Abstract
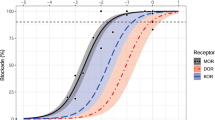
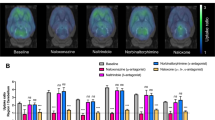
Morphine and morphine-6-glucuronide (M6G) produce central nervous system (CNS) effects by activating mu-opioid receptors, while naloxone is used mainly for the reversal of opioid overdose, specifically for the fatal complication of respiratory depression, but also for alleviating opioid-induced side effects. In this study we developed a physiologically-based pharmacokinetic-pharmacodynamic (PBPK-PD) model to simultaneously predict pharmacokinetics and CNS effects (miosis, respiratory depression and analgesia) of morphine as well as antagonistic effects of naloxone against morphine. The pharmacokinetic and pharmacodynamic parameters were obtained from in vitro data, in silico, or animals. Pharmacokinetic and pharmacodynamic simulations were conducted using 39 and 36 clinical reports, respectively. The pharmacokinetics of morphine and M6G following oral or intravenous administration were simulated, and the PBPK-PD model was validated using clinical observations. The Emax model correlated CNS effects with free concentrations of morphine and M6G in brain parenchyma. The predicted CNS effects were compared with observations. Most clinical observations fell within the 5th–95th percentiles of simulations based on 1000 virtual individuals. Most of the simulated area under the concentration-time curve or peak concentrations also fell within 0.5–2-fold of observations. The contribution of morphine to CNS effects following intravenous or oral administration was larger than that of M6G. Pharmacokinetics and antagonistic effects of naloxone on CNS effects were also successfully predicted using the developed PBPK-PD model. In conclusion, the pharmacokinetics and pharmacodynamics of morphine and M6G, antagonistic effects of naloxone against morphine-induced CNS effects may be successfully predicted using the developed PBPK-PD model based on the parameters derived from in vitro, in silico, or animal studies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout









Similar content being viewed by others
References
Faura CC, Collins SL, Moore AR, McQuay HJ. Systematic review of factors affecting the ratios of morphine and its major metabolites. Pain. 1998;74:43–53.
Packiasabapathy S, Zhang X, Ding L, Aruldhas BW, Pawale D, Sadhasivam S. Quantitative pupillometry as a predictor of pediatric postoperative opioid-induced respiratory depression. Anesth Analg. 2021;133:991–9.
Macleod DB, Habib AS, Ikeda K, Spyker DA, Cassella JV, Ho KY, et al. Inhaled fentanyl aerosol in healthy volunteers: Pharmacokinetics and pharmacodynamics. Anesth Analg. 2012;115:1071–7.
Lötsch J, Geisslinger G. Are mu-opioid receptor polymorphisms important for clinical opioid therapy? Trends Mol Med. 2005;11:82–9.
German C, Pilvankar M, Przekwas A. Computational framework for predictive PBPK-pd-tox simulations of opioids and antidotes. J Pharmacokinet Pharmacodyn. 2019;46:513–29.
Verscheijden LFM, Litjens CHC, Koenderink JB, Mathijssen RHJ, Verbeek MM, de Wildt SN, et al. Physiologically based pharmacokinetic/pharmacodynamic model for the prediction of morphine brain disposition and analgesia in adults and children. PLoS Comput Biol. 2021;17:e1008786.
He F, Jiang Y, Li L. The effect of naloxone treatment on opioid-induced side effects: A meta-analysis of randomized and controlled trails. Med (Baltim). 2016;95:e4729.
Busse D, Leandersson S, Amberntsson S, Darnell M, Hilgendorf C. Industrial approach to determine the relative contribution of seven major ugt isoforms to hepatic glucuronidation. J Pharm Sci. 2020;109:2309–20.
Wahlström A, Persson K, Rane A. Metabolic interaction between morphine and naloxone in human liver. A common pathway of glucuronidation? Drug Metab Dispos. 1989;17:218–20.
Meissner K, Dahan A, Olofsen E, Göpfert C, Blood J, Wieditz J, et al. Morphine and hydromorphone effects, side effects, and variability: A crossover study in human volunteers. Anesthesiology. 2023;139:16–34.
Tylleskar I, Skulberg AK, Skarra S, Nilsen T, Dale O. Pharmacodynamics and arteriovenous difference of intravenous naloxone in healthy volunteers exposed to remifentanil. Eur J Clin Pharmacol. 2018;74:1547–53.
D’Honneur G, Gilton A, Sandouk P, Scherrmann JM, Duvaldestin P. Plasma and cerebrospinal fluid concentrations of morphine and morphine glucuronides after oral morphine. The influence of renal failure. Anesthesiology. 1994;81:87–93.
