.' Child-reported impacts associated with a dental general anaesthetic. Br Dent J 2014; DOI: 10.1038/sj.bdj.2014.333.
Huntington C, Liossi C, Donaldson A N et al. On-line preparatory information for children and their families undergoing dental extractions under general anaesthesia: A phase III randomized controlled trial. Paediatr Anaesth 2018; 28: 157-166.
Acknowledgements
This paper is part of a clinical research collaboration with Brazil entitled: Children Experiencing Dental Anxiety Collaboration on Research and Education (CEDACORE) which was funded by CAPES (Brazil) and Newton Fund British Council (UK). The Ministry of Education, Saudi Arabia is also acknowledged for sponsoring the PhD studentship of Reem Alkhalaf. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alkhalaf, R., Neves, A., Banerjee, A. et al. Minimally invasive judgement calls: managing compromised first permanent molars in children. Br Dent J 229, 459–465 (2020). https://doi.org/10.1038/s41415-020-2154-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-020-2154-x
This article is cited by
-
Clinical and radiographic performance of preformed zirconia crowns and stainless-steel crowns in permanent first molars: 18-month results of a prospective, randomized trial
BMC Oral Health (2023)
-
Molar-incisor hypomineralisation combat: exploratory qualitative interviews with general dental practitioners in England regarding the management of children with molar-incisor hypomineralisation
British Dental Journal (2022)
-
An update of treatment modalities in children and adolescents with teeth affected by molar incisor hypomineralisation (MIH): a systematic review
European Archives of Paediatric Dentistry (2022)
-
Children’s dental treatment requirements of first permanent molars with poor prognosis
Clinical Oral Investigations (2022)
-
Worldwide trends on molar incisor and deciduous molar hypomineralisation research: a bibliometric analysis over a 19-year period
European Archives of Paediatric Dentistry (2022)