Lagas JS, Wagenaar JFP, Huitema ADR, Hillebrand MJX, Koks CHW, Gerdes VEA, et al. Lethal morphine intoxication in a patient with a sickle cell crisis and renal impairment: Case report and a review of the literature. Hum Exp Toxicol. 2010;30:1399–403.
Upadhyay S, Jain R, Chauhan H, Gupta D, Mishra S, Bhatnagar S. Oral morphine overdose in a cancer patient antagonized by prolonged naloxone infusion. Am J Hosp Palliat Care. 2008;25:401–5.
Coffman BL, Rios GR, King CD, Tephly TR. Human UGT2B7 catalyzes morphine glucuronidation. Drug Metab Disposition. 1997;25:1–4.
Emoto C, Fukuda T, Johnson TN, Neuhoff S, Sadhasivam S, Vinks AA. Characterization of contributing factors to variability in morphine clearance through PBPK modeling implemented with OCT1 transporter. CPT Pharmacomet Syst Pharmacol. 2017;6:110–9.
Bickel U, Schumacher OP, Kang YS, Voigt K. Poor permeability of morphine 3-glucuronide and morphine 6-glucuronide through the blood-brain barrier in the rat. J Pharmacol Exp Ther. 1996;278:107–13.
Letrent SP, Polli JW, Humphreys JE, Pollack GM, Brouwer KR, Brouwer KL. P-glycoprotein-mediated transport of morphine in brain capillary endothelial cells. Biochem Pharmacol. 1999;58:951–7.
Bouw MR, Gårdmark M, Hammarlund-Udenaes M. Pharmacokinetic-pharmacodynamic modelling of morphine transport across the blood-brain barrier as a cause of the antinociceptive effect delay in rats—a microdialysis study. Pharmacol Res. 2000;17:1220–7.
Tunblad K, Hammarlund-Udenaes M, Jonsson EN. Influence of probenecid on the delivery of morphine-6-glucuronide to the brain. Eur J Pharm Sci. 2005;24:49–57.
Mashayekhi SO, Sattari MR, Routledge PA. Evidence of active transport involvement in morphine transport via MDCKII and MDCK-PGP cell lines. Res Pharm Sci. 2010;5:99–106.
Crowe A. The influence of P-glycoprotein on morphine transport in Caco-2 cells. Comparison with paclitaxel. Eur J Pharmacol. 2002;440:7–16.
Dale O, Nilsen T, Olaussen G, Tvedt KE, Skorpen F, Smidsrød O, et al. Transepithelial transport of morphine and mannitol in Caco-2 cells: The influence of chitosans of different molecular weights and degrees of acetylation. J Pharm Pharmacol. 2006;58:909–15.
Nagaya Y, Nozaki Y, Kobayashi K, Takenaka O, Nakatani Y, Kusano K, et al. Utility of cerebrospinal fluid drug concentration as a surrogate for unbound brain concentration in nonhuman primates. Drug Metab Pharmacokinet. 2014;29:419–26.
Lin JH. CSF as a surrogate for assessing CNS exposure: An industrial perspective. Curr Drug Metab. 2008;9:46–59.
Caruso A, Alvarez-Sánchez R, Hillebrecht A, Poirier A, Schuler F, Lavé T, et al. PK/PD assessment in CNS drug discovery: Prediction of CSF concentration in rodents for P-glycoprotein substrates and application to in vivo potency estimation. Biochem Pharmacol. 2013;85:1684–99.
Practice guidelines for the prevention, detection, and management of respiratory depression associated with neuraxial opioid administration: An updated report by the american society of anesthesiologists task force on neuraxial opioids and the american society of regional anesthesia and pain medicine. Anesthesiology. 2016; 124: 535–52.
Klimas R, Mikus G. Morphine-6-glucuronide is responsible for the analgesic effect after morphine administration: A quantitative review of morphine, morphine-6-glucuronide, and morphine-3-glucuronide. Br J Anaesth. 2014;113:935–44.
Meineke I, Freudenthaler S, Hofmann U, Schaeffeler E, Mikus G, Schwab M, et al. Pharmacokinetic modelling of morphine, morphine-3-glucuronide and morphine-6-glucuronide in plasma and cerebrospinal fluid of neurosurgical patients after short-term infusion of morphine. Br J Clin Pharmacol. 2002;54:592–603.
Sarton E, Olofsen E, Romberg R, den Hartigh J, Kest B, Nieuwenhuijs D, et al. Sex differences in morphine analgesia: An experimental study in healthy volunteers. Anesthesiology. 2000;93:1245–54.
Niesters M, Dahan A, Kest B, Zacny J, Stijnen T, Aarts L, et al. Do sex differences exist in opioid analgesia? A systematic review and meta-analysis of human experimental and clinical studies. Pain. 2010;151:61–8.
Badreldin N, Grobman WA, Yee LM. Racial disparities in postpartum pain management. Obstet Gynecol. 2019;134:1147–53.
Ofoegbu A, B Ettienne E. Pharmacogenomics and morphine. J Clin Pharmacol. 2021;61:1149–55.
Moren J, Francois T, Blanloeil Y, Pinaud M. The effects of a nonsteroidal antiinflammatory drug (ketoprofen) on morphine respiratory depression: A double-blind, randomized study in volunteers. Anesth Analg. 1997;85:400–5.
Dershwitz M, Walsh JL, Morishige RJ, Connors PM, Rubsamen RM, Shafer SL, et al. Pharmacokinetics and pharmacodynamics of inhaled versus intravenous morphine in healthy volunteers. Anesthesiology. 2000;93:619–28.
Westerling D, Persson C, Höglund P. Plasma concentrations of morphine, morphine-3-glucuronide, and morphine-6-glucuronide after intravenous and oral administration to healthy volunteers: Relationship to nonanalgesic actions. Ther Drug Monit. 1995;17:287–301.
Skarke C, Jarrar M, Erb K, Schmidt H, Geisslinger G, Lötsch J. Respiratory and miotic effects of morphine in healthy volunteers when P-glycoprotein is blocked by quinidine. Clin Pharmacol Ther. 2003;74:303–11.
Murthy BR, Pollack GM, Brouwer KL. Contribution of morphine-6-glucuronide to antinociception following intravenous administration of morphine to healthy volunteers. J Clin Pharmacol. 2002;42:569–76.
Meissner K, Avram MJ, Yermolenka V, Francis AM, Blood J, Kharasch ED. Cyclosporine-inhibitable blood-brain barrier drug transport influences clinical morphine pharmacodynamics. Anesthesiology. 2013;119:941–53.
Ederoth P, Tunblad K, Bouw R, Lundberg CJ, Ungerstedt U, Nordström CH, et al. Blood-brain barrier transport of morphine in patients with severe brain trauma. Br J Clin Pharmacol. 2004;57:427–35.
Bouw R, Ederoth P, Lundberg J, Ungerstedt U, Nordström CH, Hammarlund-Udenaes M. Increased blood-brain barrier permeability of morphine in a patient with severe brain lesions as determined by microdialysis. Acta Anaesthesiol Scand. 2001;45:390–2.
Lötsch J, Weiss M, Kobal G, Geisslinger G. Pharmacokinetics of morphine-6-glucuronide and its formation from morphine after intravenous administration. Clin Pharmacol Ther. 1998;63:629–39.
Hanna MH, Peat SJ, Knibb AA, Fung C. Disposition of morphine-6-glucuronide and morphine in healthy volunteers. Br J Anaesth. 1991;66:103–7.
Dale O, Thoner J, Nilsen T, Tveita T, Borchgrevink PC, Klepstad P. Serum and cerebrospinal fluid morphine pharmacokinetics after single doses of intravenous and intramuscular morphine after hip replacement surgery. Eur J Clin Pharmacol. 2007;63:837–42.
Sverrisdóttir E, Foster DJ, Upton RN, Olesen AE, Lund TM, Gabel-Jensen C, et al. Modelling concentration-analgesia relationships for morphine to evaluate experimental pain models. Eur J Pharm Sci. 2015;66:50–8.
Skarke C, Langer M, Jarrar M, Schmidt H, Geisslinger G, Lötsch J. Probenecid interacts with the pharmacokinetics of morphine-6-glucuronide in humans. Anesthesiology. 2004;101:1394–9.
Aitkenhead AR, Derbyshire DR, Pinnock CA, Achola K, Smith G. Pharmacokinetics of intravenous naloxone in healthy volunteers. Anesthesiology. 1984;61:A381.
McDonald R, Lorch U, Woodward J, Bosse B, Dooner H, Mundin G, et al. Pharmacokinetics of concentrated naloxone nasal spray for opioid overdose reversal: Phase-I healthy volunteer study. Addiction. 2018;113:484–93.
Knaggs RD, Crighton IM, Cobby TF, Fletcher AJP, Hobbs GJ. The pupillary effects of intravenous morphine, codeine, and tramadol in volunteers. Anesth Analg. 2004;99:108–12.
Miller CD, Asbury AJ, Brown JH. Pupillary effects of alfentanil and morphine. Br J Anaesth. 1990;65:415–7.
Lötsch J, Skarke C, Schmidt H, Grösch S, Geisslinger G. The transfer half-life of morphine-6-glucuronide from plasma to effect site assessed by pupil size measurement in healthy volunteers. Anesthesiology. 2001;95:1329–38.
Stoops WW, Hatton KW, Lofwall MR, Nuzzo PA, Walsh SL. Intravenous oxycodone, hydrocodone, and morphine in recreational opioid users: Abuse potential and relative potencies. Psychopharmacology (Berl). 2010;212:193–203.
Walker DJ, Zacny JP. Subjective, psychomotor, and analgesic effects of oral codeine and morphine in healthy volunteers. Psychopharmacology (Berl). 1998;140:191–201.
Kharasch ED, Hoffer C, Whittington D, Sheffels P. Role of P-glycoprotein in the intestinal absorption and clinical effects of morphine. Clin Pharmacol Ther. 2003;74:543–54.
Romberg R, Olofsen E, Sarton E, Teppema L, Dahan A. Pharmacodynamic effect of morphine-6-glucuronide versus morphine on hypoxic and hypercapnic breathing in healthy volunteers. Anesthesiology. 2003;99:788–98.
Bailey PL, Clark NJ, Pace NL, Isern M, Stanley TH. Failure of nalbuphine to antagonize morphine: A double-blind comparison with naloxone. Anesth Analg. 1986;65:605–11.
Thompson PI, Joel SP, John L, Wedzicha JA, Maclean M, Slevin ML. Respiratory depression following morphine and morphine-6-glucuronide in normal subjects. Br J Clin Pharmacol. 1995;40:145–52.
Gairola RL, Gupta PK, Pandley K. Antagonists of morphine-induced respiratory depression. A study in postoperative patients. Anaesthesia. 1980;35:17–21.
Romagnoli A, Keats AS. Ceiling effect for respiratory depression by nalbuphine. Clin Pharmacol Ther. 1980;27:478–85.
Motov S, Rockoff B, Cohen V, Pushkar I, Likourezos A, McKay C, et al. Intravenous subdissociative-dose ketamine versus morphine for analgesia in the emergency department: A randomized controlled trial. Ann Emerg Med. 2015;66:222–.e1.
Chang AK, Bijur PE, Meyer RH, Kenny MK, Solorzano C, Gallagher EJ. Safety and efficacy of hydromorphone as an analgesic alternative to morphine in acute pain: A randomized clinical trial. Ann Emerg Med. 2006;48:164–72.
Dahan A, Romberg R, Teppema L, Sarton E, Bijl H, Olofsen E. Simultaneous measurement and integrated analysis of analgesia and respiration after an intravenous morphine infusion. Anesthesiology. 2004;101:1201–9.
Skarke C, Darimont J, Schmidt H, Geisslinger G, Lötsch J. Analgesic effects of morphine and morphine-6-glucuronide in a transcutaneous electrical pain model in healthy volunteers. Clin Pharmacol Ther. 2003;73:107–21.
Penson RT, Joel SP, Bakhshi K, Clark SJ, Langford RM, Slevin ML. Randomized placebo-controlled trial of the activity of the morphine glucuronides. Clin Pharmacol Ther. 2000;68:667–76.
Romberg R, Olofsen E, Sarton E, den Hartigh J, Taschner PE, Dahan A. Pharmacokinetic-pharmacodynamic modeling of morphine-6-glucuronide-induced analgesia in healthy volunteers: Absence of sex differences. Anesthesiology. 2004;100:120–33.
Evans JM, Hogg MI, Lunn JN, Rosen M. Degree and duration of reversal by naloxone of effects of morphine in conscious subjects. Br Med J. 1974;2:589–91.
Olofsen E, van Dorp E, Teppema L, Aarts L, Smith TW, Dahan A, et al. Naloxone reversal of morphine- and morphine-6-glucuronide-induced respiratory depression in healthy volunteers: A mechanism-based pharmacokinetic-pharmacodynamic modeling study. Anesthesiology. 2010;112:1417–27.
Acknowledgements
This work was supported by the National Key Research and Development Program of China (Grant No. 2022YFC3300902).
Author information
Authors and Affiliations
Contributions
RJM and LL designed the research; RJM and XDL performed the research; RJM and TLL analyzed the data; RJM, and XDL wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mu, Rj., Liu, Tl., Liu, Xd. et al. PBPK-PD model for predicting morphine pharmacokinetics, CNS effects and naloxone antagonism in humans. Acta Pharmacol Sin (2024). https://doi.org/10.1038/s41401-024-01255-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41401-024-01255-2